Armamentarium
|
History of the Procedure
The canine is not only a critical tooth in determining facial esthetics and dental occlusion, but it also affects the course of orthodontic treatment when there is a disturbance in its eruption and alignment. The maxillary canine is usually expected to erupt before 13.9 years of age for girls and before 14.6 years for boys. It has been cited as the most frequently impacted tooth after third molars, and maxillary canine impaction is significantly more common than mandibular canine impaction. This chapter describes techniques related to maxillary canine impactions; however, the reader should keep in mind that these techniques can be applied to mandibular canines and to other impacted teeth when indicated.
In maxillary canine impaction, the position of the tooth is most often palatal, with a ratio of 2 : 1. The maxillary canine travels almost 22 mm during the time of eruption, and it moves in a palatal direction before it begins its buccal descent. The tooth’s long and tortuous eruption path from between the maxillary sinus and orbit to the occlusal plane makes it more prone to disturbances in its path. The etiology of maxillary canine impactions traditionally has been attributed to tooth mass/arch space insufficiency in buccal impactions, whereas palatal eruption and impaction are more likely to occur secondary to early eruption of the maxillary lateral incisor, which deviates the path of maxillary canine eruption. A genetic component also has been suggested in palatal impactions. Treatment planning decisions historically included extraction, observation, removal of the overretained deciduous precursor, exposure, or forced orthodontic eruption. Treatment planning should be based on multidisciplinary planning and communication between the orthodontist and surgical specialist.
Historically, a variety of tools and methods have been described for surgical repositioning of impacted maxillary canines. Most of these have fallen out of favor due to moderately high failure rates and the development of modern adhesive materials. Examples include:
- •
Celluloid crown
- •
Packing the wound area to maintain exposure
- •
Pins
- •
Orthodontic band/bracket
- •
Wire ligature
History of the Procedure
The canine is not only a critical tooth in determining facial esthetics and dental occlusion, but it also affects the course of orthodontic treatment when there is a disturbance in its eruption and alignment. The maxillary canine is usually expected to erupt before 13.9 years of age for girls and before 14.6 years for boys. It has been cited as the most frequently impacted tooth after third molars, and maxillary canine impaction is significantly more common than mandibular canine impaction. This chapter describes techniques related to maxillary canine impactions; however, the reader should keep in mind that these techniques can be applied to mandibular canines and to other impacted teeth when indicated.
In maxillary canine impaction, the position of the tooth is most often palatal, with a ratio of 2 : 1. The maxillary canine travels almost 22 mm during the time of eruption, and it moves in a palatal direction before it begins its buccal descent. The tooth’s long and tortuous eruption path from between the maxillary sinus and orbit to the occlusal plane makes it more prone to disturbances in its path. The etiology of maxillary canine impactions traditionally has been attributed to tooth mass/arch space insufficiency in buccal impactions, whereas palatal eruption and impaction are more likely to occur secondary to early eruption of the maxillary lateral incisor, which deviates the path of maxillary canine eruption. A genetic component also has been suggested in palatal impactions. Treatment planning decisions historically included extraction, observation, removal of the overretained deciduous precursor, exposure, or forced orthodontic eruption. Treatment planning should be based on multidisciplinary planning and communication between the orthodontist and surgical specialist.
Historically, a variety of tools and methods have been described for surgical repositioning of impacted maxillary canines. Most of these have fallen out of favor due to moderately high failure rates and the development of modern adhesive materials. Examples include:
- •
Celluloid crown
- •
Packing the wound area to maintain exposure
- •
Pins
- •
Orthodontic band/bracket
- •
Wire ligature
Indications for the Use of the Procedure
Impaction/noneruption of the maxillary canine is the chief indication for surgical exposure, but surgery is not the only treatment modality. Consideration should be given to prevention of impaction with early interceptive treatment, including extraction of the deciduous canine. This has been shown to allow eruption of its permanent successor.
Signs of impaction of the maxillary canine, according to Bishara, are:
- •
Delayed eruption of the permanent canine
- •
Overretained deciduous canine (after age 14 to 15 years)
- •
Absence of a normal labial canine bulge along the alveolar ridge
- •
Presence of a bulge on the palatal side of the alveolus
- •
Distal tipping of the lateral incisor
According to Ericson and Kurol, a canine bulge is seen in only 29% of children at 10 years of age; therefore, clinical absence of a bulge should not be considered pathognomonic for impaction. The clinical examination should be substantiated by a radiographic evaluation, which also helps localize the tooth’s position. Localization of the impacted tooth is critical in planning the surgical access and type of procedure.
Clinical Examination
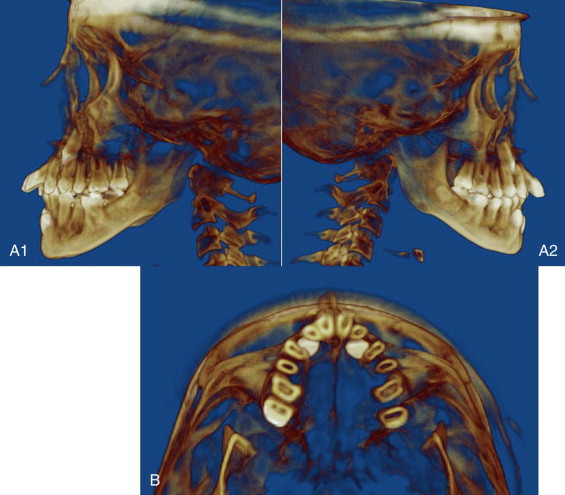
The first step in localization is clinical evaluation, including visual inspection and digital palpation for the presence or absence of any buccal or palatal bulges, retained primary canines, and tipping of adjacent teeth ( Figure 12-1, A ).

Radiographic Examination
Although routinely performed, radiographic assessment is especially helpful when no clinical signs of localization of an impacted tooth are noted. Radiologic diagnostic methods for impacted canines can be classified into intraoral exams and extraoral exams.
Intraoral Radiographic Examination.
A traditional intraoral radiographic technique involves obtaining two periapical films with varying horizontal/mesiodistal angulations, with application of the buccal object or SLOB (same-lingual, opposite-buccal) rule to determine the location of the impacted canine. Occlusal radiography may help localize the buccolingual position of the impacted teeth.
Extraoral Radiographic Examination.
The extraoral radiographic exam includes an orthopantomogram (OPG) and lateral cephalometric and cone beam computed tomography (CBCT) scans. CBCT is a three-dimensional imaging technique that not only provides accurate localization of the canine, but also shows the availability of bone and resorption of adjacent tooth roots. CBCT may have limited application secondary to cost and radiation exposure.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


