Armamentarium
|
History of the Procedure
Correction of soft tissue and bony defects has proven to be some of the most challenging tasks for the reconstructive surgeon. The use of tissue flaps has become a common technique in reconstructive surgery due to their demonstrated success. Flaps have been documented as far back as 600 bc , when an Indian hermit, Sushrutha, reconstructed the nose with a forehead flap, a technique that continues to be used to this day. However, it wasn’t until the late nineteenth century, when Golovine and Lentz performed reconstructions on an eviscerated orbital defect and a resected condylar neck, respectively, that the first descriptions of the temporalis flap were documented. This type of flap also was used in early reconstructive efforts on the temporomandibular joint, as a portion of the temporalis muscle was attached to the temporalis fascia. In 1948, Campbell described the use of the temporalis flap in the reconstruction of a left maxillary defect, and nearly 10 years later, the same flap was used in middle ear and mastoid cavities.
Later years saw the anatomic boundaries expanded by Bakamjian and Horton, who used the flap to reconstruct the palate and maxilla after tumor resection. Nevertheless, reconstruction of exenterated orbital defects remained the primary use for most surgeons, as demonstrated by a study by Tessier and Krastinova. They described 14 cases in which the flap was transposed through the lateral orbital wall, preserving the eyelids. Further developments, combined with a better understanding of the anatomic site, allowed surgeons to carry the flap to defects that once seemed too far to reconstruct.
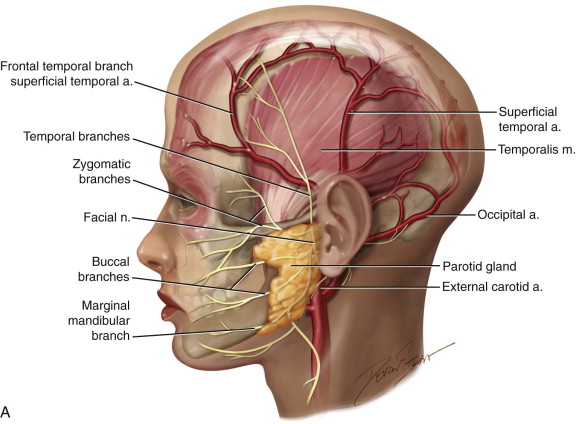
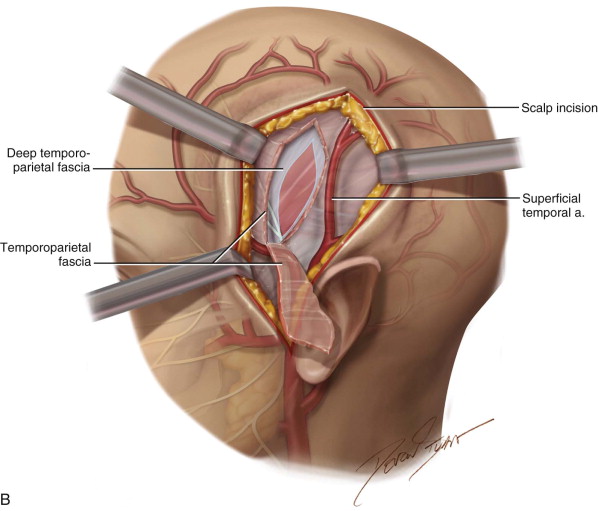
Over the past few decades, the temporalis flap has been used in a myriad of reconstructive efforts for the orbit, eyelids, cranial base, maxilla and palate, and mandible. This flap even found a use in the treatment of craniofacial deformities, such as Treacher Collins syndrome, after van der Meulen et al. modified the technique proposed by McCarthy and Zide. The temple region is an appropriate donor site because it has a copious vascular supply and several layers of tissue, which provide it with the versatility seen surgically. The advantages of this flap have been demonstrated in previous studies, and its popularity continues to increase, along with its evolution. With its robust blood supply and proven versatility, the temporalis flap has shown staying power as a treatment for more than 2,000 years, which can be attributed to its reliability, ability to cover many areas in the maxillofacial region.
History of the Procedure
Correction of soft tissue and bony defects has proven to be some of the most challenging tasks for the reconstructive surgeon. The use of tissue flaps has become a common technique in reconstructive surgery due to their demonstrated success. Flaps have been documented as far back as 600 bc , when an Indian hermit, Sushrutha, reconstructed the nose with a forehead flap, a technique that continues to be used to this day. However, it wasn’t until the late nineteenth century, when Golovine and Lentz performed reconstructions on an eviscerated orbital defect and a resected condylar neck, respectively, that the first descriptions of the temporalis flap were documented. This type of flap also was used in early reconstructive efforts on the temporomandibular joint, as a portion of the temporalis muscle was attached to the temporalis fascia. In 1948, Campbell described the use of the temporalis flap in the reconstruction of a left maxillary defect, and nearly 10 years later, the same flap was used in middle ear and mastoid cavities.
Later years saw the anatomic boundaries expanded by Bakamjian and Horton, who used the flap to reconstruct the palate and maxilla after tumor resection. Nevertheless, reconstruction of exenterated orbital defects remained the primary use for most surgeons, as demonstrated by a study by Tessier and Krastinova. They described 14 cases in which the flap was transposed through the lateral orbital wall, preserving the eyelids. Further developments, combined with a better understanding of the anatomic site, allowed surgeons to carry the flap to defects that once seemed too far to reconstruct.
Over the past few decades, the temporalis flap has been used in a myriad of reconstructive efforts for the orbit, eyelids, cranial base, maxilla and palate, and mandible. This flap even found a use in the treatment of craniofacial deformities, such as Treacher Collins syndrome, after van der Meulen et al. modified the technique proposed by McCarthy and Zide. The temple region is an appropriate donor site because it has a copious vascular supply and several layers of tissue, which provide it with the versatility seen surgically. The advantages of this flap have been demonstrated in previous studies, and its popularity continues to increase, along with its evolution. With its robust blood supply and proven versatility, the temporalis flap has shown staying power as a treatment for more than 2,000 years, which can be attributed to its reliability, ability to cover many areas in the maxillofacial region.
Indications for the Use of the Procedure
The goals of maxillofacial reconstruction should focus on accurately reproducing the original form, providing the patient with appropriate esthetics, and restoring functional needs.
The vascular supply of the temporalis muscle is from the temporal artery, one of two terminal branches of the external carotid artery. The temporal artery divides into three primary arteries: the anterior deep temporal artery (ADTA), the posterior deep temporal artery (PDTA), and the middle temporal artery (MTA). Each primary artery branches into secondary arterioles and then into the terminal arterioles. In the coronal plane, the vessels were located mainly on the lateral and medial aspects of the muscle, with a significantly lower vascular density in the midline ( Figure 110-1 ). The versatility of the temporalis muscle flap enables surgeons to accomplish multiple tasks, whether the defect is traumatic, pathologic, or developmental in origin.
In cases of extensive en bloc resection of the maxilla, orbits, and cranial base, in which communication with the anterior skull base occurs, the temporalis muscle flap can provide appropriate coverage and a watertight seal. The flap is also used in the reconstruction of oral-mandibular defects and temporomandibular joint (TMJ) ankylosis, the reconstruction of palatal defects in cleft patients, and even in reanimation of total unilateral facial paralysis. The temporalis flap also is ideal for other maxillofacial defects of the cheek and palate caused by pathologic lesions, such as ameloblastoma, myxoma, and giant cell tumor. In the field of dentistry, it can be used as a soft tissue bed for later placement of bone grafts and implants, with epithelialization taking approximately 4 to 6 weeks to complete. Nevertheless, its popularity is largely due to its ability to resurface enormous defects of the orbital region, particularly the orbit. Donor site esthetics often is acceptable to patients and also provides great flexibility and versatility. Additionally, compared to other flaps, the temporalis flap is less bulky, more malleable, originates in a relatively hairless region, and is in close proximity to the oral cavity and other potential donor areas.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


