Armamentarium
|
History of the Procedure
Treatment of panfacial fractures poses unique challenges to the surgeon. These fractures are often complex in nature, and the treatment must be individualized for each patient. These injuries are complicated by concomitant injuries that require immediate attention and could delay early repair of the panfacial fractures. Important advancements have paved the way for more effective treatments, resulting in better prognoses and patient satisfaction.
Prior to the technologic amenities at a clinician’s disposal, surgical exploration was used to analyze the extent of injuries caused by trauma, and plain radiographs provided limited information of bony involvement. Advancements in technology have provided clinicians with the ability to identify areas of injury without invasive exploration. The computed tomography (CT) scan has been one of the most significant gains in this area, as it identifies the location and exact fracture patterns in precise areas. This was an important point in the history of treatments for panfacial injuries, as it allowed for better classification of facial injuries, thus allowing treating surgeons to better anticipate injuries and subsequent treatment. Ultrafast thin-section multidetector CT scanners are now providing even more detail than those utilizing wider sections, thereby preventing clinicians from missing facial fractures that were unnoticed in previous years. With these advances in radiographic imaging comes the responsibility to provide a more accurate interpretation as well as better preoperative planning and subsequent outcome. By combining CT scanned data with computer technology, the information can be viewed, analyzed, and manipulated in three dimensions, all without any invasive exploration. Axial, coronal, and sagittal views are helpful, as well as three-dimensional views, especially in severely comminuted fractures. However, two-dimensional CT still displays some injuries more accurately, such as those involving the paranasal sinuses, orbital walls, and soft tissues. The advantages of CT imaging are not limited to diagnosing but also apply to the surgical planning and treatment. This information is also readily transferable to a surgical navigation system that can be used intraoperatively.
Other advances such as antibiotics and plate and screw fixation led to improved treatment of facial fractures in general but especially panfacial fractures. The use of primary bone grafts was another advance that has impacted treatment of these fractures.
Standard Definition of Panfacial Fractures
Although there is no universally accepted definition for panfacial fractures, Markowitz and Manson defined it as a fracture that involves all three thirds of the face: upper, middle, and lower. Because all three regions are affected, these fractures involve several skeletal structures as well: mandible, maxilla, zygomatic complex, frontal bone, and the naso-orbito-ethmoid complex. Severe panfacial fractures can lead to complex facial deformities, decreased facial movements, and malocclusion. The clinician should be aware of the soft tissue injuries often associated with these fractures, as well as other injuries (such as those that are intracranial, cervical, or vascular) that may be potentially life threatening.
History of the Procedure
Treatment of panfacial fractures poses unique challenges to the surgeon. These fractures are often complex in nature, and the treatment must be individualized for each patient. These injuries are complicated by concomitant injuries that require immediate attention and could delay early repair of the panfacial fractures. Important advancements have paved the way for more effective treatments, resulting in better prognoses and patient satisfaction.
Prior to the technologic amenities at a clinician’s disposal, surgical exploration was used to analyze the extent of injuries caused by trauma, and plain radiographs provided limited information of bony involvement. Advancements in technology have provided clinicians with the ability to identify areas of injury without invasive exploration. The computed tomography (CT) scan has been one of the most significant gains in this area, as it identifies the location and exact fracture patterns in precise areas. This was an important point in the history of treatments for panfacial injuries, as it allowed for better classification of facial injuries, thus allowing treating surgeons to better anticipate injuries and subsequent treatment. Ultrafast thin-section multidetector CT scanners are now providing even more detail than those utilizing wider sections, thereby preventing clinicians from missing facial fractures that were unnoticed in previous years. With these advances in radiographic imaging comes the responsibility to provide a more accurate interpretation as well as better preoperative planning and subsequent outcome. By combining CT scanned data with computer technology, the information can be viewed, analyzed, and manipulated in three dimensions, all without any invasive exploration. Axial, coronal, and sagittal views are helpful, as well as three-dimensional views, especially in severely comminuted fractures. However, two-dimensional CT still displays some injuries more accurately, such as those involving the paranasal sinuses, orbital walls, and soft tissues. The advantages of CT imaging are not limited to diagnosing but also apply to the surgical planning and treatment. This information is also readily transferable to a surgical navigation system that can be used intraoperatively.
Other advances such as antibiotics and plate and screw fixation led to improved treatment of facial fractures in general but especially panfacial fractures. The use of primary bone grafts was another advance that has impacted treatment of these fractures.
Standard Definition of Panfacial Fractures
Although there is no universally accepted definition for panfacial fractures, Markowitz and Manson defined it as a fracture that involves all three thirds of the face: upper, middle, and lower. Because all three regions are affected, these fractures involve several skeletal structures as well: mandible, maxilla, zygomatic complex, frontal bone, and the naso-orbito-ethmoid complex. Severe panfacial fractures can lead to complex facial deformities, decreased facial movements, and malocclusion. The clinician should be aware of the soft tissue injuries often associated with these fractures, as well as other injuries (such as those that are intracranial, cervical, or vascular) that may be potentially life threatening.
Indications for the Use of the Procedure
Panfacial trauma poses several challenges for the treating surgeon, the most important of which is the complexity of injuries. The most serious injuries—which vary from case to case—should be quickly identified and addressed first. Mithani and colleagues reviewed 4786 patients treated for facial fractures and found that 9.7% had cervical spine injuries and 45.5% had associated head injuries. These concomitant injuries should be investigated closely with distinct types of facial fractures.
Sound anatomic knowledge is necessary to ensure a successful long-term outcome for patients with few postoperative complications. Blunt force to the midface region may have devastating consequences to the orbital region, even if it is not directly involved. The zygoma articulates posteriorly with the greater wing of the sphenoid bone within the orbit, and anteriorly it attaches to portion of the orbicularis oculi muscle. Any significant change in the bony orbit volume may lead to enophthalmos, which if untreated could significantly delay or hamper future treatment. Blow-in fractures, which decrease the volume of the orbit, should likewise be considered. The surgeon should also be aware of fragments of orbital bone directly damaging the globe itself, which would necessitate complete removal of the fragments. Possible orbital injuries include proptosis, coronal displacement of the globe, globe rupture, superior orbital fissure syndrome, and optic nerve injury.
There are situations in which the zygoma may not be involved directly, and instead a naso-orbito-ethmoid (NOE) injury may occur. The management of this type of injury may prove to be an arduous task for even the most-well trained surgeon, and it may require direct wiring and fixation of the fragmented and fracture sites with or without bone grafts. For significant skeletal deformities, the use of bone grafts may prove to be essential. For some high-velocity/high-impact facial injuries, closed reduction of such comminuted fractures may lead to obvious bony collapse and soft tissue shrinkage, thus necessitating early exposure and treatment. In severely comminuted fractures, such as those associated with significant bone loss or displacement in panfacial injuries, the use of primary bone grafting is often beneficial. The use of the immediate bone graft to replace bone that is missing or damaged provides the surgeon with a better opportunity for successful reconstruction. Immediate bone grafts provide several advantages such as decreased complications and reduced incidences of subsequent deformities that need additional surgical correction. However, an additional vascularized soft tissue flap might be needed to provide an adequate blood supply.
The importance of integrity of the zygomatic arch for maintaining normal facial projection and prominence of the cheek has been well documented. The zygomatic bone articulates with several important structures: superiorly with the frontal bone, laterally with the zygomatic process of the temporal bone, and medially with the maxilla, and it forms the lateral wall of the orbit. The junction of the zygomatic bone with the sphenoid is often helpful to ensure accurate reduction of zygomaticomaxillary complex fractures. It also possesses important muscular attachments: zygomaticus minor and major attach anteriorly, whereas laterally the masseter muscle attaches. Any trauma that leads to a collapse of the zygomatic arch will lead to inadequate anteroposterior projection of the zygoma and subsequently an increase in facial width. It is important to realize that when reconstructing the arch, it is rather straight and not “bowed.” If it is not reconstructed properly, there can be increased facial width and decreased facial projection.
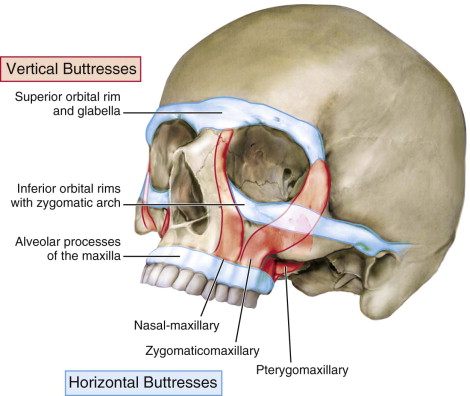
Complex facial fractures, however, may require more elaborate treatment than restoring facial projection. This includes addressing the facial width and vertical dimensions as well. These complex fractures often require reconstruction of the facial buttresses in order to restore facial height. The buttress system of the face absorbs and transmits forces and includes vertical and horizontal buttresses. Reconstructing panfacial fractures should proceed with particular attention to reconstructing these buttresses to provide the most stable result ( Figure 79-1 ). Three pairs of vertical structural supports, or buttresses, have been identified and, from anterior to posterior, are the following sites: nasal-maxillary, zygomaticomaxillary, and pterygomaxillary. The three horizontal buttresses, from superior to inferior, are superior orbital rims and the glabella, inferior orbital rims with the zygomatic arches, and the alveolar processes of the maxilla. Treatment of injuries to these areas, particularly in the anterior maxillary region, may require direct fixation of the medial and lateral buttresses combined with immediate bone graft support. This may circumvent the need for multiple surgeries, as the reconstruction effort can be done in a single stage.
Technique: Surgical Approaches
Adequate access to fracture sites is critical when treating panfacial injuries, and there are many approaches that are dependent on the area of treatment. Although there is debate among surgeons regarding which approach gives better access to sites in the lower and middle thirds of the face, the coronal approach is generally regarded as providing the widest exposure for fractures in the upper facial skeleton. Although this approach provides the best access, it does have some drawbacks: larger scars, peri-incisional hair loss, sensory deficits, frontalis nerve injury, and even corneal abrasion. Nevertheless, the coronal approach has been the standard for Le Fort III and NOE fractures, because it provides excellent exposure for reduction and fixation of the fractured sites. The coronal approach also has the added benefit of allowing the surgeon to harvest a cranial bone graft for any fractures in the vicinity that may require an immediate bone graft.
In those cases in which the coronal incision is not required for adequate exposure other, less invasive, approaches may be used. One such method is the transconjunctival and upper blepharoplasty approach for orbital fracture repair and concomitant zygomaticomaxillary complex (ZMC) fractures. The zygomaticosphenoid suture can be accessed, which aids in the evaluation for proper reduction of a ZMC fracture. This approach also offers the surgeon the option of using a lateral canthotomy. The need for this additional procedure varies depending on the goals of the surgeon: isolated orbital floor fractures can be treated without one, but those fractures that require a greater exposure may require it.
In 1998, Garcia and colleagues introduced the transcaruncular extension of the transconjunctival approach, which provided excellent access and visualization of the medial orbital wall. The transcaruncular approach is not as invasive as the traditional coronal approach, nor does it produce any significant visible external scars. Moreover, it has been shown to be used in the management of other pathologies such as frontoethmoid mucoceles.
The zygoma and mandible are accessed through a gingivobuccal sulcus incision, which can be used to treat comminuted and malunited fractures. This approach allows for the visualization and reconstruction of important vertical buttresses.
Sequencing
Treatment of panfacial fractures can prove to be challenging for both experienced and inexperienced surgeons. As with any facial fracture, the goal of treatment is to restore both the facial contours (facial width, projection, and height) and function prior to the injury. Panfacial fractures involve all three regions of the face, so there are several sequencing algorithms at the surgeon’s disposal: “top to bottom,” “bottom to top,” “inside out,” and “outside in.”
Bottom-to-Top Approach ( Figure 79-2, A )
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


