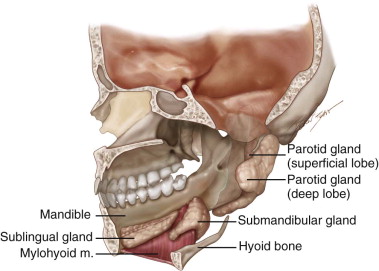
The human salivary gland system is composed of glands that are found in and around the mouth and throat. They can be divided into two distinct exocrine groups, the major salivary glands and the minor salivary glands. Collectively, the paired parotid, submandibular, and sublingual glands are referred to as the major salivary glands ( Figure 6-1 ). They all secrete saliva into the mouth through tubes called salivary ducts. The parotid duct, or Stensen’s duct, is located in the buccal mucosa adjacent to the upper molars; the submandibular duct, or Wharton’s duct, is found under the tongue in the anterior floor of the mouth; and the sublingual glands open through multiple small ducts in the floor of the mouth. In addition to these glands, many tiny glands, called minor salivary glands, are located in the lips, inner cheek area (buccal mucosa), and extensively in other linings of the mouth and throat. As a whole, salivary glands produce the saliva used to moisten the mouth, initiate digestion, and help protect teeth from decay.
General Anatomic Considerations
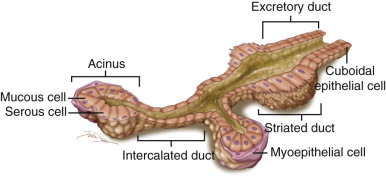
Histologically the glands are all divided into lobules. Specific blood vessels and nerves supplying the glands enter at the hilum and subsequently branch out into the lobules. The ducts follow the same general anatomic considerations applicable to all exocrine glands ( Figure 6-2 ). The acinus is the secretory end piece of the salivary gland. Acini produce and secrete the saliva into lumina formed by intercalated ducts. The intercalated ducts then join each other to form striated ducts, finally draining into ducts located between the lobes of the gland. Cuboidal epithelial cells form the ductal epithelium and are partially covered by myoepithelial cells. The acinus unit is composed of excretory/secretory cells and surrounding myoepithelial cells. Human salivary gland acinar secretory cells can be broken down into two major types, serous and mucous types; these are differentiated from one another by the chemical composition and morphologic profiles of the secretory granules within them. Mucous secretory granules contain appreciable amounts of mucin and glycoconjugates. The distal ends of the mucous acinar units are surrounded by serous demilunes in the submandibular and sublingual glands. These serous demilunes secrete small amounts of serous saliva that mixes with the mucous saliva secreted by the majority of mucous cells in the mucous acinus. In general, serous secretory granules contain little glycoconjugates and a large amount of water and ions, but some serous granules contain acidic glycoconjugates (these are termed seromucous ).
Parotid Gland
Anatomy
The parotid gland is the largest of the paired major salivary glands. The average gland weighs between 14 and 28 grams. In men the gland averages 5.8 cm in the craniocaudal dimension and 3.4 cm in the ventrodorsal axis (it tends to be slightly smaller in women). The intercalated ducts are long and thin. The parotid gland has an abundance of fatty tissue in its parenchyma, with a ratio of adipose to acinar tissue of about 1 : 1.
Although commonly mentioned as having distinct superficial and deep lobes, the parotid gland itself is actually not divided in this way anatomically. This nomenclature is based on using the facial nerve and its associated interstitial structures as a reference plane within the gland. The superficial portion is the region that overlies the lateral surface of the ramus of the mandible and masseter muscle, lateral to the facial nerve. The deep portion refers to the smaller region behind and deep to the mandibular ramus, medial to the facial nerve, located between the mastoid process of the temporal bone and the ramus of the mandible. Nearly 80% of the gland lies on the outer surface of the masseter muscle and the ascending ramus and angle of the mandible, lying caudal to and ventral to the external auditory canal and mastoid tip. The remaining approximately 20% of the gland extends medially through an area known as the stylomandibular tunnel. This area is bounded ventrally by the posterior edge of the mandibular ramus, dorsally by the anterior borders of the sternocleidomastoid muscle and posterior belly of the digastric muscle, and more deeply and dorsally by the stylomandibular ligament, which extends from the tip of the styloid process to the angle and posterior edge of the mandible. With these anatomic relationships in mind, it can be noted that the deep portion of the gland lies anterior to the styloid process, its musculature, and the carotid sheath, thereby placing this portion in the prestyloid compartment of the parapharyngeal space.
The deep lobe portion of the parotid gland is located behind the lower jaw and base of the cranium and cannot be palpated under normal conditions. However, the superficial portion can be palpated as it overlies the ramus of the mandible. The parotid gland is irregular in shape, resembling a wedge that envelops the posterior border of the ascending ramus of the mandible ( Figure 6-3 ). If viewed from its superficial surface, it extends medially to cover a portion of the masseter muscle. The body of the gland fills the space between the mandible and the surface bounded by the external auditory meatus and mastoid process. Deep to the ascending ramus, the gland extends forward variably to lie in contact with the medial pterygoid muscle. Just below the condylar neck, above the medial pterygoid attachment, the gland extends between the two. Near the condyle, the gland lies between the capsule of the temporomandibular joint and external acoustic meatus. Laterally, at the junction of the mastoid process and sternocleidomastoid muscle, the gland lies directly on the posterior belly of the digastric muscle, styloid process, and stylohyoid muscle. These structures separate the gland from the internal carotid artery, internal jugular vein, and cranial nerves (CN) IX to CN XII. A histologically distinct accessory parotid gland with both mucinous and serous acinar cells may also be seen lying anteriorly over the masseter muscle between the parotid duct and zygoma; its ducts empty directly into the parotid duct through one tributary.
Fascia
The parotid gland is fixed by fibrous attachments at several important anatomic landmarks, including the external acoustic meatus, mastoid process, and fibrous sheath of the sternocleidomastoid. The parotid fascia proper is an extension of the deep cervical fascia as it continues superiorly. This fascia splits into superficial and deep layers that completely enclose the gland, forming a dense, inelastic capsule that also covers the masseter muscle on the deep aspect of the parotid gland; this capsule often is referred to as the parotid masseteric fascia. The superficial fascia is thicker, extending from the masseter and sternocleidomastoid muscles superiorly to the zygomatic arch. The thinner deep layer extends to the stylomandibular ligament, which separates the superficial and deep lobes of the parotid gland. Important as a surgical landmark, the stylomandibular ligament passes deep to the gland from the styloid process to the posterior border of the ascending ramus just above the angle, thereby also separating the parotid and submandibular glands. The stylomandibular ligament and the mandibular ramus combine to form a tunnel through which a process of the gland can extend into the parapharyngeal space.
Stensen’s Duct
The parotid duct (Stensen’s duct) is 4 to 6 cm in length, 5 mm in diameter, and runs 13 mm inferior and parallel to the zygomatic arch. Following a line from the floor of the external auditory meatus to just above the commissure of the lips, the duct exits the gland from its anteromedial surface and courses superficially over the masseter muscle and buccal fat pad. It then turns medially at the anterior border of the muscle, at a near right angle, to pierce the buccinator muscle to empty into the oral cavity. The orifice into the oral cavity, known as the parotid papilla, typically can be found buccal to the upper second molars. In 20% of people, as the duct passes over the masseter, it may receive the duct of an accessory parotid gland that is usually slightly cranial to Stensen’s duct.
Neural Anatomy
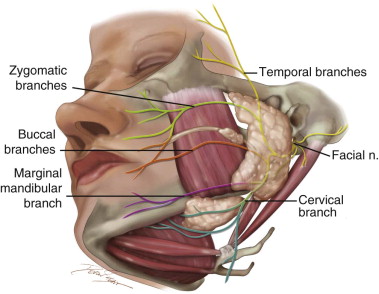
The facial nerve is intimately associated with the gland and has often been used to divide the parotid gland into a larger superficial lobe and a smaller deep lobe ( Figure 6-3 ). The main trunk is always located in the triangle formed by the mastoid, angle of the mandible, and cartilaginous ear canal. Within this triangle the main trunk can be found medial to the mastoid, almost at a point between the mandible and the cartilaginous ear canal. The facial nerve is a mixed nerve carrying motor, sensory, and parasympathetic fibers; it has five intracranial segments and one extracranial segment.
The motor fibers originate from the facial nucleus of the pons. These fibers are joined by the nervus intermedius before entering the temporal bone through the internal acoustic meatus. The nerve takes a tortuous course anteriorly toward the geniculate ganglion and then travels posteriorly along the medial wall of the tympanic cavity toward the second genu at the oval window. The facial nerve gives rise to three small branches just before it exits the skull: (1) the posterior auricular, (2) the posterior digastric, and (3) the stylohyoid nerves. As it exits the skull through the stylomastoid foramen, the facial nerve provides motor innervations for the muscles of facial expression. After exiting the skull through the stylomastoid foramen, it courses anterolaterally around the styloid process, following the lateral surface of the posterior belly of the digastric muscle approximately 1 cm before piercing the posterior capsule of the parotid gland, where it splits into two main branches. This area of the facial nerve before it splits is an important surgical and anatomic landmark known as the pes anserinus (Latin for “goose’s foot”). The upper temporofacial branch takes a vertical course, and the lower cervicofacial branch takes an anterior course. The two main branches continue within the gland, lateral to the posterior facial vein and external carotid artery. These two main branches eventually divide into five smaller branches: the temporal, zygomatic, buccal, marginal mandibular, and cervical branches.
Six different branching anatomic patterns have been described, with rami often communicating between the branches, sometimes within the parotid gland but more often anterior to it. The upper temporal and zygomatic branches are branches of the upper division, sharing the motor supply of the orbicularis oculi; the temporal branch alone supplies the forehead musculature. The marginal mandibular and cervical branches are branches of the lower division; the cervical branch supplies the platysma, and the remaining buccal and mandibular branches share the supply of the remaining facial muscles. The buccal branch demonstrates the most anatomic variability and cross-innervation, with the highest number of cross-innervations occurring between the zygomatic and buccal branches. All muscles of facial expression receive motor innervations from the facial nerve on their deep surface except for the mentalis, buccinator, and levator anguli oris muscles.
Autonomic Nerve Innervation
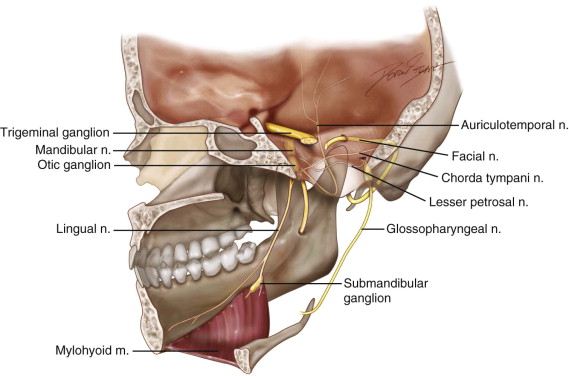
The parotid gland is innervated by sympathetic and parasympathetic fibers ( Figure 6-4 ). The function of the sympathetic fibers is most likely vasoconstriction, whereas the function of the parasympathetic fibers (CN IX) is most likely secretory. The secretory parasympathetic innervation originates from the inferior salivatory nucleus in the medulla carrying preganglionic parasympathetic fibers through the jugular foramen. The efferent fibers travel through the glossopharyngeal nerve. Jacobsen’s nerve, a branch of the glossopharyngeal nerve found distal to the inferior ganglion, reenters the skull through the inferior tympanic canaliculus and proceeds into the middle ear, forming the tympanic plexus. These fibers then continue into the middle cranial fossa as the lesser petrosal nerve, exiting through the foramen ovale to synapse in the otic ganglion. The postganglionic parasympathetic fibers leave the otic ganglion at a level below the mandibular nerve and join the auriculotemporal nerve in the infratemporal fossa. These fibers are responsible for parotid gland salivary secretion. The superior cervical ganglion supplies the sympathetic innervation via postganglionic fibers that innervate the salivary and sweat glands and cutaneous blood vessels. Acetylcholine is the neurotransmitter for both postganglionic sympathetic and parasympathetic fibers.
Arterial Supply
The transverse facial artery, a terminal branch of the external carotid artery, provides the gland’s main arterial blood supply. The external carotid artery enters the inferior surface of the gland and divides into two branches, the maxillary and superficial temporal arteries, at the junction between the middle and upper thirds of the gland. The superficial temporal artery gives off the transverse facial artery, which courses anteriorly between the zygoma and parotid duct to supply the parotid gland, parotid duct, and masseter muscle. The maxillary artery courses in a forward and upward direction behind the condylar neck in the part of the parotid gland lying deep to it initially and subsequently emerges coursing into the infratemporal fossa.
Venous Drainage
The venous return is via the retromandibular vein, which is formed by the union of the maxillary and superficial temporal veins. This vein courses through the gland to drain into both the external and internal jugular veins. The facial nerve lies superficial to the vessels, the artery is deeper, and the veins lie between them. The anatomy of the retromandibular vein varies, often bifurcating into anterior and posterior branches. The superficial temporal vein typically enters the superior surface of the parotid gland and receives the internal maxillary vein to become the retromandibular vein, lying immediately deep to the marginal mandibular branch of the facial nerve. Within the gland, it divides into anterior and posterior branches. The posterior branch joins the posterior auricular vein above the sternocleidomastoid muscle to form the external jugular vein. The anterior branch emerges from the gland to join the posterior facial vein to form the common facial vein.
Lymphatic Drainage
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


