The oral and maxillofacial surgeon must have a firm grasp of facial anatomy and the surgical implications of the location and orientation of anatomic structures. This knowledge guides the surgeon in the planning of surgical approaches and in reconstruction of traumatic or surgical defects.
The visceral cranium is the lower portion of the head that facilitates the visceral functions, including breathing, smelling, speaking, tasting, and swallowing. In this discussion, the anatomy of the region is addressed in a manner similar to a surgical approach, from superficial to deep, with assessment of clinical points of interest as they relate to surgical access to the face.
The Skin
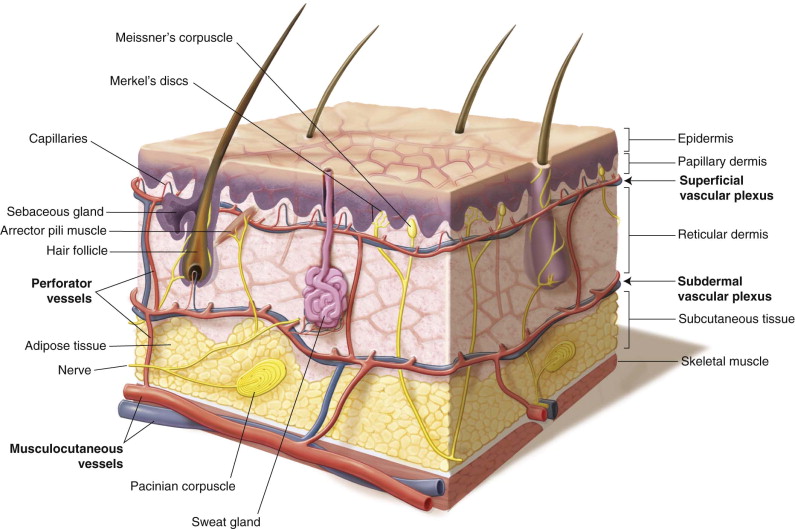
The skin is a complex organ, composed of superficial epidermis and underlying dermis, that provides sensation and protection. The anatomic and physiologic properties of the skin play an important role in the final esthetics of any facial surgical procedure ( Figure 5-1 ).
Gonzalez-Ulloa et al. first described 14 distinct facial esthetic units where the skin throughout has a uniform color, texture, thickness, and mobility. Burget and Menick expounded upon this concept. The relaxed skin tension lines (RSTLs) of the face generally provide excellent camouflage of incisions placed within or parallel to them. The lines of maximum extensibility are generally perpendicular to the relaxed skin tension lines. Surgical approaches to the face should attempt to place incisions at the borders of facial subunits and parallel to relaxed skin tension lines to minimize the effect of the final scar ( Figure 5-2 ).
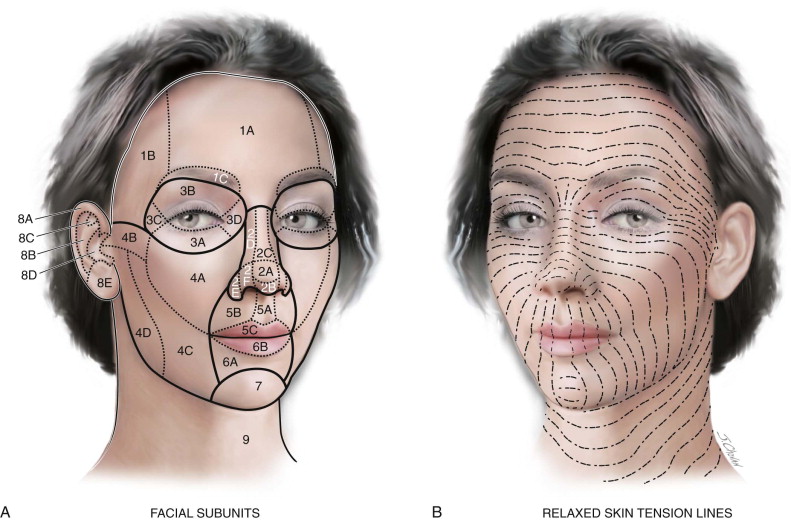
The thickness and character of facial skin is also important when considering skin matches for reconstruction. For example, the skin of the nasal dorsum is nearly 3.3 times the thickness of the upper eyelid skin. The skin of the face is also densely populated with pilosebaceous units, particularly in the forehead, nose, and chin (an area sometimes referred to as the T-zone), with a progressive decrease toward the lateral edges of the face. This should be taken into consideration when planning skin resurfacing procedures that rely on the pilosebaceous units for reepithelialization.
The Fat Pads of the Face
The malar fat pad is a triangular structure superficial to the superficial musculoaponeurotic system (SMAS) and mimetic muscles. It is oriented with its base along the nasolabial fold and its apex at the zygomatic prominence. This structure descends and loses volume with age, resulting in the descent of the facial soft tissues associated with aging.
The buccal fat pad is an important structure within the cheek. It has a central body and four processes: the buccal, pterygoid, pterygopalatine, and temporal (superficial and deep) processes. The zygomatic and buccal branches of the facial nerve lie superficial to the buccal process, with the parotid duct running within it. Care should be taken when excising a portion of the buccal fat pad for cosmetic purposes or when using a pedicled buccal fat flap for oral-antral fistula closure.
Multiple other distinct fat pads have been described and should be taken into account, particularly when fat is injected as an adjunct to cosmetic surgery.
The Fat Pads of the Face
The malar fat pad is a triangular structure superficial to the superficial musculoaponeurotic system (SMAS) and mimetic muscles. It is oriented with its base along the nasolabial fold and its apex at the zygomatic prominence. This structure descends and loses volume with age, resulting in the descent of the facial soft tissues associated with aging.
The buccal fat pad is an important structure within the cheek. It has a central body and four processes: the buccal, pterygoid, pterygopalatine, and temporal (superficial and deep) processes. The zygomatic and buccal branches of the facial nerve lie superficial to the buccal process, with the parotid duct running within it. Care should be taken when excising a portion of the buccal fat pad for cosmetic purposes or when using a pedicled buccal fat flap for oral-antral fistula closure.
Multiple other distinct fat pads have been described and should be taken into account, particularly when fat is injected as an adjunct to cosmetic surgery.
The Superficial Musculoaponeurotic System
An understanding of the superficial musculoaponeurotic system (SMAS) is fundamental to the facial surgeon because of the orientation of the SMAS and the neurovascular structures of the face. The territorial distribution and details of the SMAS continue to be controversial; however, an understanding of the general principles and anatomic descriptions allows surgeons to draw their own conclusions.
The SMAS is a fanlike fibromuscular layer that encases the muscles of facial expression, similar to the superficial cervical fascia of the neck that encases the platysma in the neck. The SMAS connects the dermis to the underlying facial muscles by a three-dimensional architecture of collagen, elastic fibers, fat cells, and muscle fibers ( Figure 5-3 ).
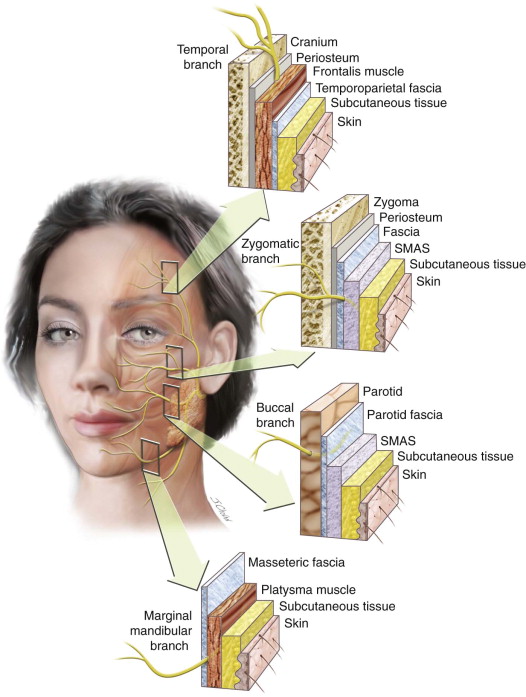
The SMAS is continuous with the superficial temporal (temporoparietal) fascia superiorly and with the superficial cervical fascia of the platysma inferiorly. It lies superficial to the parotidomasseteric fascia. Anteriorly the SMAS can be extended to the approximate point of the facial artery and vein; however, it is of primary surgical relevance in the region overlying the parotid. Anterior to the nasolabial fold, the innervation of the perioral musculature becomes more susceptible to injury as the SMAS becomes more fibrous and divides to form an investing fascia of the zygomaticus muscles.
The Facial Layers of the Face: Regional Considerations
In the upper face, when elevating a coronal or forehead flap, dissection in the avascular plane between the periosteum and temporoparietal fascia protects the temporal branch of the facial nerve. During this dissection, it is important to note that the vessels and sensory nerves exit the bone via their various foramina and penetrate the layer being elevated; therefore, care must be taken in these areas.
In the temporal region, dissection should proceed deep to the superficial layer of the deep temporal fascia, within the temporal fat pad, to ensure that the temporal branch is sufficiently protected and elevated within the superficial temporal (temporoparietal) fascia.
The Facial Musculature
Six major muscle groups in the head assist with visceral functions: orbital muscles, masticatory muscles, muscles of facial expression, tongue muscles, pharynx muscles, and larynx muscles. This chapter focuses on the masticatory muscles, mimetic muscles (muscles of facial expression), and tongue muscles.
Masticatory Muscles
The muscles of mastication are derived from the first branchial arch and are innervated by the mandibular division of cranial nerve (CN) V ( Figure 5-4 and Table 5-1 ).

| Muscle | Action | Innervation: CN V-3 |
|---|---|---|
| Masseter | Bilateral: Elevates and protrudes the mandible | Masseteric nerve |
| Temporalis | Bilateral: Elevates the mandible (vertical fibers) Bilateral: Retracts protruded mandible (horizontal fibers) |
Deep temporal nerves |
| Medial pterygoid | Bilateral: Elevates the mandible | Medial pterygoid nerve |
| Lateral pterygoid | Bilateral: Initiates mouth opening, protrudes mandible, and moves articular disk forward Unilateral: Lateral movement while chewing |
Lateral pterygoid nerve |
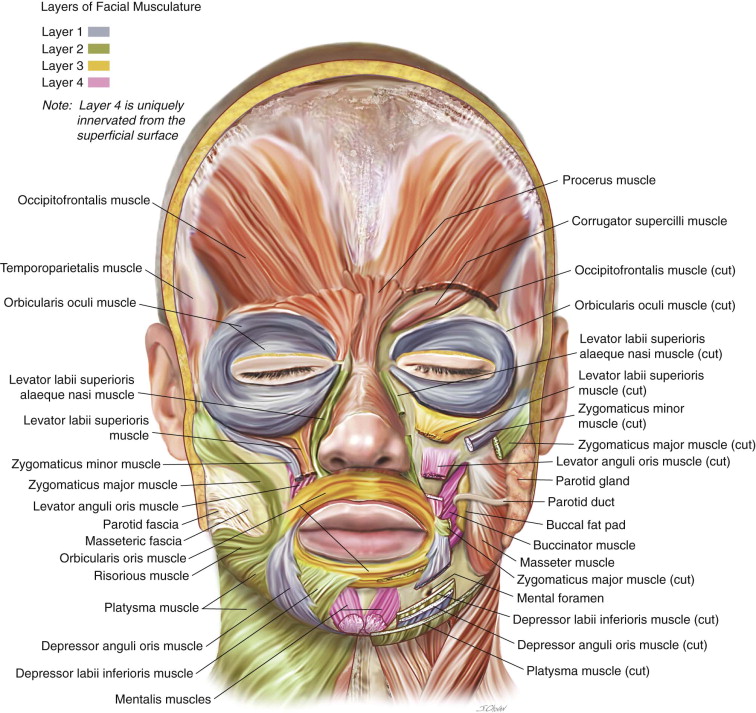
Superficial Facial Musculature
The muscles of facial expression are superficial muscles that are innervated by branches of the facial nerve (CN VII); they are composed of the orbicularis oris and 23 paired muscles. Some have suggested that there are four layers of facial muscles; layer four is unique because these muscles are innervated from their superficial surface, whereas the muscles in layers one through three receive innervation from their deep surfaces ( Table 5-2 ).
| Layer 1 | Depressor anguli oris, zygomaticus minor, orbicularis oculi |
| Layer 2 | Depressor labii inferioris, risorius, platysma, zygomaticus major, levator labii superioris alaeque nasi |
| Layer 3 | Orbicularis oris, levator labii superioris |
| Layer 4 | Mentalis, levator anguli oris, buccinator |
Table 5-3 lists the muscles of facial expression with their general actions. An understanding of the general and more specific actions of the facial musculature can be helpful in the diagnosis of facial nerve deficits and in selective chemical denervation for esthetic purposes.
| Muscle | Innervation | General Action |
|---|---|---|
| Occipitofrontalis | Temporal | Elevates eyebrows, wrinkles forehead |
| Corrugator supercilii | Temporal | Eyebrows medial and down, squint |
| Procerus | Temporal/zygomatic | Eyebrows medial and down, frown |
| Orbicularis oculi | Temporal/zygomatic | Closes eyelid, contracts skin around eye |
| Zygomaticus major | Zygomatic/buccal | Elevates corner of mouth |
| Zygomaticus minor | Zygomatic/buccal | Elevates upper lip |
| Levator labii superioris | Zygomatic/buccal | Elevates upper lip and nasolabial fold |
| Levator labii superioris alaeque nasi | Zygomatic/buccal | Elevates upper lip, flares nostril |
| Risorius | Buccal | Pulls corner of mouth laterally, smile |
| Buccinator | Buccal | Pulls cheek against teeth, pulls cheeks from side to side |
| Levator anguli oris | Buccal | Pulls angle of mouth up and medially, deepens nasolabial fold |
| Orbicularis oris | Buccal | Closes and compresses lips |
| Nasalis | Buccal | Transverse: Compresses nostril Alar: Flares nostril |
| Depressor anguli oris | Buccal/marginal mandibular | Pulls corner of mouth down |
| Depressor labii inferioris | Marginal mandibular | Pulls down lower lip |
| Mentalis | Marginal mandibular | Elevates and protrudes lower lip, drinking |
| Platysma | Cervical | Depresses and wrinkles skin of lower face, mouth, and neck |
The buccinator muscle plays an important role in bolus formation and bolus control by pressing the cheek against the teeth during mastication.
Musculature of the Tongue
The musculature of the tongue is composed of four intrinsic and four extrinsic muscles ( Figure 5-5 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


