History of the Procedure
The history of submandibular gland excision demonstrates two chronologic levels of observation and scientific reporting. First-level literature (published from the 1950s through the 1970s) made general comments related to submandibular gland tumors and non-neoplastic processes, with later literature (published from the 1980s to the present) commonly discussing specific morbidity of the submandibular gland excision. A description of pathologic processes of the major salivary glands was initially provided by McFarland in 1926 and later by the same author in 1933. This author’s observations focused exclusively on parotid gland neoplasms, owing to their much higher incidence, with no mention of the rare submandibular gland tumors. In these two initial reports, 135 tumors of the parotid gland were reviewed, and the author primarily commented on the outcome of surgery and nonsurgical therapy as a function of size of the parotid tumor. The author did not discuss the specific microscopic diagnosis in his review of these cases. Rather, he described the outcome of tumors smaller in size than a walnut (tumors that were the size of a bean, hazelnut, grape, marble, or almond), those of ordinary size between the size of a walnut and that of a lemon (those that were the size of a walnut, plum, egg, Seckel pear, or lemon), and those larger than a lemon (those that were the size of an apple, goose egg, orange, grapefruit, two fists, or a human head). Moreover, the author did not make comments regarding the specific technique of surgical treatment of the tumors of the parotid gland. Finally, McFarland indicated that it was not advisable to operate on parotid tumors when small and that the complications of facial nerve palsy, salivary fistula, and recurrence should be carefully considered for fear that more harm than good may be done.
In 1936, McFarland reported on 301 tumors of the major salivary glands, including 278 parotid tumors, 22 submandibular tumors, and 1 sublingual tumor. This paper represents the first mention of submandibular gland tumors. As in his 1933 publication, the author offered no specific comments regarding surgical technique, including that for submandibular gland tumors. Nonetheless, he indicated that 8 of the 22 submandibular gland tumors recurred. It was not until 1953 that Foote and Frazell provided a specific assessment of the histologic diagnosis of major salivary gland tumors. A total of 877 major salivary gland tumors were analyzed, of which 107 were located in the submandibular gland. These included 47 benign mixed tumors, 11 malignant mixed tumors, 17 adenoid cystic carcinomas, and 8 mucoepidermoid carcinomas, among others. In fact, this paper was written as a clinicopathologic review of tumors of the major salivary glands, again without specific mention of the technical aspects of the surgery performed to remove these tumors.
It was not until 1966 that Work introduced comments regarding the surgical excision of major salivary glands associated with benign and malignant neoplastic diagnoses. In the case of parotid tumors, the author advised against enucleation procedures and reported that parotidectomy was infrequently combined with elective prophylactic neck dissection in cases of primary parotid malignant disease. Nonetheless, he recommended prophylactic neck dissection in the case of a primary submandibular gland malignancy. In 1966, Work and Gates reviewed the treatment of non-neoplastic diseases of the major salivary glands. Transcutaneous excision of the submandibular gland was recommended in the case of a sialolith located within or near the submandibular gland. In addition, the authors recommended submandibular gland excision in the case of severe injury to the gland and duct.
In 1967, Work recapitulated comments regarding surgery for neoplastic and non-neoplastic disorders of the major salivary glands. For parotid neoplasia, the author recommended a facial nerve–preserving parotidectomy, and for submandibular gland tumors, he recommended an excision of the tumor and gland. The largest initial series of submandibular gland tumors was published by Eneroth and Hjertman in 1967; they reviewed 187 cases of tumors of the submandibular gland, of which 125 were benign and 62 were malignant. Of the benign tumors, 95 were mixed tumors. Treatment for these benign mixed tumors consisted of excising the tumor in 50 cases, and evacuating the submandibular region in 45 cases, including 4 patients who underwent radical neck dissection. Forty-one of these 95 patients also underwent preoperative or postoperative radiation therapy. Five of these patients accounted for 18 recurrences related to surgery/radiation therapy for these benign mixed tumors. In 1968, Seward published three papers on the topic of anatomic surgery for non-neoplastic processes of the major salivary glands. These included salivary calculi that addressed the symptoms, signs, and differential diagnosis ; calculi in the anterior part of the submandibular duct ; and calculi in the posterior part of the submandibular duct. Although these papers reviewed surgical principles, they were described exclusively in relation to the salivary ducts rather than to the surgical excision of the submandibular gland. Finally, Rafla reported on 35 submandibular gland tumors in 1970. This report commented on 13 benign tumors and 22 malignant tumors, of which 3 were metastatic tumors. Enucleation of benign submandibular gland tumors was performed in 3 cases, yet the author did not criticize this technique.
Second-level literature related to submandibular gland excision first appeared in the 1980s and has largely centered on clinical outcomes. Specific complications related to the submandibular gland excision for benign disease are discussed in the avoidance and management of intraoperative complications section of this chapter.
History of the Procedure
The history of submandibular gland excision demonstrates two chronologic levels of observation and scientific reporting. First-level literature (published from the 1950s through the 1970s) made general comments related to submandibular gland tumors and non-neoplastic processes, with later literature (published from the 1980s to the present) commonly discussing specific morbidity of the submandibular gland excision. A description of pathologic processes of the major salivary glands was initially provided by McFarland in 1926 and later by the same author in 1933. This author’s observations focused exclusively on parotid gland neoplasms, owing to their much higher incidence, with no mention of the rare submandibular gland tumors. In these two initial reports, 135 tumors of the parotid gland were reviewed, and the author primarily commented on the outcome of surgery and nonsurgical therapy as a function of size of the parotid tumor. The author did not discuss the specific microscopic diagnosis in his review of these cases. Rather, he described the outcome of tumors smaller in size than a walnut (tumors that were the size of a bean, hazelnut, grape, marble, or almond), those of ordinary size between the size of a walnut and that of a lemon (those that were the size of a walnut, plum, egg, Seckel pear, or lemon), and those larger than a lemon (those that were the size of an apple, goose egg, orange, grapefruit, two fists, or a human head). Moreover, the author did not make comments regarding the specific technique of surgical treatment of the tumors of the parotid gland. Finally, McFarland indicated that it was not advisable to operate on parotid tumors when small and that the complications of facial nerve palsy, salivary fistula, and recurrence should be carefully considered for fear that more harm than good may be done.
In 1936, McFarland reported on 301 tumors of the major salivary glands, including 278 parotid tumors, 22 submandibular tumors, and 1 sublingual tumor. This paper represents the first mention of submandibular gland tumors. As in his 1933 publication, the author offered no specific comments regarding surgical technique, including that for submandibular gland tumors. Nonetheless, he indicated that 8 of the 22 submandibular gland tumors recurred. It was not until 1953 that Foote and Frazell provided a specific assessment of the histologic diagnosis of major salivary gland tumors. A total of 877 major salivary gland tumors were analyzed, of which 107 were located in the submandibular gland. These included 47 benign mixed tumors, 11 malignant mixed tumors, 17 adenoid cystic carcinomas, and 8 mucoepidermoid carcinomas, among others. In fact, this paper was written as a clinicopathologic review of tumors of the major salivary glands, again without specific mention of the technical aspects of the surgery performed to remove these tumors.
It was not until 1966 that Work introduced comments regarding the surgical excision of major salivary glands associated with benign and malignant neoplastic diagnoses. In the case of parotid tumors, the author advised against enucleation procedures and reported that parotidectomy was infrequently combined with elective prophylactic neck dissection in cases of primary parotid malignant disease. Nonetheless, he recommended prophylactic neck dissection in the case of a primary submandibular gland malignancy. In 1966, Work and Gates reviewed the treatment of non-neoplastic diseases of the major salivary glands. Transcutaneous excision of the submandibular gland was recommended in the case of a sialolith located within or near the submandibular gland. In addition, the authors recommended submandibular gland excision in the case of severe injury to the gland and duct.
In 1967, Work recapitulated comments regarding surgery for neoplastic and non-neoplastic disorders of the major salivary glands. For parotid neoplasia, the author recommended a facial nerve–preserving parotidectomy, and for submandibular gland tumors, he recommended an excision of the tumor and gland. The largest initial series of submandibular gland tumors was published by Eneroth and Hjertman in 1967; they reviewed 187 cases of tumors of the submandibular gland, of which 125 were benign and 62 were malignant. Of the benign tumors, 95 were mixed tumors. Treatment for these benign mixed tumors consisted of excising the tumor in 50 cases, and evacuating the submandibular region in 45 cases, including 4 patients who underwent radical neck dissection. Forty-one of these 95 patients also underwent preoperative or postoperative radiation therapy. Five of these patients accounted for 18 recurrences related to surgery/radiation therapy for these benign mixed tumors. In 1968, Seward published three papers on the topic of anatomic surgery for non-neoplastic processes of the major salivary glands. These included salivary calculi that addressed the symptoms, signs, and differential diagnosis ; calculi in the anterior part of the submandibular duct ; and calculi in the posterior part of the submandibular duct. Although these papers reviewed surgical principles, they were described exclusively in relation to the salivary ducts rather than to the surgical excision of the submandibular gland. Finally, Rafla reported on 35 submandibular gland tumors in 1970. This report commented on 13 benign tumors and 22 malignant tumors, of which 3 were metastatic tumors. Enucleation of benign submandibular gland tumors was performed in 3 cases, yet the author did not criticize this technique.
Second-level literature related to submandibular gland excision first appeared in the 1980s and has largely centered on clinical outcomes. Specific complications related to the submandibular gland excision for benign disease are discussed in the avoidance and management of intraoperative complications section of this chapter.
Indications for the Use of the Procedure
Sialadenitis of the Submandibular Gland
Sialadenitis, a generic term referring to salivary gland inflammation and infection, is a fairly common affliction of the submandibular gland. There are numerous etiologies of submandibular sialadenitis, including bacterial, viral, fungal, mycobacterial, parasitic, and immunologic causes that may occur in the acute or chronic settings. The diagnosis of sialadenitis is made based on a thorough medical history, physical examination, and imaging studies. A number of modifiable, nonmodifiable, or relatively nonmodifiable predisposing factors can result in sialadenitis. In particular, dehydration with or without recent surgery and anesthesia, the presence of a sialolith in the intraglandular or extraglandular ducts of the submandibular gland, and medications with known anticholinergic properties are of significance in the development of submandibular sialadenitis.
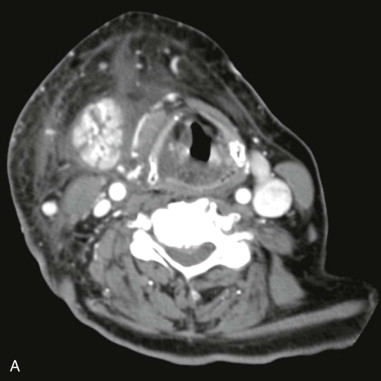
Acute bacterial submandibular sialadenitis (ABSS) is a community-acquired disease that is most commonly diagnosed in association with a sialolith. The diagnosis of ABSS is less frequently associated with dehydration and an in-patient admission to the hospital than occurs with acute bacterial parotitis. The history and clinical presentation of ABSS includes submandibular swelling and pain that commonly occur in relation to eating. The presence of an enlarged submandibular gland should primarily suggest sialadenitis, with a neoplasm considered a remote second diagnosis. The presence of pus may be noted at the opening of Wharton’s duct in the floor of mouth, under which circumstances the diagnosis of ABSS is made rapidly. The most common cause of ABSS is obstruction of Wharton’s duct, typically from a sialolith, such that obtaining a panoramic radiograph is of paramount importance in the initial workup of a patient with a clinical diagnosis of submandibular sialadenitis. The use of computed tomography (CT) scans in patients with ABSS is indicated when complicated sialadenitis is diagnosed as noted by a febrile and toxic patient, when an abscess requiring drainage is suspected, or when initial management does not resolve the infection ( Figure 87-1, A and B ). The management of ABSS is initially medical, including the use of empiric antistaphylococcal/antistreptococcal antibiotics, hydration, massage of the affected submandibular gland, heat, and sourball candies (sialogogues) so as to stimulate obstructed salivary flow. A sialolith located in the extraglandular duct should be removed if possible when it is identified. More aggressive therapy is rarely required, and the compliant patient only rarely requires submandibular gland excision for a diagnosis of ABSS.
Chronic recurrent submandibular sialadenitis is usually the result of ineffective treatment of ABSS due to a noncompliant patient, the presence of a previously undiagnosed sialolith, or the presence of unrecognized or untreated chronic sialadenitis at the time of the initial evaluation. Chronic recurrent submandibular sialadenitis occurs more frequently than chronic bacterial parotitis. Under such circumstances, patients usually report symptoms of submandibular postprandial pain and swelling lasting longer than a month. Physical examination typically demonstrates an indurated gland that may be smaller than the unaffected contralateral submandibular gland due to scar contracture. This firm swelling of the submandibular gland affected by chronic inflammation has occasionally been referred to as a Kuttner tumor, as this chronic inflammatory state can be difficult to distinguish from neoplastic disease based on physical examination alone. Initial medical management is instituted similarly to that for ABSS, but most patients with chronic sialadenitis ultimately require submandibular gland excision.
Sialolithiasis of the Submandibular Gland
Submandibular sialolithiasis is not an uncommon diagnosis, with postmortem studies suggesting the prevalence of salivary calculi in 1% to 2% of cases. Sialolithiasis is the most common cause of salivary gland obstruction and occurs primarily in the submandibular gland (80% to 90%), with only 5% to 10% of sialoliths occurring in the parotid gland. It has been estimated to represent more than 50% of major salivary gland diseases and is the most common cause of acute and chronic salivary gland infections. Some consider sialolithiasis to be a consequence as well as a cause of sialadenitis. For example, the presence of a sialolith may result in obstruction of salivary flow, thereby predisposing the submandibular gland to retrograde infection. In addition, the presence of sialadenitis may change the characteristics of the saliva, thereby favoring the deposition of calcium with the development of a sialolith.
Clinically, in a series of 245 patients with sialolithiasis, 94.3% of cases were diagnosed in the submandibular gland system, with the remaining stones located primarily in the parotid gland. Distribution between right and left submandibular gland stones was nearly equal, and only about 1% of submandibular stones had bilateral involvement. A discussion of sialolithiasis, therefore, centers nearly exclusively on the submandibular gland. Swelling was present in 94% of patients, pain in 65.2%, pus secretion in 15.5%, fever in 6%, and 2.4% of patients in this series were asymptomatic. Radiographically, approximately 80% of submandibular sialoliths are radioopaque and able to be identified radiographically, compared to 60% of parotid sialoliths being radioopaque. A majority of submandibular sialoliths are single in nature compared with parotid sialoliths, which more commonly occur as multiple stones. Pathophysiologically, it has been suggested that the bend or genu in the submandibular duct may be an etiologic factor in the formation of salivary stones because this bend may encourage stagnation of saliva. The submandibular duct emerges from the superficial aspect of the gland and passes over the free posterior margin of the mylohyoid muscle. It courses forward and slightly superiorly on the mylohyoid before opening at the sublingual papilla.
Drage and colleagues investigated the genu of the submandibular duct to determine if its angle was of significance in the development of submandibular sialadenitis and sialolithiasis. One hundred and two sialograms were analyzed from three groups of patients, including 18 normal patients, 61 patients with salivary calculi, and 23 patients with sialadenitis. Their study concluded that there is a wide variation in the angle of the genu of the submandibular duct in the sagittal plane in normal glands and in disease that does not appear to be associated with either sialadenitis or sialolithiasis. The length of the submandibular duct, the dependent anatomic position of the submandibular gland, and the alkaline nature of saliva along with its relatively high viscosity and high content of calcium salts probably account for the higher incidence of sialolithiasis of the submandibular gland compared to the other salivary glands. The components of salivary stones were once believed to include desquamated epithelial cells, foreign bodies, mucous plugs, and microorganisms. In 2004, Kasaboglu and colleagues studied the chemical composition and micromorphology of sialoliths using radiograph diffraction analysis and scanning electron microscopy. In six examples of sialoliths, only hydroxyapatite crystals were identified without signs of foreign bodies or microorganisms identified at the core of the sialolith.
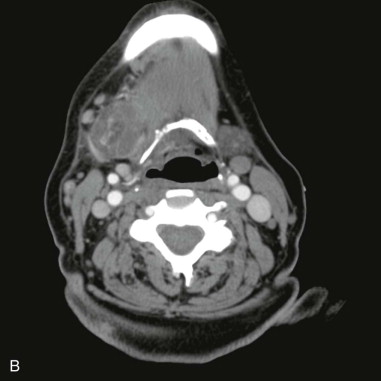
In general terms, the treatment of submandibular sialolithiasis is a function of the size and location of the sialolith. Transoral sialolithotomy is the preferable procedure for submandibular sialolithiasis provided that the sialolith can be palpated on transoral examination. This is particularly the case since increasing evidence exists to show that the submandibular gland regains function after stone removal. As such, submandibular gland excision is generally reserved for cases of submandibular sialolithiasis where the stone is noted radiographically to exist within the gland or its hilum where transoral retrieval of the stone is not possible. Preoperative imaging is indicated so as to provide precise localization of the stone or stones ( Figure 87-2 ).


Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


