Implant Fixture
Implant fixtures are designed to integrate with the host’s bone and provide stability and retention for the restoration. Fixtures are available in many different lengths, shapes (e.g., tapered), and widths (or platform sizes). Manufacturers produce differing designs, each having unique features. These unique features require clinicians and laboratory technicians to adhere strictly to the individual manufacturer’s procedures and guidelines when placing and constructing implant borne prosthetics.
To provide successful osseointegration, the fixture material must be biocompatible. Currently, the most popular material is either commercially pure titanium (typically 99.2% pure) or titanium alloy. Titanium has proved to be biocompatible in long-term evaluations and documentation reporting on the success and longevity of dental implants.3, 4 Titanium is lightweight and noncorrosive (because of its oxide layer); it appears to be the most predictable material for manufacturing implants and implant components. Titanium is graded according to its carbon and iron content. In general tensile and yield strength increases with the grade number.
Titanium 4 is used in most situations because it is stronger than other grades. Recently grade 5 titanium is being used increasingly. This alloy consists of 6% aluminum and 4% vanadium alloy and offers better strength and fracture resistance.
A more recent development is the use of high strength zirconia ceramics as a material for dental implant fixture. They are considered to be inert in the body and exhibit minimal ion release compared with metallic implants. Yttrium-stabilized tetragonal zirconia polycrystals appear to offer advantages over aluminum oxide for dental implants because of their higher fracture resilience and higher flexural strength.5 Zirconium appears to offer the same rate of success as titanium in its osseointegration properties,6 although research in this field is currently limited.
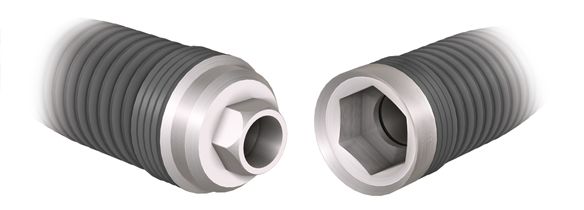
The two most common mating interfaces of the abutment to fixture platform are described as “internal hex” or “external hex” configurations (Fig. 17-2). This configuration prevents rotation of the abutment. Manufacturers have created numerous variations of this basic design. It is beyond the scope of this chapter to discuss every implant design, and esthetic principles may vary because of the limitations and enhancements of any a particular design.
Implant Abutments
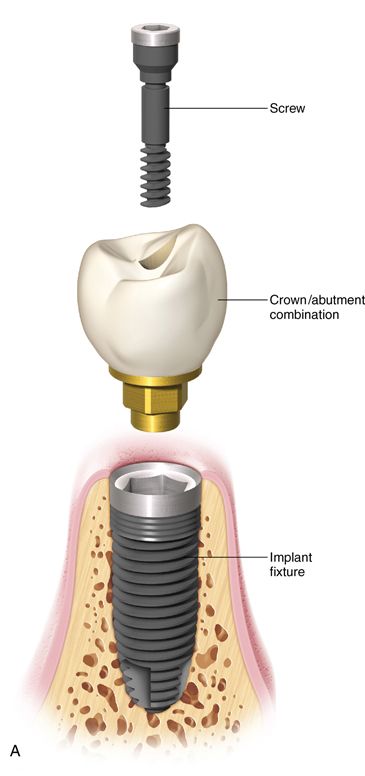
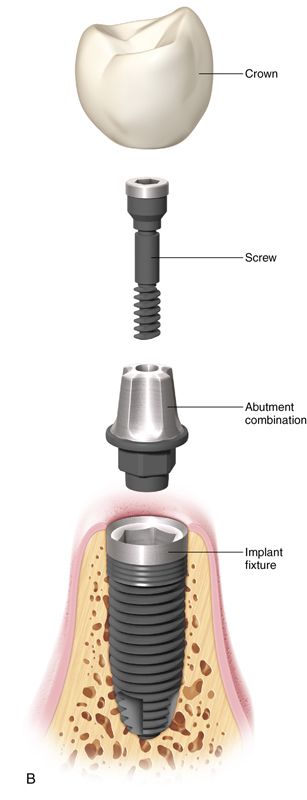
The implant abutment links the implant fixture to the restoration. Abutments are available in a variety of different types, each designed to manage a particular clinical situation (Fig. 17-3 B,C). The abutment provides an area of retention similar to a prepared tooth for cementation of a crown. Some clinical situations, typically related to angle correction, necessitate the fabrication of a custom cast or CAD/CAM abutment, which is constructed at the implant level (Fig. 17-3 A). The definitive prosthesis is placed directly on this custom abutment. The definitive prosthesis or prosthetic superstructure may be cemented to the custom abutment or screw retained. The abutment generally consists of an abutment and an abutment-retaining screw. The abutment retaining screw maintains the abutment’s position on the implant.



Prosthetic retaining screws are generally constructed of gold alloy or titanium. They are recessed internally within the occlusal surface of the abutment and hold the definitive restoration in place.
Compressive forces, generated across the implant-abutment interface by tightening the abutment retaining screw to a specific torque help maintain the integrity of the connection and position of the screw, although preload forces slowly decay with time. They are recessed internally within the occlusal surface of the abutment and hold the definitive restoration in place. Preload torque recommendations vary but typically range from 10 to 35 N-cm, depending on screw material and implant/abutment manufacturer. Preload for the abutment screw should ideally be established using a torque wrench and must be sufficient to ensure that lateral forces are distributed to the implant abutment interface rather than to the screw to reduce the likelihood of loosening or fracture.7
The abutment provides an area of retention similar to a prepared tooth for cementation of a crown. Some clinical situations typically related to angle correction necessitate the fabrication of a custom cast or CAD/CAM abutment, which is constructed at the implant level. The definitive prosthesis is placed directly on this custom abutment. The definitive prosthesis is placed directly on this custom abutment. The definitive prosthesis or prosthetic superstructure may be cemented to the custom abutment or screw may be retained.
Implant Restoration
Restorations are cemented or are part of an abutment attached directly to the implant fixtures by internal prosthetic retaining screws. Modern porcelain systems provide many options to choose from when planning an implant restoration.
Diagnosis and Treatment Planning
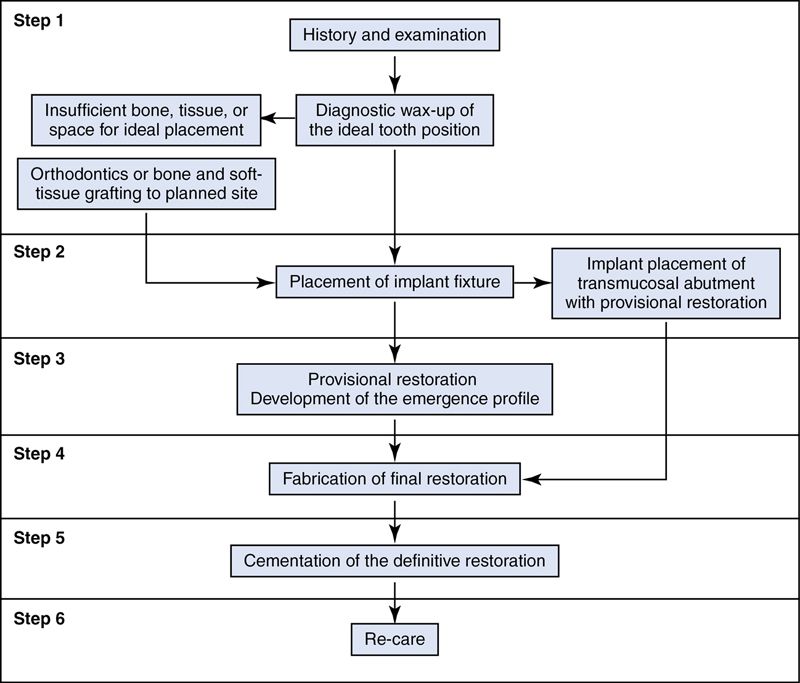
To obtain ideal esthetic results it is critical that the restorative dentist, in conjunction with the implant surgeon and laboratory technician, formulate a preoperative plan. Figure 17-4 outlines the potential treatment pathways that can be taken during implant therapy. Treatment planning must address hard and soft tissue deficiencies and combine this with precision in implant placement. This plan culminates in the fabrication of a surgical guide. However, a number of factors must be considered first.
Patient Selection
An appropriate medical history should be obtained and evaluated for systemic conditions to prevent complications during the treatment. The dental examination must consider active infection caries, endodontic lesions, and periodontitis. All the active infections should be treated before implant placement.
Psychological Considerations
The issue of patient expectation must be addressed before implant placement.
Patients must be informed that the professionals’ ability to satisfy their concerns may be limited. Persistent unrealistic expectations warrant the use of alternate treatment plans.
Oral Examination and Esthetic Factors
To evaluate the implant site in esthetic areas, the following factors should be considered.
Smile Line.
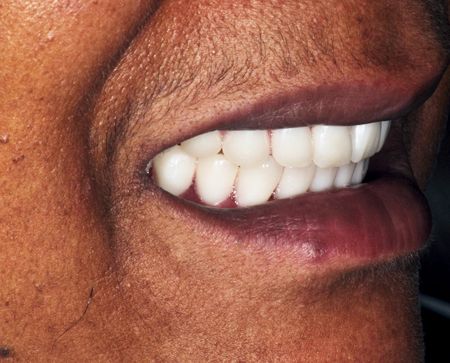
The study of the smile line is the most important factor in evaluating the patient’s dental esthetics. Lip position relative to the display of teeth and gingiva must be evaluated at rest, while speaking, with a moderately relaxed smile and with a full smile (see Chapter 2).
Tooth Morphology and Periodontal Biotype.
The periodontal biotype is an important factor in evaluating the prognosis of implant-supported restorations in the esthetic zone. Two periodontal biotypes related to tooth morphology have been described.9
Thin scalloped periodontal biotype.
The thin, scalloped biotype (Fig. 17-5 A) is associated with less than 15% of clinical situations and is characterized by a delicate soft tissue, a scalloped underlying osseous form, and often has dehiscence and fenestrations and a reduced quantity and quality of keratinized mucosa.


It is associated with a specific dental morphology with anatomically triangular crowns, small interdental contact surfaces in the incisal third, and long thin papillae. It responds to surgical and prosthodontic interventions with recession, apical migration of the periodontal anchorage, and loss of underlying alveolar volume, which results in an empty space known as a black triangle.
It is usually is accompanied by thin vestibular cortical bone, with a tendency to form bone defects secondary to bone remodeling and resorption after tooth extraction or implant placement.
Thick flat periodontal biotype.
The thick, flat biotype (Fig. 17-5 B) exhibits dense, fibrotic soft tissue. The underlying bone is thick and dense. It is associated with dental crowns that are square and convex in the cervical third. The contact points between crowns are long and often extend to the zone of the cervical third. It presents with papillae that are considered short when compared with the thin periodontal biotype. It responds to surgical aggression with scar formation that can jeopardize the aesthetic and functional outcome.
Mounted Diagnostic Cast Analysis
Preoperative mounted diagnostic casts can influence decisions concerning the selection of the type of definitive restoration. For example, if the final tooth position will be facial to the residual mandibular ridge, a hybrid-type prosthesis may be considered, as opposed to a conventional crown and fixed partial denture restoration.
In the maxillary arch, an occlusal rim demonstrates the amount of facial positioning required of the replacement tooth to properly support the maxillary lip relative to the residual ridge. This aids in determining whether a conventional crown and fixed partial denture prosthesis, a hybrid prosthesis, or an overdenture should be constructed to best support the lip.
In the fully edentulous patient, it may be necessary to construct a trial tooth setup to precisely determine final tooth position. This is especially true when the location of the teeth is changed both in the arch to be reconstructed with the osseointegrated dental implant and in the opposing arch, which may be restored conventionally. Because tooth position in one arch will affect tooth position in the opposing arch, the location must be determined precisely before constructing the mandibular surgical guide. In those situations, a wax try-in of the maxillary and mandibular teeth should be constructed as part of a diagnostic workup before constructing a surgical guide and placing implants (Fig. 17-6).
The guidelines for selection of a conventional crown and fixed partial denture prosthesis, hybrid prosthesis, or overdenture prosthesis after diagnostic cast analysis are as follows:
• Patient’s desire for a fixed restoration. For many patients, the avoidance of a removable appliance is paramount.
• The size of the framework involved. This may eliminate the possibility of using a conventional crown and fixed partial denture-type prosthesis because of the amount of necessary metal.
• Amount of interarch distance. The amount of interarch distance is important because moderate to severe resorption requires a hybrid prosthesis or overdenture to replace missing alveolar bone and soft tissue. If providing adequate lip support is critical, an overdenture is generally necessary, especially in the case of severe resorption.
• Number and location of implants. For construction of a conventional crown and fixed partial denture-type prosthesis, implants must be positioned in tooth locations. In addition, the implants must be adequately spaced in the anterior and posterior regions to provide adequate stabilization.
• Strength and dimension of supporting bone. When severe resorption has occurred, especially in the mandibular posterior region of totally edentulous patients, placing an overdenture is preferred. An anterior fixed appliance can develop significant functional forces that may overstress the mandible, which thins posteriorly. This may cause fracture of the mandible because of an overload of the anterior region with a fixed restoration.
Radiographic Analysis
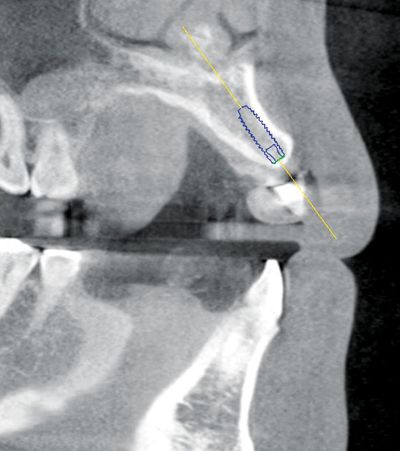
Proper radiographic analysis is needed to evaluate the amount of bone available in the area. Computed tomography scans (Fig. 17-7) disclose bone dimension and the contours of the residual ridge and guide proper angling of an implant at a given edentulous site. The sectional portion of the CT scan is especially important because it gives an indication of facial-lingual bone dimension, bone quality, and the location of vital structures.
Types of Prostheses
Implant restorations can be attached to the implant fixture with screws (screw-retained) (Fig. 17-8 A), or it can be cemented to an abutment, which is attached to the implant fixture with a screw (cement retained) (Fig. 17-8 B). Each method has advantages and disadvantages. However, in certain clinical situations, only one method is indicated.
Screw-Retained Prosthesis
Advantages
• Easy prosthesis retrieval. Allows for the retrieval of the prosthesis without damage to the restoration or the implant fixture.
• Reduced interarch dimension. Used when the interarch dimension is less than 5 mm from the crest of the tissue to the opposing arch.
• Eliminates cement margins. Absence of cement margins which can result in adverse peri-implant tissue response.
Disadvantages
• Occlusal esthetic requirements. The esthetics of the occlusal surface can be partially compromised when the screw access area is filled with a composite resin, especially when metal-base frameworks are used. The introduction of zirconia-base frameworks has lessened this complication. The white or shaded substructure facilitates an esthetically pleasing closure of the access opening; however, if the top of the screw is near the occlusal surface it may be difficult to completely mask it.
• Requires ideal fixture positioning. Ideal position and angulations of the fixture in relation to the anticipated definitive restoration are required.
• Passive fit considerations. A passive fit is more difficult to attain for a screw-retained implant restoration with more than one implant. The improving accuracy of CAD/CAM over traditional casting, even when corrective procedures are included, aids in the fabrication of better fitting frameworks.
Cement-Retained Prosthesis
Provisional cements should be used in order to maintain retrievability of the prosthesis. Conventional or CAD/CAM custom abutments or prefabricated (stock) abutments are available.
Advantages
• Accessibility. The cement-retained prosthesis is easier to seat in areas where accessibility with screwdrivers is limited.
• Fixture alignment less critical. The abutment can compensate for misaligned fixtures.
• Familiar clinical procedures. Techniques more closely parallels conventional crown-and-fixed partial denture technique.
• Passivity requirements. Fabrication and seating of passively fitting restorations is easier than screw-retained prostheses.
• Cement retained. The cement layer may act as a shock absorber and enhance the transfer of load throughout the prosthesis-implant-bone system.10
Disadvantages
• Soft tissue concerns. There is a potential risk for cement trapping in the peri-implant tissue (Fig. 17-9). Cement extrusion into the sulcular area may result in soft tissue inflammation or even in an exudate.11
• Cement margins. Removal of excess cement with plastic and metal scalers may result in scratches and gouges on the implant surfaces.12, 13
• Inadequate interarch distance. A minimum of 5 mm of abutment is required to provide predictable retention for the definitive restoration.14 When a reduced amount of interarch distance is available, a screw-retained prosthesis is indicated.
• Retrievability concerns. Despite the use of provisional cements to allow retrievability, removal of the prosthesis should be carried out with great care to avoid damaging the restoration, abutment, or implant fixture.

Abutment Selection
The choice of the implant abutment can be daunting because of different abutment types. Materials such as titanium and various high-strength ceramics (zirconia, lithium di-silicate) are available. Abutments can be categorized as prefabricated abutments (stock abutments), custom abutments (castable abutments or milled), or combined abutment/crown (screw-retained prostheses). Titanium abutments are milled from solid titanium alloy blanks. Zirconia abutments are milled from zirconia blanks and are available in multiple shades. Before selecting an abutment several factors must be considered, including visibility of the region (e.g., high vs. low smile line), the gingival biotype (high scalloped, thin vs. low scalloped, thick), angulation of the implant, inter-arch distance, and peri-implant tissue height (see Chapter 2).
Visibility and Gingival Biotype
In esthetically demanding situations, customized ceramic abutments are indicated to avoid the visible display of metal through the soft tissue, which can occur of when metal abutments are used, particularly in patients with a high smile line and thin biotype. This not only produces the best esthetic results, but also partially compensates for future soft tissue recession (Fig. 17-10 A).



Angle of the Implant
Precise preplanning and the construction of surgical guides suggest the proper positioning of the implant. However, the clinical acceptability of this predetermined position is determined by the available bone, when bone augmentation is not possible. Sometimes in the maxillary premolar and maxillary anterior regions, implants must be placed with a facial flare to be within the supporting bone. This creates an unesthetic screw access opening in the facial aspect of a screw-retained restoration.
To compensate, a custom abutment can compensate for the angle of the implant so that it emerges from the soft tissue in a favorable position (Fig. 17-10 B). A prosthesis can be cemented over these custom abutments, producing an esthetic result (Fig. 17-10 C). Another option is the use of a pre-angled stock abutment.
Interarch Distance
Successfully cemented retained restorations with predictable retention require 5 mm of abutment height. If the vertical distance from the crest of the tissue to the opposing tooth is less than 5 mm, then a screw-retained restoration is indicated.
Peri-implant Tissue Height
If the distance between the platform of the implant and the crest of the tissue is less than 3 mm, a stock abutment (prefabricated) may be chosen, as the margin is sufficiently accessible for cleaning at the time of cementation.16 If it is greater than 3 mm, a scalloped prefabricated or custom abutment should be used to position the cement in a more accessible, cleansable position relative to the gingival margin.
Implant Position and Alignment
Osseointegrated implants are ideally positioned in the site previously occupied by the natural tooth, assuming that it was properly located before extraction. Implants placed in an interproximal position can result in considerable restorative difficulties in final crown contour and esthetics when crown and fixed partial denture type restorations are planned.
Considerations with the Peri-implant Papilla
Loss of implant results in a “black triangle” around the implant-supported crown and fixed partial denture type restorations. Phonetics difficulties and food impactions can also occur. Implant position affects interproximal tissue esthetics between a natural tooth and the implant restoration or between two adjacent implants. Correct three-dimensional placement (mesiodistal, buccolingual, and incisoapical) of the implant in the bone enhances the likelihood of an acceptable result.
Mesiodistal Position.
The mesiodistal distance between an implant and a neighboring tooth should be at least 1.5 mm. If this minimum distance is not maintained, the attachment on the tooth side may undergo resorption to the level of that of the implant; this will, in turn cause a loss of interproximal papilla.17 This also creates restorative problems. Poor embrasure forms and emergence profiles will result in restorations with long contact zones and a compromised clinical outcome.
There should be at least 3 mm between two adjacent implants fixtures.18’19
Buccolingual Position.
After the implant osteotomy is prepared, the buccal wall should be intact. It should ideally measure at least 2 mm in thickness. This is important to ensure proper soft-tissue support and to avoid the resorption of the facial bone wall following the placement of a restoration.
Apicocoronal Position.
The implant platform should be 1 mm apical to the cement-enamel junction of the contralateral tooth in apicocoronal direction.20 This recommendation, however, is only valid when the contralateral tooth is without periodontal tissue loss.
Considerations with a Congenitally Missing Lateral Incisor
Ideally the definitive restoration will simulate the natural tooth. This can be a challenge if a patient is congenitally missing one or two maxillary incisors. The amount of space required for the restored tooth should be determined by the contralateral incisor. However, in some patients, the existing lateral incisor may be peg shape and in others, both lateral incisors are congenitally missing. In the latter two situations, the space for the lateral incisor is determined by two factors: esthetics and occlusion clearance. An esthetic relationship exists between the size of the maxillary central and lateral incisor teeth. Ideally the maxillary lateral incisor should be about two thirds the width of the central incisor.21 One of the most predictable methods to determine the size of the lateral is to fabricate a diagnostic wax-up.
Clinical Case Showing Congenitally Missing Maxillary Lateral Incisor.
A 21-year-old female patient presented with an over-retained primary maxillary right canine in need of extraction, and for a consultation on treatment options to replace the congenitally missing maxillary lateral incisor. The patient’s medical history was noncontributory. A detailed examination of the teeth and periodontium was performed to assess the esthetic risk for implant dentistry. The patient’s gingival biotype was thin to medium thick and scalloped, presenting a broad band of keratinized mucosa (Fig. 17-11 A). The maxillary left lateral incisor was a peg lateral incisor. The maxillary right canine had migrated mesially into the lateral incisor location. The periapical radiograph revealed root resorption on tooth C and distal caries (Fig. 17-11 B).









Restorative options included:
1. Extraction of the primary maxillary right canine, placement of a three-unit resin-bonded (“Maryland”) fixed partial denture and recontouring of the maxillary right permanent canine so that it would to appear to be a lateral incisor. Also orthodontic creation of the required space for placement of a properly sized restoration on the maxillary left lateral incisor.
2. Extraction of the primary maxillary right canine, placement of a cantilever two-unit fixed partial denture using the canine as the abutment, and recontouring of the maxillary right canine so that it would to appear to be a lateral incisor. Also, orthodontic creation of the required space for placement of a properly sized restoration on the maxillary left lateral incisor.
3. Extraction of the primary maxillary right canine, placement of a single unit implant, and recontouring of the maxillary right canine so that it would to appear to be a lateral incisor. Also, orthodontic creation of the required space for placement of a properly sized restoration on the maxillary left lateral incisor.
4. Extraction of the primary maxillary right canine, orthodontic distalization of the maxillary right canine to its correct position, and placement of a single unit implant at the proper site the lateral incisor. Also, orthodontic creation of the required space for placement of a properly sized restoration on the maxillary left lateral incisor.
Option 4 was selected was selected for this patient (Fig. 17-11 C-I).
Considerations with a Small Edentulous Space with Limited Bone
When replacement tooth size or limited bone availability prevents placement of a standard-size implant, an implant of smaller diameter may be indicated. This type of implant can be used for replacing a single mandibular incisor tooth (Fig. 17-12) or a maxillary lateral incisor.

Considerations with Implant-Retained Removable Partial Dentures
Poor removable partial denture (RPD) stability occurs with highly resorbed ridges and an inadequate number of suitable abutment teeth (Fig. 17-13 A,B). Removable partial dentures with distal extensions (Kennedy Class I and II) generally have less stability than those engaging distal abutment teeth.22, 23 Implant-retained removable partial dentures have made treatment options possible to patients who previously may not have been able to benefit from implant dentistry because of limitations in health, anatomy, or finances. This treatment modality provides options for additional treatment in the future and accommodates future changes in the remaining natural dentition.



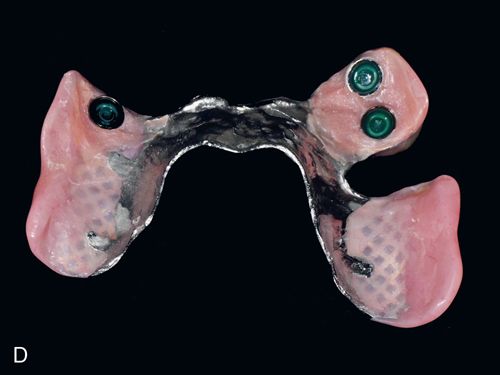
Implant-retained RPDs can combine the use of natural teeth and implants in one arch when certain requirements are met. Because teeth are considered resilient because of the presence of the periodontal ligament and dental implants are considered rigid because of their osseointegrated state, the use of a “resilient” implant attachment (Locator implant attachment systems) and possibly resilient “clasps” are needed. These attachments to provide the level of resilience needed for an implant-retained, tissue-supported prosthesis, and to allow for normal movement of the teeth24 (Fig. 17-13 B,C
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


