Fig. 5.1
Relative absorption in the visible electromagnetic spectrum of hemoglobin (Hb), oxyhemoglobin (HbO2), and melanin (Image courtesy of Giovanni Olivi, Rome, Italy)
5.2.2.1 Argon Laser
Argon is a noble and inert gas and extremely stable chemical element. Argon gas is used as active medium inside the optical cavity; when it is bombed by the pumping system, its ionized molecules produce different kinds of wavelengths, among them two in the blue spectrum (470–488 nm) and one in the green spectrum (514 nm).
The possibility of using the blue argon laser (470 nm) in dentistry has been extensively studied by a Japanese group at Showa University School of Dentistry, Tokyo, Department of Endodontics, in 1998 and 1999 [24–26]. The investigations verified the ability of argon laser for smear layer and debris removal from the root canals, prepared in a conventional way and irradiated at 1 W, with 0.05 s pulse duration and 5 Hz pulse frequency [24, 25] and at 0.3 W in continuous wave [26]. However, as of today, the use of the argon lasers remains limited only to ophthalmology in retinal pathology for superficial photocoagulation (see Fig. 5.1).
5.2.2.2 KTP Laser
In the spectrum of visible light, in the green band, the wavelength 532 nm was chosen for the construction of the KTP laser (a duplicate neodymium of 532 nm), with high affinity with hemoglobin (see Fig. 5.1). This laser in fact was introduced to dentistry in the 1990s (nineties), due to its elevated capacity for soft tissue cutting and coagulation [27, 28], and it is used mainly in oral surgery and periodontics. Nowadays however, its diffusion remains limited because of its cost.
Effectively its system of construction is complex. The active medium is a solid: a crystal of Nd:YAG is excited by a diode laser pumping system; a crystal of KTiOPO4 is located between the active medium and the semi-reflecting mirror and duplicates the vibration frequency of photons, splitting the wavelength of the Nd:YAG (1,064 nm) and emitting a radiation of 532 nm in the green visible spectrum.
KTP laser emits energy continuously. Alternatively, a mechanically interrupted mode (chopped or gated) can be used to control the thermal rise in tissue during the irradiation. The delivery system is a flexible optic fiber that exits through a terminal handpiece. Fibers of different diameters (200, 300, and 600 μm) permit different uses in dentistry including endodontics.
The effective use in endodontics was reported by several studies [28–33], at power ranging from 2.25 to 3 W, at 5 Hz, per 2–5 s, and repeated for 4–5 cycles, depending on the study; no damaging thermal rise for the periodontal tissue was observed at these parameters [28, 29]. Also the root canal decontamination ability after conventional endodontic instrumentation was studied, at different power output (at 1 and 1.5 W), in dry mode or wet model [30–34].
5.2.2.3 Semiconductor Laser: Diode Lasers
Some diode lasers are built with wavelengths in the range of visible light. Lasers at 635–675 nm are used for antibacterial photodynamic therapy (aPDT or photoactivated disinfection, PAD) [35–40] because the light of these lasers, emitted in the red spectrum of light, is absorbed by particular photoactive colored substances, which when activated release singlet oxygen with elevated lytic capacity on many species of bacteria. For this reason, LED lights or diode lasers in this spectrum of light have been used in recent years with success in root canal, periodontal, and implant decontamination. This laser application in endodontics will be analyzed in Chap. 7. Recently, a new diode emitting laser radiations in both visible and near-infrared spectrum of light is promisingly introduced at 445, 660, and 970 nm for several application in dentistry, including endodontics; the optical characteristics of the blue wavelength are similar to those of blue argon laser (see Fig. 5.1).
5.2.3 Near-Infrared Lasers
Following the first studies with excimer lasers, near-infrared lasers were the first to be studied and then largely used for root canal decontamination, in particular the Nd:YAG (1,064 nm) and then diode lasers (from 810 to 1,064 nm), thanks to the optic fiber technology, introduced at the end of the 1980s (eighties) [13] that allow the introduction of the laser light deeply in the root canal.
Target chromophores of near-infrared lasers are the hemoglobin, the melanin, and the pigment of some type of bacteria (Fig. 5.2). Near-infrared lasers are mainly scattered in the target tissues; the absorption is negligible and reflection minimal. Shorter wavelengths have less deep diffusion than the longer Nd:YAG laser (1,064 nm), both in soft tissues and in radicular dentin. Near-infrared lasers of different wavelengths have slight different optical behavior, depending on the affinity of the specific wavelength with the target chromophore (see the absorption curve). Different affinities with the target correspond to different energies necessary for the clinical use.
Fig. 5.2
Relative absorption in the near-infrared electromagnetic spectrum of hemoglobin (Hb), oxyhemoglobin (HbO2), and melanin (Image courtesy of Giovanni Olivi, Rome, Italy)
This paragraph analyzes only the constructive characteristics and the interaction with tissues typical of these lasers. Chapter 6 will analyze diffusely the effects of these lasers in endodontics.
5.2.3.1 Semiconductor Laser: Diode Laser
The diode laser was introduced in endodontics at the end of the 1980s, initially for treatment of dentin hypersensitivity [41, 42] and to bio-modulate the inflammatory response during vital pulp therapy (pulp capping or pulpectomy) and other inflammatory pathologies of the maxillary bone [43, 44].
Today, diode lasers represent a valid alternative to Nd:YAG lasers for incision, vaporization, and coagulation of soft tissues (gingiva, mucosa, and pulp), for treatment of periodontal pockets (curettage, decontamination) and root canal decontamination.
The constructive simplicity and the contained dimensions justify the contained cost, which facilitates its diffusion.
The active medium is a semiconductor, which is, nowadays, miniaturized, made up of various layers (wafer-like construction). The gallium arsenide (GaA1As), doped with aluminum atoms, is widely used. Some lasers use the indium as doping atom (IGaAsP).
The activation of the semiconductor produces the emission of laser light in the invisible spectrum of the near infrared in different wavelengths (from 810 to 1,064 nm), depending on the type of semiconductor. In order to see and control the interaction of laser light with tissue, there is a visible aiming beam with low mW of power (1 mW), generally red at 650 nm or green at 530 nm.
Diode laser energy is emitted in continuous wave mode, and a mechanical system can interrupt the impulses (chopped or gated), dividing their exit in variable intervals (t on/t off). The single impulse (t on) has a linear evolution without variations from the beginning to the end of the emission, and its duration is variable, from a few microseconds to many milliseconds, with variable frequency up to 20,000 Hz. The mechanical interruption of the emission (chopped or gated mode) makes it possible to choose the time interval between one pulse and another (t on–t off), which is important for clinical purposes because it allows cooling of the irradiated tissue. By modulating the quota of thermal energy released and its effects, it is also possible to control the patient’s pain sensitivity.
The diode laser delivery system is similar to that of Nd:YAG laser and uses an optic fiber (diameter 200–300–400 μm) which ends in a terminal handpiece, going through it and coming out in a terminal curve tip. The fibers are sterilizable after cleaning and cutting of a pair of millimeters after use. Diode lasers of more recent design have fiber which ends in a handpiece where disposable tips of different diameter, angle, and length are inserted (Figs. 5.3 and 5.4). The fiber/tip must be activated before the surgical procedures. It has to be kept constantly clean using sterile dressings soaked with nonflammable disinfectant or cotton rolls. For decontamination of periodontal pockets or root canals, the activation of the tip is still a topic of debate (Fig. 5.5). It should be remembered that:



Fig. 5.3
Long and 200 μm thin disposable tip for endodontics, available for diode laser (Picasso, AMD; USA)
Fig. 5.4
Long and 200 μm thin disposable tip for endodontics, available for diode laser (BluLaser, Sirona: Germany)

Fig. 5.5
The fiber/tip activation is performed at 1 W on dark-blue articulating paper, repeating the procedure 4–5 times up to seeing the tip becomes darker
Activation of the fiber/tip concentrates the emitted energy near the tip itself; without activation of the tip a major quota of energy can be diffused at distance.
The use of thin fiber (200 μm) inside a root canal permits decontamination in the endodontic system at up to 500–750 μm of distance from the main canal [45].
It should be remembered that diode lasers are also used for LLLT: the diode laser emitted at low energy and for a long time is converted into photochemical energy that bio-modulates many cellular functions. Photochemical energy is also used for the activation of (whitening) bleaching systems.
5.2.3.2 Neodymium:YAG Laser
It is one of the first lasers to be experimented with in dentistry [13, 14]. Still today it is a valid laser system for incision, vaporization, and coagulation of soft tissues (gingiva, mucosa, and pulp) and for the treatment of periodontal pockets (curettage, decontamination) and is the best system for thermal decontamination of the root canals.
Its active medium is a solid crystal of yttrium, aluminum, and garnet (YAG), doped with neodymium. Neodymium (Nd, atomic number of 60) is a metal of the group of rare heart elements. The energy of neodymium YAG laser is produced through stimulation of the active medium using a powerful flash lamp (free-running pulse mode). Each pulse has a Gaussian development, with a quick start, a peak, and an end; between one pulse and another, there is a time of latency.
The stimulated neodymium YAG emits invisible photonics radiation at 1,064 nm, and it is equipped with a coaxial aiming beam, with low power (1 mW), generally red at 650 nm or green at 530 nm.
The emitted energy is delivered through an optic fiber (diameter 200–300–400 μm) that enters in a hollow handpiece and ends in a terminal curved tip (Fig. 5.6).


Fig. 5.6
Small hollow handpiece for Nd:YAG laser allows the passage of the fiber up to the terminal tip
The energy emitted by the laser radiation is mainly scattered in the target tissues under the form of thermal energy, while a certain quota of retrograde diffusion of energy can overlap the incident radiation, with the risk of the phenomenon of summary accumulation of thermal energy and tissue damage. For this reason, the Nd:YAG laser is only used in dentistry, in free-running pulse mode with variable frequency from 10 to 200 Hz and with a pulse duration from microseconds to milliseconds. This greatly limits the possibility of heat accumulation in irradiated tissue. The emission of short duration pulses produces elevated peak power, so to justify the elevated efficiency of Nd:YAG lasers compared to diode lasers. Only a small quota of energy is diffused for reflection.
The use of thin and flexible fibers (200 μm microns) facilitates access to the radicular canals, where the scattering and penetration in depth of this wavelength allow decontamination of the endodontic system up to a distance of 1 mm from the main canal [45–48]. The power and energy used for clinical applications produce high photothermal effect and never ablative effect on the dentin. For this reason, the near-infrared lasers are used in endodontics only for decontamination.
5.2.3.3 Neodymium:YAP Laser
The Nd:YAP laser has been constructed with a wavelength of 1,340 nm. The active medium is solid, a crystal of yttrium, aluminum, and perovskite (YAP), doped with neodymium. The optic fiber of a reduced diameter (200 μm) permits endodontic application. The constructive characteristics of this laser are very similar to those of the Nd:YAG, with a slightly different affinity with hemoglobin, melanin, and water. It is not very diffused and the clinical indications are comparable to those of other near-infrared lasers.
5.2.4 Medium-Infrared Lasers: Erbium YAG and Erbium, Chromium YSGG Laser
At the end of the 1980s (eighties) to the beginning of the 1990s (nineties), the erbium YAG laser (2,940 nm) [49–52] first and then the erbium, chromium YSGG laser (2,780 nm) [53, 54] were introduced in dentistry with the idea of substituting the drill for caries removal.
Studies in endodontics started in 1998 for the erbium YAG laser and in 2001 for the erbium chromium YSGG laser [55, 56] for the availability of specific thin tips to access to the root canals (Fig. 5.7).


Fig. 5.7
Long and 200–300 μm thin tip and handpiece for Er,Cr:YSGG laser
The Er:YAG laser has a solid active medium, a crystal of yttrium, aluminum, or garnet, doped with erbium atoms. Erbium is a silver metal of the group of rare heart elements (Er, atomic number of 68). When stimulated, the YAG crystal emits photons of a wavelength of 2,940 nm. The laser energy is delivered to a terminal handpiece through different systems, among which the optic fiber and the articulated arm are still in use.
The Er,Cr:YSGG laser also has a solid active medium, a crystal of yttrium, scandium, gallium, and garnet (YSGG), doped with atoms of erbium and chromium. When stimulated, the crystal emits radiations in the medium-infrared spectrum at 2,780 nm. This energy is transferred to a terminal handpiece through an optic fiber.
The term erbium family lasers combines the two wavelengths and is frequently used when referring to both the wavelengths without any specific connection to one another.
Erbium lasers use a visible aiming beam, red or green, to provide good visibility and control of interaction with tissue.
These lasers can develop high power, and for this reason, the energy is emitted in free-running pulsed mode, with pulses of duration and frequency of variable repetition depending on the different equipment used.
The wavelengths of the erbium family fall on the curve of water absorption (principal target chromophore). Absorption in hydroxyapatite is also high, but it has unimportant value for clinical purposes [57–60] (Fig. 5.8).
Fig. 5.8
Relative absorption in the medium-infrared electromagnetic spectrum of water (blue line) and hydroxyapatite (orange line) (Image courtesy of Giovanni Olivi, Rome, Italy)
The high absorption in water explains the effects on dentin, more pronounced in the intertubular zone, that is, more rich in water than in mineral.
The photothermal effect of erbium lasers produces vaporization of the smear layer and a certain grade of ablation and decontaminating effect that are however limited to the dentin canal surface (up to 250–300 μm in depth), where laser energy is mainly absorbed and where it produces a direct photothermal effect.
The dentin ablation happens when the energy used exceeds the threshold of dentin ablation (see Sect. 4.6.1). The ability of medium-infrared lasers to ablate radicular dentin encouraged research in the past years, to explore the possibility of preparing the canal with lasers, with quite poor results.
The affinity of erbium lasers with water explains the activation and agitation of the irrigant solution (NaOCl ed EDTA), their tridimensional streaming through the endodontic system (LAI and PIPS techniques), and their effect on bacteria decontamination, on debris and smear layer removal, via an indirect laser action.
The great presence of water in the oral soft tissues; in the hard dental tissue, such as the enamel and the dentin; and much more in the carious tissue explains the extensive use of erbium lasers in dentistry. Water is also present in the bone. For this reason, erbium lasers are considered “all tissue” lasers, very versatile for clinical use in dentistry, in periodontics, restorative, endodontics, and bone surgery, and also recommended for soft tissue therapy, especially on tissues with low vascularization and more evident fibrous components (fibroma removal, labial and lingual frenectomy, gingivectomy, gingivoplasty, operculectomy).
Clinically, the two wavelengths work in overlapping mode. However, the higher absorption in water tissues for the Er:YAG laser makes its tissue interaction more superficial when compared to Er,Cr:YSGG laser (Fig. 5.9). Under equal parameter used, also less energy is necessary for the Er:YAG laser, compared to the Er,Cr:YSGG, to ablate hard dental tissues (see ablation threshold, Chaps. 4 and 7) [61, 62]. However, is the different technology of construction and control (analogic or digital) of different laser units that produces variable performances of different lasers.
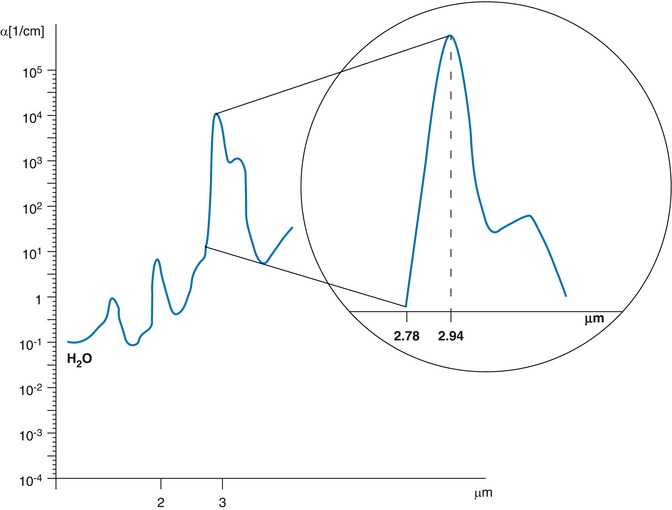
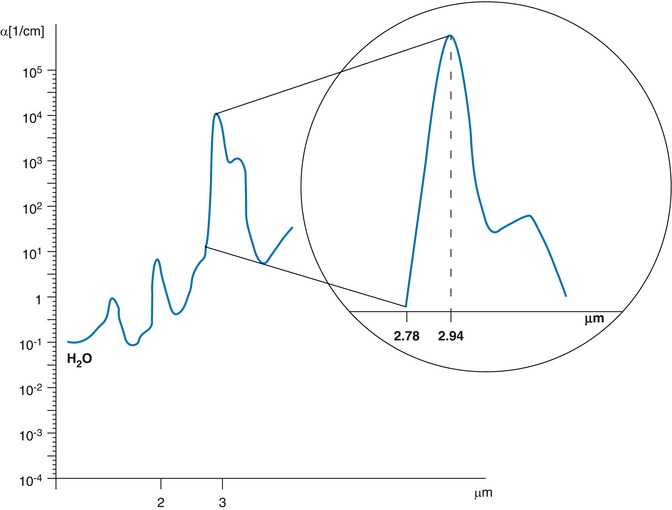
Fig. 5.9
Different water absorption coefficients in the medium electromagnetic spectrum 2780 and 2940 nm. Er:YAG at 2920 nm is three times more absorbed in water than the Er,Cr:YSGG at 2780 nm (Image courtesy of Giovanni Olivi, Rome, Italy)
Different erbium lasers can have differences in terms of delivery system (optical fiber or articulated arm), handpiece (in close contact with the tip or no contact using a mirror), straight or angled, and big or small (see Figs. 4.3, 4.4, 4.5, 4.6, 4.9, and 4.10); also tips are of different shape and size, as well as the efficacy and modulability of the air-water spray. Technological characteristics include the temporal characteristic of the pulse (pulse duration) which varies from 50 to 1000 μs and the spatial characteristics of the pulse (pulse shape). Different laser systems also offer different choice of a variety of pulse frequency from 2 to 100 pps and different power output from 0.1 to 20 W, all characteristics that allow greater possibility of managing the interaction with tissues, with better clinical application and better control of pain stimulation.
5.2.5 Far-Infrared Laser: CO2 Laser
CO2 far-infrared lasers (9,300–10,600 nm) were the first to be studied and used in endodontics for the decontamination and fusion of the apex in endodontic surgery [7–9]. Nowadays, they are no longer used in endodontics, except for the vital pulp therapy (decontamination, vaporization, and coagulation in pulp capping and pulpotomy).
Together with KTP and near-infrared lasers, the CO2 laser is still one of the best systems for incision, vaporization, and coagulation of soft tissues (gingiva, mucosa, and pulp) but is not very widely used because of its cost and the range of clinical applications limited to soft tissues.
The main target tissue is water that greatly absorbs the wavelengths.
The active medium is a gas, the carbon dioxide (CO2), and the emitted laser radiation is delivered through an optic fiber or an articulated arm.
The radiation is emitted, with different wavelengths (9,300 nm, 9,600 nm, or 10,600 nm), in the invisible far-infrared spectrum. Native CO2 laser at 10,600 nm is only useful on soft tissue. New laser technology introduced some modifications and an oxygen isotope (O18) to emit a radiation at 9,300 nm, matching the peak absorption of hydroxyapatite and making also the interaction with hard tissue applicable.
Being invisible in the far-infrared spectrum, also these wavelengths are supported by a visible coaxial aiming beam (red or green, of a few mW of power).
In the past, the modality of continuous emission (CW) created problems of thermal damage, especially in the hard tissues. Today, pulsed and super-pulsed technology make this laser one of the best systems for oral surgery, due to its elevated coagulating ability via photothermal effect. The thermal effect of CO2 lasers is able to seal small (0.3–0.5 mm of diameter) blood or lymphatic vessels, realizing an excellent coagulating effect.
5.3 Classification of Lasers in Endodontics
Lasers are used with different techniques in endodontics (Table 5.1).
Table 5.1
Classification of laser techniques used in endodontics (Olivi [63])
|
Wavelength
|
Laser technique
|
Target chromophore
|
Laser tissue interaction
|
Laser effects
|
|---|---|---|---|---|
|
Visible
Near infrared
|
Conventional
Direct irradiation
|
Bacteria pigment
|
Diffusion
|
Photothermal
|
|
Medium infrared
|
Conventional
Direct irradiation
|
Water content of dentin bacteria
|
Absorption
|
Photothermal
|
|
Visible
Near infrared
|
PAD
Indirect irradiation
|
Photosensitizers
|
Absorption
|
Photochemical
|
|
Medium infrared
|
LAI
Indirect irradiation
|
Water content of irrigants
|
Absorption
|
Photothermal cavitation
|
|
Medium infrared
|
PIPS
Indirect irradiation
|
Water content of irrigants
|
Absorption
|
Photothermal photo-acoustic cavitation
|
They can be used to directly irradiate the dentin walls or to irradiate/activate photoactive substances or irrigants, so performing the clinical action on the endodontic system indirectly (Table 5.1) (Fig. 5.10).
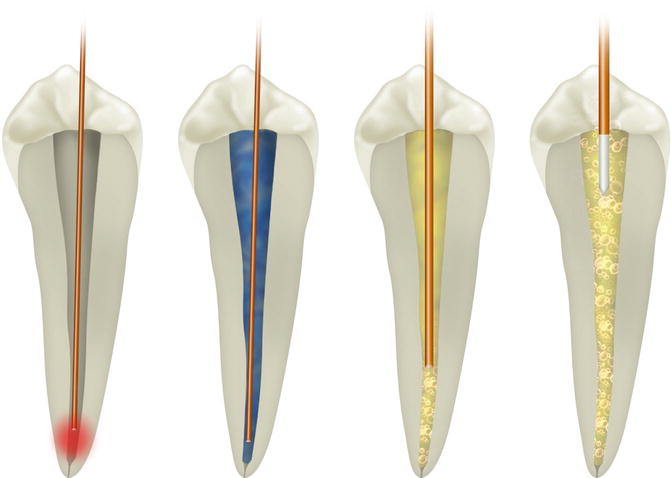
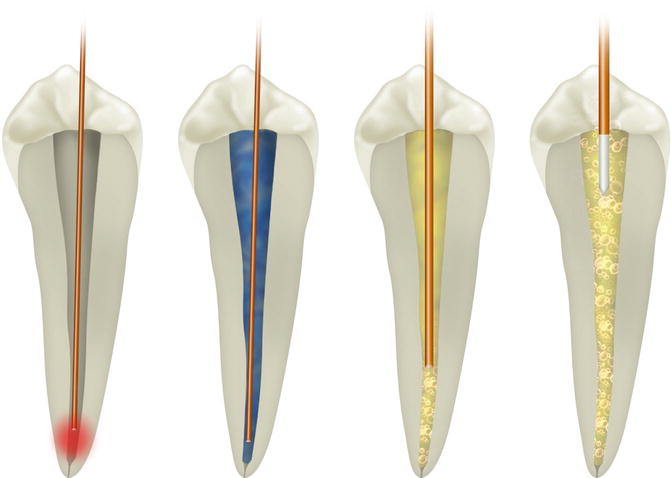
Fig. 5.10
Different laser endodontic techniques consider different positions of the tip and its movement inside the canal, or its position stationary in the chamber; also different techniques propose a dry mode or the use of different dye or irrigant solutions. From left to right: conventional laser endodontics, PAD, LAI, and PIPS (Image courtesy of Giovanni Olivi, Rome, Italy)
5.3.1 Conventional Laser Endodontics (Direct Laser Irradiation)
The laser technique used since the beginning involves the use of fibers or tips with end emission (end firing) positioned in the canal, conventionally at 1 mm from the apex. The activation of the laser starts during the movement of retraction of the fiber/tip, performing a helical movement, in a determined time. This technique is suitable for most of the wavelengths in the visible (445 and 532 nm), near-infrared (from 810 to 1,340 nm), and medium-infrared (2780 and 2,940 nm) zones of electromagnetic spectrum. The laser energy is delivered through fibers or tips inserted on terminal handpiece; endodontic tips have a specific diameter of 200–300 μm and a length suitable for this application, and also the optic fibers have a small diameter of 200 μm allowing the insertion within the root canal (see Figs. 5.3, 5.4, 5.6, and 5.7).
When in the canal, laser irradiation produces a direct thermal effect on dentin walls and bacteria that generates also undesired effects that vary depending on the wavelength used and on its interaction with the dental walls (laser-tissue interaction).
The light of the near-infrared laser (with diffusion prevalent to absorption) scatters in the dentinal tubules until it hits the pigment of the target bacteria cells, producing also thermal effects on the surface of the dentin walls.
The light of the medium infrared is mainly absorbed in the surface by the watery component of the dentin (water is the target chromophore of the erbium laser), with vaporization of the smear layer and of the debris, generating also a certain degree of dental ablation, depending on the energy used.
5.3.2 Photoactivated Disinfection (PAD)
Photoactivated disinfection (PAD) also called antibacterial photodynamic therapy (aPDT) involves the use of photosensitizers with antimicrobial activity introduced in the root canal and selectively activated by an affine wavelength: these are visible (from 635 to 675 nm) and near-infrared (810 nm) wavelengths. The laser irradiation produces a photochemical effect that activates the photoactive colored liquid with the release of active radicals and singlet oxygen that finally generate the bactericidal effect. There is no direct laser interaction with the dentin surface, almost eliminating any undesired collateral effect. This part is discussed in Chap. 7 (see Fig. 5.10).
5.3.3 Laser-Activated Irrigation and PIPS™
The laser-activated irrigation (LAI) involves the activation of the irrigant (watery solutions) with the use of the erbium and erbium chromium laser. The target is water that completely absorbs the radiation. Endodontic tips used are end firing and/or radial firing tips (conical and modified conical tips) (Fig. 5.11), and, in particular, the PIPS™ technique uses a radial and stripped tip (the last 3 mm), in order to increase the lateral emission of laser photons (see Chaps. 10 and 11) (Fig. 5.12). The irrigants, so activated by erbium lasers, become more reactive and can flow three-dimensionally in the canals, improving their antibacterial and cleaning effect. When the liquid is present in the canal, no direct interaction on dentin surface happens.
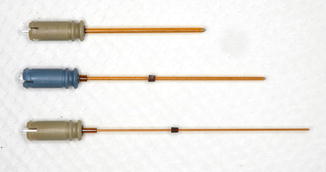

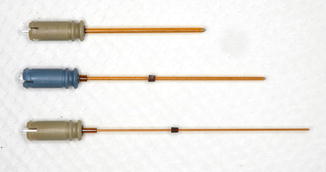
Fig. 5.11
Radial firing tips of different diameters (200–400–500 μm) and lengths for Er,Cr:YSGG laser (Waterlase MD, iPlus; Biolase; USA)

Fig. 5.12
Radial and stripped PIPS tips of 400 and 600 μm diameter, 14 and 9 mm long, respectively, for Er:YAG laser (LigthWalker, Fotona; Slovenia)
5.4 Laser-Tissue Interaction in Endodontics
The interaction between laser light and the target tissue follows the rules of physics. Laser radiation can be:
-
Reflected
-
Absorbed
-
Diffused
-
Transmitted
Reflection is an optical phenomenon due to the lack of affinity and absorption of light from the target, which, once hit, rejects the light completely. The quota reflected is about 5 % of the radiation emitted and represents the aspect of laser therapy that involves safety measures (protective glasses specific for each wavelength), because of the potential eye damage of laser radiation.
Absorption on the contrary is the expression of high affinity between light and the target which retains light in the point of irradiation. The portion of laser energy absorbed is responsible for the majority of therapeutic effects, and it is locally converted into photochemical energy, photomechanical energy, and photo-acoustic energy depending on the type of laser used, the modality of emission, and the parameters used.
Diffusion depends on the capacity of the light to spread irregularly deeper into the target. The portion of laser energy which diffuses into the tissues is responsible for the therapeutic effects of some wavelengths (visible red and near infrared), which allows decontamination at a distance from the irradiation point.
Transmission is the passage of light through a body or tissue, in the absence of interaction with it and, in consequence, without producing physical or biological effects.
Besides intrinsic optical properties of different wavelengths, the interaction depends also on the optical characteristics of the target and, in particular, on the absorption coefficient of the specific chromophore of the target tissue for a specific wavelength (optical affinity). Accordingly, different interactions happen with the target tissues: dentin, smear layer, debris, organic remnants, bacteria, and irrigant fluids.
In summary, three groups of laser-tissue interaction can be identified:
-
Laser radiation emitted in the visible blue-green spectrum of light, such as KTP laser (or neodymium duplicate at 532 nm) and argon lasers (488–514 nm), that produces effects of absorption and diffusion (scattering) of overlapping entities, with penetration in tissue at intermediate depth
-
Radiation emitted in the visible red spectrum (600–700 nm) and in the near infrared (from 810 to 1,340 nm), which renders scattering highly predominant over absorption, with deeper penetration in tissues
-
Radiation emitted in the medium- or far-infrared spectrum (2,780–2,940–10,600 nm) that mainly produces absorption in tissue and in water, superficially with unimportant phenomena of diffusion
When the laser light interacts with the target tissue, for diffusion or absorption, it generates on it the biological effects responsible for the desired therapeutical results and for the unwanted collateral effects.
5.5 Laser Effects in Endodontics
The laser light, absorbed and/or diffused in the target, generates different effects:
(a)
A photothermal effect results from the direct laser irradiation on the dentinal walls, when the lasers are used with the conventional technique for the decontamination and removal of the smear layer, positioning the fiber inside the canal; all the wavelengths produce thermal effect.
(b)
A photochemical effect produces the activation of photosensitive substances (photosensitizers) inoculated in the canal and responsible for the antibacterial effects of the photoactivated disinfection (PAD), without direct irradiation (and interaction) on the dentin; this effect is characteristic of visible (635–675 nm) and near-infrared (810 nm) lasers.
(c)
Photothermal effect primarily and photomechanical-acoustic effect successively activate the commonly used irrigants in endodontics during the laser-activated irrigation and PIPS, without any direct irradiation (and interaction) on the radicular dentin, when the irrigant liquids are present and remain in the canal. These effects are typical and exclusive of medium-infrared lasers.
Depending on the wavelength and on the technique used, the laser interaction will target with different modalities different substances:
-
Bacteria (in their different forms of aggregation, planktonic or biofilm)

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


