8
Dental Implants
Case 1: Conventional Implant Placement
Samuel Koo, DDS, MS
Case 2: Immediate Implant Placement
Mohamed A. Maksoud, DMD
Case 3: Sinus Lift and Immediate Implant Placement
Samuel Soonho Lee, DDS, and Nadeem Karimbux, DMD, MMSc
Case 1
Conventional Implant Placement
CASE STORY
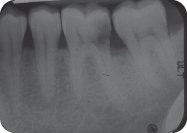
A 38-year-old Caucasian male presented with a chief compliant of: “I need a cleaning and also I have a tooth missing.” The patient had not had a teeth cleaning in 3 years (Figure 1), and tooth #19 had been extracted elsewhere 18 months ago (Figure 2) due to extensive caries (Figure 3). The patient claimed to brush his teeth two to three times daily. He flossed once a day but denies use of any mouth rinse.
Figure 1: Preoperative frontal view.

Figure 2: Missing mandibular first molar area.

Figure 3: Tooth #19 was extracted due to large distal caries.
LEARNING GOALS AND OBJECTIVES
- To understand the indications of implant treatment
- To interpret radiographic examinations for implant surgical planning
- To understand the sequence of conventional implant therapy
Medical History
The patient was prehypertensive but had no other significant medical problems and no known allergies. Occasionally the patient took diphenhydramine hydrochloride (Benadryl) for seasonal allergy.
Review of Systems
- Vital signs
- Blood pressure: 138/86 mm Hg
- Pulse rate: 67 beats/minute (regular)
Social History
The patient was a social drinker (three to four glasses per weekend). Currently he did not smoke, but he had a history of social smoking for 1 year during college.
Extraoral Examination
No significant findings were noted. The patient had no masses or swelling and the temporomandibular joint was within normal limits (Figure 4).
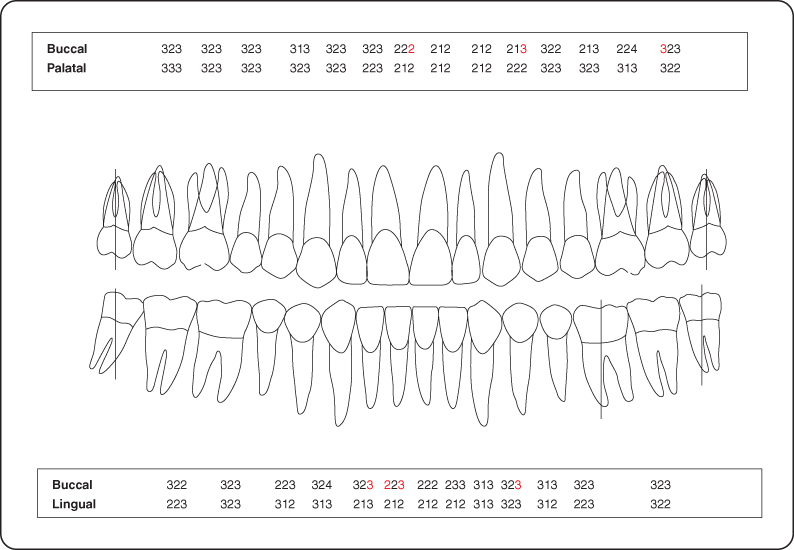
Figure 4: Probing pocket depth measurements.
Intraoral Examination
- There was no lymphadenopathy and oral cancer screen was negative.
- There was an adequate band of attached gingiva. Stippling was present.
- A hard tissue and soft tissue examination was completed (Figures 4–6).
Figure 5: Occlusal view of the maxillary arch.

Figure 6: Occlusal view of the mandibular arch.

Occlusion
The patient presented normal molar relationship and no interference in excursive movements (Figure 7).
Figure 7: Normal molar occlusal relationship.

Radiographic Examination
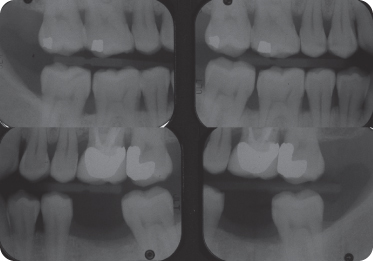
There were no caries or significant crestal bone loss seen on examination of the bite-wing radiographs (Figure 8).
Figure 8: Bite-wing radiographs depicting the interproximal bone levels.
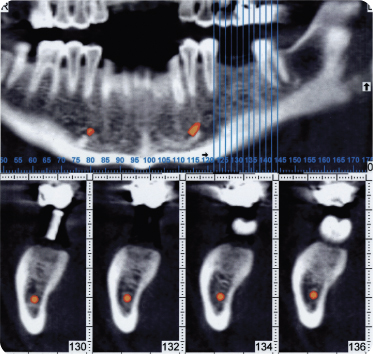
A computer tomographic (CT) image (Figure 9) revealed the presence of available bone >15 mm in height and sufficient width for wide diameter implant placement. Therefore no bone graft was necessary for implant placement (Figure 9).
Figure 9: CT radiographs reveal sufficient bone available for implant placement without bone graft. Radiographic guide is placed at the site of implant surgery for planning.
Diagnosis
The patient had partial edentulism and was diagnosed as American Dental Association type I due to gingivitis.
Treatment Plan
The treatment plan for this patient includes an initial phase of scaling with polishing and implant-supported porcelain fused to metal (PFM) crown for the area of #19.
Treatment
After the consult and diagnostic phase, the patient received initial therapy of scaling and polishing. The patient was able to maintain good oral hygiene in follow-up visits. Study models of maxillary and mandibular arch were fabricated to evaluate adequate spacing of area #19. The mesiodistal space of missing molar #19 area was compatible with the contralateral molar. A radiographic template was fabricated before sending the patient for CT evaluation. The CT revealed adequate quantity of bone and healing of extraction site with normal pattern of trabeculation.
The patient refused the alternative treatment option of a three-unit fixed partial denture #18-X-20 because the virgin abutment teeth would require preparation. A step-by-step description of implant therapy was discussed including possible complications. A consent form was obtained prior to the procedure.
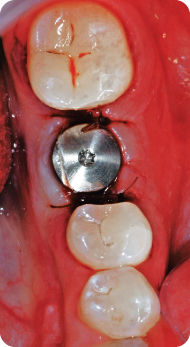
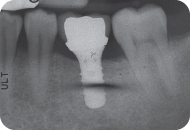
On the day of the procedure, the patient’s blood pressure was measured, and it was in a similar range of hypertensive level as the initial visit. Local infiltration anesthesia was given in the surgical area with lidocaine 2% (epinephrine 1:100,000). A full-thickness flap was raised after midcrestal incision. A surgical template was used to guide sequential drilling with copious irrigation to prepare the site for implant placement (Figure 10). One-stage implant of 4.8 × 10 mm and a wide neck platform for prosthesis connection was placed (Figure 11). The implant was clinically stable and a short healing abutment was screwed in (Figures 12 and 13). A periapical radiograph confirmed appropriate implant angulation and a safe distance from the inferior alveolar nerve. Flaps were sutured for primary closure. Minimum bleeding was observed before the patient left. Postoperative instructions were given. The patient received prescriptions for pain medication and an oral rinse.
Figure 10: A surgical template was used to guide angulations of drills.
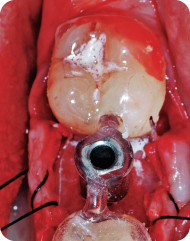
Figure 11: A wide diameter implant was placed in the molar region.
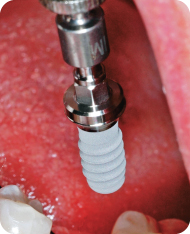
Figure 12: Implant placed in the molar area with appropriate angulation and distance from adjacent teeth.
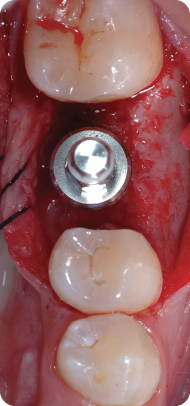
Figure 13: A short healing abutment placed and sutured for primary closure.
One week later, sutures were removed and soft tissue was healing normally. Minimum postoperative discomfort was reported.
The prosthetic phase of the case was initiated 2 months after the surgery. An impression coping was attached for closed final impression using polyether. An appropriate shade was selected for porcelain fabrication. The favorable implant position allowed for selection of a prefabricated straight abutment (Figure 14).
Figure 14: A straight prefabricated final abutment was used for restoration.

Four weeks after the final impression, final implant-supported PFM was cemented (Figure 15). A periapical radiograph was taken as a baseline for future reference. Oral hygiene instruction was reinforced and the patient was scheduled for recall visit every 6 months.
Figure 15: Final implant-supported PFM was delivered.

Figure 16: Postoperative periapical radiograph.
Discussion
Implant-supported restorations have become routine treatment in dental practice with predictable outcome and a high success rate [1]. However, the prevention aspect should be emphasized with patients so loss of tooth due to caries or periodontal disease may be minimized. Effective oral home care including fluoride with periodic professional visits is crucial for appropriate prevention and early detection of oral disease.
The initial therapy of oral prophylaxis and compliance of oral home care is an important factor before considering implant therapy [2]. Once the implant option is chosen, study models and radiographic images are used as part of the planning. The planning should be done with the final outcome in mind. Various radiographic examinations may be prescribed such as conventional two-dimensional (2D) panoramic or computer tomography, which has the advantage of three-dimensional analysis of anatomic structures with minimum distortion [3]. When the radiographic template has the appropriate angulation, the same device may be used as a surgical template. If incorrect angulation is detected in the radiograph, appropriate modification should be made before the surgery.
In radiographic analysis, important anatomic structures should be identified. Ideally in the maxilla, implants should not penetrate the maxillary sinus space. In the mandible, the apex of implants should be 2 mm away from the inferior alveolar nerve or the mental foramen. Convergence of roots should be also be evaluated, especially in patients with a history of orthodontic treatment to avoid damaging root structure during implant placement. Implant diameter is selected to give appropriate support and emergence profile for the size of the crown. However, there should be a space of approximately 2 mm from implant to root surface [4].
Once the implant is placed, a certain period of time is necessary for healing and osseointegration. Branemark originally suggested a healing time of 4 months for the mandible and 6 months for the maxilla [5]. Recent advances in bone biology and implant designing have allowed a shortening of the waiting time from implant placement and final delivery of crown with predictable results [6]. In limited cases, it is also possible to extract the tooth, place the implant, and restore it all in the same day [7].
After final delivery of the restoration, the patient should be in strict recall protocol for professional oral hygiene and radiographic reevaluation.
Self-Study Questions
A. Is there any age limitation to place a dental implant?
B. What kind of radiographs could be ordered for an implant case planning?
C. What are the advantages and disadvantages of implant treatment compared with conventional fixed-partial denture (FPD)?
D. What is the difference between the one-stage and two-stage implant approach?
E. What are the possible postoperative complications in the short and long term?
Answers located at the end of the chapter.
References
1. Adell R, Eriksson B, et al. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants 1990;5:347–e59.
2. Wennström JL, Ekestubbe A, et al. Oral rehabilitation with implant-supported fixed partial dentures in periodontitis-susceptible subjects. A 5-year prospective study. J Clin Periodontol 2004;31:713–724.
3. Harris D, Buser D, et al; European Association for Osseointegration. E.A.O. guidelines for the use of diagnostic imaging in implant dentistry. A consensus workshop organized by the European Association for Osseointegration in Trinity College Dublin. Clin Oral Implants Res 2002;13:566–570.
4. Buser D, Martin W, et al. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants 2004;19:43–61.
5. Branemark PI, Hansson BO, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl 1977;16:1–132.
6. Bornstein MM, Schmid B, et al. Early loading of non-submerged titanium implants with a sandblasted and acid-etched surface. 5-year results of a prospective study in partially edentulous patients. Clin Oral Implants Res 2005;16:631–638.
7. Misch CE, Hahn J, et al. Workshop guidelines on immediate loading in implant dentistry. Immediate Function Consensus Conference. J Oral Implantol 2004;30:283–288.
8. Op Heij DG, Opdebeeck H, et al. Age as compromising factor for implant insertion. Periodontol 2000 2003;33:172–184.
9. Park SH, Wang HL. Implant reversible complications: classification and treatments. Implant Dent 2005;14:211–220.
TAKE-HOME POINTS
A. There is no upper age limit for implant placement as long as the patient fulfills the prerequisites for general surgery. However, an implant placed in a young patient may work as an ankylosed structure and interfere with the growth of facial bones [8]. In general, growth spurt occurs at the age of 12 years for girls and 14 for boys. However, the craniofacial/skeletal growth may continue further, and individual variation could be up to 6 years of difference. Therefore the chronological age is not sufficient to estimate growth cessation. A more reliable test would be superimposing tracings of cephalometric radiographs taken at least 6 months apart and determining the growth cessation.
B. Bite-wing, periapical, and panoramic radiographs are the most common radiographic techniques in the dental setting. Bite wing is not appropriate for implant planning because it only shows a limited range of the crestal bone area. A periapical radiograph may be used in limited cases, but it may fail to show anatomic sites such as the maxillary sinus and inferior alveolar nerve. Panoramic radiograph has the advantage of showing a large area, but it has greater distortion than a periapical radiograph. Because it is a superimposed 2D image, bone width cannot be determined. The CT scan is the ideal radiograph for planning since it is a three-dimensional image with minimum distortion. CT images can also be applied to software to fabricate computer-generated surgical templates.
C. The greatest advantage of a dental implant is that the preparation of neighboring teeth is avoided. The physiological stimulation to the alveolar bone through the dental implant also prevents further bone loss. In cases where distal abutment is absent, a dental implant may be the only alternative to deliver a fixed prosthesis option. However, treatment length for an implant may be longer compared with conventional FPD, and patients may reject the idea of having surgical intervention, especially when it requires the additional steps of bone grafting.
D. Traditionally, implants were designed to be closed with the soft tissue at the time of implant placement. After a period of healing, implants would be uncovered by placing a healing abutment at the second stage. This two-stage approach would require a second surgical intervention and further waiting time for soft tissue maturation.
Other implants are designed with a longer neck; therefore soft tissue would be adapted around it instead of covering the implant at the time of placement. This one-stage approach eliminates the necessity of a second surgical intervention to expose the implant. Two-stage designed implants can be used as one-stage approach by inserting a healing abutment at the time of implant placement.
E. Some of the intraoperative surgical-related complications are as follows [9]:
- Damage of adjacent teeth
- Lack of primary stability
- Hemorrhage
- Nerve injury
- Penetration of sinus floor
- Fracture of mandible
Careful planning and knowledge of anatomy are important to avoid these types of complications. Minor complications such as a small perforation of sinus floor may not require removal of implants, and antibiotics and a decongestant may help to avoid complications. Complications such as nerve injury and fracture of the mandible require immediate removal of implant, and further treatment should be considered.
These are the postoperative surgical-related complications:
- Incision line opening
- Prolonged pain
- Fistula and abscess
- Peri-implantitis
Even if sutures are loosen earlier that expected, it may not require resuturing. If pain persists longer than usual period, the dentist should suspect overheating during drilling preparation or carefully evaluate f/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


