Armamentarium
|
History of the Procedure
Le Fort I osteotomy for the correction of maxillary hypoplasia in a cleft palate patient is reported to have been first performed by Axhausen in 1939, but the operation was improved by Schuchardt, who added the posterior dysjunction procedure that enabled the necessary mobilization of the pedicled maxilla. Scarring and possible obliteration of the greater palatine arteries as a result of earlier cleft palate repair gave rise to concerns about the blood supply of the downfractured cleft maxilla through a buccal incision, but the seminal work of William H. Bell demonstrated the safety of a Le Fort I osteotomy. Modifications of the Le Fort I technique were developed to enable differential movement of the maxillary segments and closure of dental gaps both in unilateral and bilateral clefts and simultaneous grafting of the alveolar clefts. When nasomaxillary hypoplasia is present, Henderson and Jackson proposed a Le Fort II osteotomy.
History of the Procedure
Le Fort I osteotomy for the correction of maxillary hypoplasia in a cleft palate patient is reported to have been first performed by Axhausen in 1939, but the operation was improved by Schuchardt, who added the posterior dysjunction procedure that enabled the necessary mobilization of the pedicled maxilla. Scarring and possible obliteration of the greater palatine arteries as a result of earlier cleft palate repair gave rise to concerns about the blood supply of the downfractured cleft maxilla through a buccal incision, but the seminal work of William H. Bell demonstrated the safety of a Le Fort I osteotomy. Modifications of the Le Fort I technique were developed to enable differential movement of the maxillary segments and closure of dental gaps both in unilateral and bilateral clefts and simultaneous grafting of the alveolar clefts. When nasomaxillary hypoplasia is present, Henderson and Jackson proposed a Le Fort II osteotomy.
Indications for the Use of the Procedure
A sizable proportion of repaired cleft lip and palate patients—unilateral cleft lip and palate (UCLP), bilateral cleft lip and palate (BCLP), and isolated cleft palate patients—present with variable degrees of maxillary growth deficiency or maxillary hypoplasia. Correction of these deformities by orthognathic surgery is a standard of care but is considered by many to be difficult to perform in terms of surgical movement due to scarring and in terms of risks to the blood supply of mobilized segments. This chapter addresses specific descriptions of the maxillary and midface surgery in cleft patients; however, considerations concerning the mandible in cases of bimaxillary skeletal corrections are beyond the scope of this chapter.
Maxillary Hypoplasia
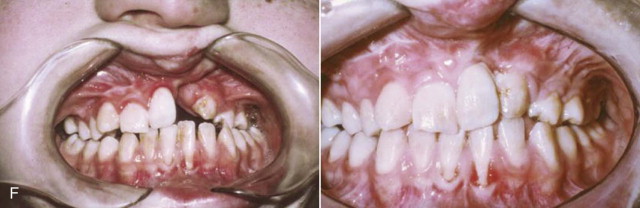
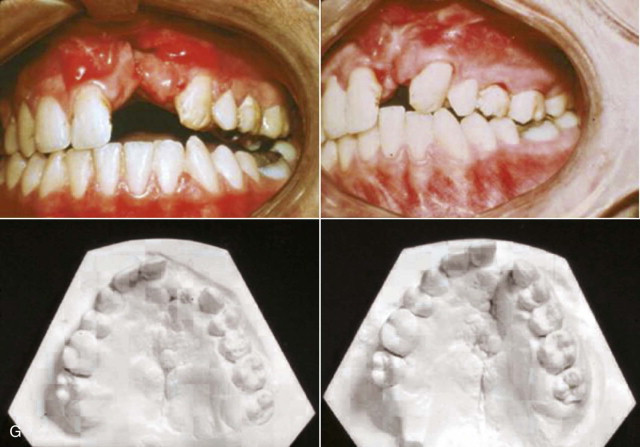
The commonly encountered maxillary hypoplasia is a three-dimensional deformity: retrusion (horizontal plane), shortening (vertical plane), and collapse (transverse plane). Unilateral or bilateral alveolar clefts will be present in UCLP and BCLP, respectively, and may or may not have been bone grafted prior to orthognathic surgery. A Le Fort I osteotomy with relevant modifications is indicated.
Nasomaxillary Hypoplasia
In some patients, the nasal pyramid is deficient in length, projection, or both; this is in addition to the hypoplasia of the dentoalveolar complex. A Le Fort II osteotomy with modifications is indicated in such cases. When the anticipated correction of the nasal pyramid and dentoalveolar complex require differential movement to achieve the overall facial correction, a two-stage procedure is planned (Le Fort II followed some months later by Le Fort I).
Limitations and Contraindications
Surgical movement of the cleft maxilla after osteotomy is limited by a variable degree of tissue scarring in the repaired palate. Adequate mobilization of the maxilla is therefore essential and requires patience to achieve the maximum possible stretching of tissues without tearing. If the required surgical movement is extensive and considered beyond the reach of on-table achievement, a gradual distraction protocol of the Le Fort I may be planned (description beyond the scope of this chapter).
Grafting of alveolar clefts in the mixed dentition permits arch alignment and elimination of interdental gaps orthodontically before orthognathic surgery. If grafting results in an adequate bony bridge with good soft tissue coverage and no oronasal fistula, a standard Le Fort I downfracture through a buccal incision is employed. However, if the result of such grafting is inadequate and a dental gap or fistula remains, osteotomy and differential segment movement to close or control the dimension of the dental gap with simultaneous alveolar cleft grating is possible both in the unilateral and bilateral cleft situation.
If the bilateral alveolar clefts exhibit an inadequate bony bridge after grafting, or if a fistula is present palatally in association with the alveolar clefts, a maxillary downfracture approach through a full buccal incision is contraindicated as a danger to the vascular supply of the premaxilla. Here a modification of technique is employed.
However, these osteotomies and simultaneous alveolar cleft grafts can only be done at the Le Fort I level. If the skeletal deformity requires a Le Fort II operation, alveolar cleft grafting is preferred before the procedure.
Technique: Le Fort I Osteotomy—Unilateral Cleft Lip and Palate (UCLP) Ungrafted Alveolar Cleft
Step 1:
Incision
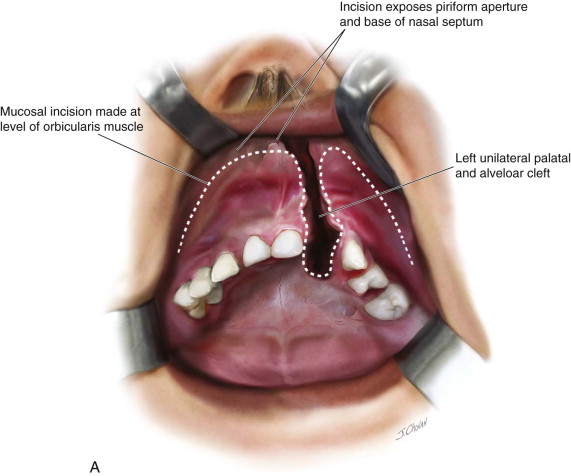
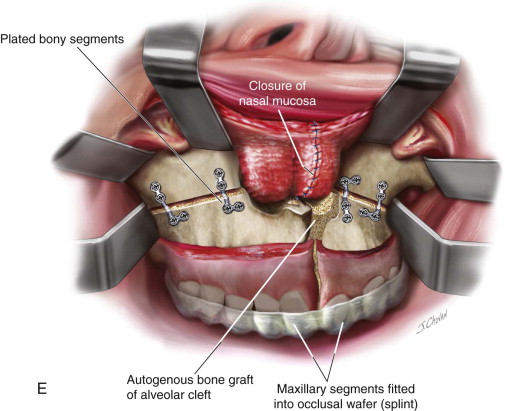
After infiltration of the mucosa with Xylocaine and epinephrine, an incision is made in the upper labial mucosa to the level of the orbicularis muscle. The blade is then angled parallel to the muscle and taken through submucosal tissue and periosteum to bone. Incision extends from the second premolar to the contralateral equivalent but dips down in the alveolar cleft region to enable access to the bony edges of the cleft. Subperiosteal exposure of bone extends from one tuberosity to the other. The piriform aperture and the base of the nasal septum are exposed. The nasal mucosa is raised away from the alveolar cleft to expose the bony edges ( Figure 56-1, A ).
Step 2:
Osteotomy
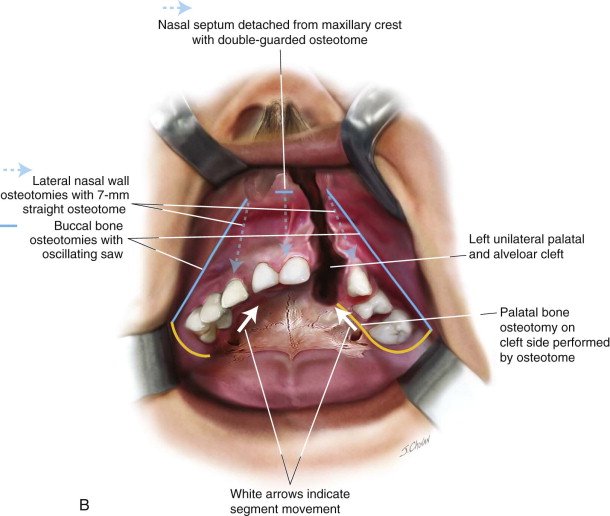
With the oscillating saw, a standard Le Fort I bone cut is made on the buccal bone surface of the major segment and minor segment. Lateral nasal walls osteotomies are completed with a 7-mm straight osteotome. The nasal septum is detached from the maxillary crest with the double-guarded nasal osteotome. Posterior tuberosity dysjunction is completed using the curved pterygoid osteotome ( Figure 56-1, B ).
Step 3:
Downfracture
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


