5
Mucogingival Therapy
Case 1: Pedicle Flaps
N. Joseph Laborde III, DDS, and Kasumi Kuse Barouch, DDS, PhD
Case 2: Connective Tissue Grafts
Ronny S. Taschner, DDS, and Jennifer F. Taschner, DDS, MMSc
Case 3: Free Gingival Grafts
Ronald M. Fried, DMD, MMSc, and Maria Dona, DDS, MSD
Case 4: Treatment of Mucogingival Deformities Using Alloplastic Materials
Helen Livson, DMD, MMSc, and Sarah D. Shih, DDS, MS, DMSc
Case 5: Frenectomy and Vestibuloplasty
Daniel Kuan-te Ho, DMD, MSc, Satheesh Elangovan, BDS, DSc, DMSc, and Sarah D. Shih, DDS, MS, DMSc
Case 1
Pedicle Flaps
CASE STORY
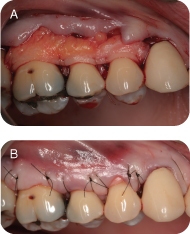
A 32-year-old Caucasian female presented with a chief complaint of: “my lower front teeth are sensitive.” She reported experiencing sensitivity of her lower teeth when drinking hot and cold liquids. She also expressed concern about the appearance of her lower gums. Her general dentist had referred her for periodontal treatment of her gingival recession (Figure 1).
LEARNING GOALS AND OBJECTIVES
- To be able to diagnose mucogingival defects and deformities
- To identify the possible etiology for gingival recession
- To understand which surgical techniques should be applied to correct gingival recession defects
Medical History
There were no significant findings in reviewing the patient’s medical history. She did not report taking any medications or supplements. The patient reported having no known drug allergies. She had had an annual physical with her primary care physician.
Review of Systems
- Vital signs
- Blood pressure 121/70 mm Hg
- Pulse rate: 70 beats/minute (regular)
- Respiration: 15 breaths/minute
Dental History
The patient reported that she saw her general dentist twice yearly for a cleaning and checkup. She had received orthodontic treatment as a teenager to correct crowding of her maxillary and mandibular arches. She reported brushing twice daily with a medium-bristle toothbrush. The patient tried to floss daily but sometimes she forgot.
Social History
The patient had been born and raised in Massachusetts. She currently resided in Boston with her husband and 4-year-old daughter. The patient was a high school English teacher. She reported drinking alcohol socially and had between one and three drinks per week and denied the use of tobacco products.
Extraoral Examination
The patient had no detectable lesions, masses, or swelling, and the temporomandibular joint was within normal limits.
Intraoral Examination
There were no detectible masses or lesions of the tongue, floor of the mouth, hard/soft palate, or buccal mucosa. Oral cancer screening was negative.
Hard Tissue Examination
The patient had no carious lesions. The restorations were intact on radiographic and clinical examination.
Periodontal Examination
- The full-mouth charting revealed probing depths of 1–3 mm with some bleeding on probing in the posterior quadrants.
- Mild gingival inflammation was present in the posterior quadrants adjacent to the second molars.
- An isolated recession defect was present on tooth #24 measuring 3 mm from the cementoenamel junction (CEJ).
- There was a minimal amount of attached keratinized tissue adjacent to the recession defect with mild localized marginal inflammation.
Occlusion
There were no occlusal discrepancies or interferences.
Radiographic Examination
- A recent full-mouth series revealed no carious lesions or pathologic findings.
- The bone levels appeared to be within normal limits with intact crestal lamina dura.
Diagnosis
According to the American Academy of Periodontology the patient’s gingival condition is classified under developmental or acquired deformities and conditions [1]. It is further grouped into mucogingival deformities and conditions around teeth with gingival/soft tissue recession and a lack of keratinized gingiva.
The recession defect can be classified according to the Miller Classification System of gingival recession defects [2]. This defect is a Miller class 1 because it does not extend beyond the mucogingival junction and there is no interproximal bone loss. For a more in-depth discussion of classification of gingival recession, refer to Chapter 5, Case 3.
Treatment Plan
The proposed treatment plan for this patient is a dental prophylaxis including oral hygiene instructions. After establishing proper home care, the recession will be treated with a pedicle graft to repair the isolated gingival defect.
Discussion
Prior to treatment of gingival recession it is important to identify the possible etiology of the defect. The patient received orthodontic treatment, which can result in gingival recession if the teeth are moved labially beyond their bony housing. The patient also has a thin biotype, which is characterized by a thin scalloped gingiva and buccal plate that make the patient more prone to recession [3]. Improper toothbrushing technique such as overzealous brushing with a medium or hard-bristle toothbrush, can also lead to gingival recession. Once a dental prophylaxis was completed and the patient demonstrated the ability to maintain proper oral hygiene, the treatment of the recession defect could proceed.
In this case the desired treatment outcome was to achieve root coverage and increase the width of attached tissue around tooth #24. After considering the possible treatment options, the decision to use a laterally positioned pedicle graft was made. (Refer to question D to review indications for laterally positioned pedicel graft.)
The lateral pedicle graft was performed under local anesthesia with no complications. (See question C for a step-by-step guide to the procedure.) The patient was seen for postoperative appointments at 2, 4, and 6 weeks. At 6 weeks there is almost full root coverage with an increase in the amount of attached keratinized tissue around #24. The patient also reported a decrease in sensitivity in her lower front teeth (Figure 2).
Self-Study Questions
A. What is a pedicle graft?
B. What are the surgical techniques that use pedicle grafts for root coverage?
C. How is a laterally positioned pedicle flap performed?
D. What are the indications/contraindications for using these techniques?
E. What are the benefits/limitations of using pedicle flaps compared with free autogenous grafts?
F. How else can pedicle flaps be used in the oral cavity?
Answers located at the end of the chapter.
References
1. Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol 1999;4:1–6.
2. Miller PD Jr. Root coverage using the free soft tissue autograft citric acid application. III. Int J Periodontal Rest Dent 1985;2:6,15.
3. Ochenbein C, Ross S. A reevaluation of osseous surgery. Dent Clin North Am 1969;13:87–102.
4. Grupe HE, Warren RF Jr. Repair of gingival defects by a sliding flap operation. J Periodontol 1956;27:92.
5. Cohen DW, Ross SE. The double papillae repositioned flap in periodontics. J Periodontol 1968;39:65–70.
6. Harris R. The connective tissue and partial thickness double pedicle graft: a predictable method of obtaining root coverage. J Periodontol 1992;63:447–486.
7. Mariotti A. Efficacy of chemical root surface modifiers in the treatment of periodontal disease. A systematic review. Ann Periodontal 2003;8:205.
8. Rose LF, Mealy BL, et al. Periodontics Medicine, Surgery and Implants. Philadelphia, PA: Mosby, 2004. Chapter 21 p432.
9. Rose LF, Mealy BL, et al. Periodontics Medicine, Surgery and Implants. Philadelphia, PA: Mosby, 2004. Chapter 21 pp432–434.
10. Wennstrom JL. Mucogingival therapy. Ann Periodontol 1996;1:671–701.
11. Fugazzotto PA. Maintenance of soft issue closure following guided bone regeneration: technical considerations and report of 723 cases. J Periodontol 1999;70:1085–1097.
12. Nemcovsky CE, Zvi A, et al. Healing of dehiscence defects at delayed-immediate implant sites primarily closed by a rotating palatal flap following extraction. Int J Oral Maxillofac Implants 2000;15:4.
TAKE-HOME POINTS
A. A pedicle graft (also called pedicle flap) is a full- or split-thickness flap designed in such a way that it remains connected at its base. The flap can then be rotated or positioned at an adjacent location while still maintaining its own blood supply through its connection. The blood supply nourishes the graft and facilitates the vascular union with the recipient site. This differs from a free autogenous tissue graft that is completely severed from its blood supply but can be attached to another part of the oral cavity.
B.
1. Laterally positioned flap: This technique, first described by Grupe and Warren in 1956, uses donor gingiva from a healthy tooth to cover the exposed root of an adjacent tooth [4].
Double papilla flap:
2. Double papilla flap: This technique, described by Cohen and Ross in 1968, is used to cover defects where there is an inadequate amount of gingival on the adjacent area for a laterally positioned flap [5]. In this method, the papillae from each side of the problem tooth are reflected and rotated over the midfacial aspect of the recipient tooth and sutured. Harris described a modification of this technique by placing a subepithelial connective tissue graft under the double pedicle flaps [6].
Coronally positioned flap:
3. Coronally positioned flap: This technique can be used when there is an adequate amount of keratinized tissue and thickness of gingiva adjacent to the recession defect. The gingiva is released and advanced coronally to cover the recession defect. The procedure can be performed with or without vertical releasing incisions and it is often used in combination with other mucogingival techniques.
C. Before beginning the procedure, the bone level on the facial of the donor site should be evaluated with bone sounding. If the distance from the bone to the CEJ is >2 mm, there is a risk of recession on the donor tooth. Leaving a collar of tissue at the donor site can reduce this risk. The root surface where coverage will be attempted should be thoroughly planed and smoothed to remove surface irregularities or defects. Some practitioners might use chemicals such as EDTA, citric acid, or tetracycline to condition the root surface. However, there is no definitive evidence in humans that chemically treated roots are more biologically acceptable than mechanically prepared surfaces for soft tissue grafting [7].
The first incisions are made to prepare the recipient site for the donor tissue. An incision starting in the papilla between the donor and recipient site is made from the level of the CEJ continuing at an oblique angle beyond the base of the defect. A small horizontal incision at the level of the expected root coverage is made on the opposite side of the recipient site and then extended apically to meet the first incision. The epithelium between these incisions is removed in preparation to receive the pedicle graft.
The next incision is made from the line angle of the tooth adjacent to the donor site and extended parallel to the first incision. The following incision extends across the donor site connecting the first and third incision. This incision can be sulcular, or if there is a concern of recession, this incision can be made so a collar of tissue remains. The tissue collar should have at least 0.5 mm of attached tissue (Figure 3).
The flap is reflected with a split-thickness dissection. Full-thickness dissection may be necessary in some portions to maintain adequate flap thickness and prevent perforations. The flap can now be mobilized and rotated to the recipient site. If there is tension on the flap at the recipient site, additional release of the tissue may be done (Figure 4).
Once the pedicle flap is in the correct position and tension free, it is sutured in place using 5-0 or 6-0 simple interrupted sutures. The leading edge of the flap is secured first with sutures in the papilla and mucosa. The trailing edge is secured with a suture in the papilla. If there is periosteum left intact from the split-thickness dissection, additional sutures can be placed to stabilize the flap (Figure 5).
The graft should be stable and immobile, which can be confirmed by movement of the lip. If desired, a periodontal dressing can be applied to the area [8].
D. Indications for the use of pedicle grafts for root coverage include the following [9]:
1. An isolated area of recession with no bone loss on the proximal surface.
2. A donor site with adequate soft tissue width and thickness, sufficient vestibular depth, and adequate bone thickness with no dehiscence.
Contraindications for the procedure include the following:
1. A donor site with thin tissue is not recommended because it is prone to future recession.
2. If the distance from the crest of bone to the CEJ on the facial surface of the donor tooth is >2 mm, there is a risk of recession after the tissue is rotated.
E.
1. There is only one surgical site with a pedicle graft (palatal donor site not needed), which limits the risk of postoperative morbidity.
2. The pedicle maintains its own blood supply, which increases the chance for graft survival and root coverage.
3. There is a harmonious blend of tissue color and contour after healing compared with free autogenous tissue grafts that can have less aesthetic results.
4. It is more difficult to treat multiple teeth using pedicle grafting techniques compared with free autogenous grafts, which can be harvested according to the size needed.
5. There is less risk of recession from the donor site of free autogenous grafts compared with pedicle flaps.
6. Root coverage is less predictable using pedicle grafting techniques with a mean root coverage of 62.5% for laterally positioned or double papilla flaps. The mean root coverage for connective tissue grafts in combination with various flap techniques is 89.3% [10].
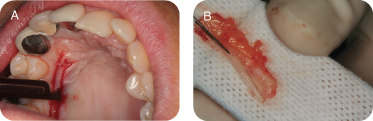
F. A variety of surgical techniques using pedicle grafts are described in the dental literature. Fugazzotto reported a technique using a rotated palatal pedicle graft to help obtain primary closure in guided bone regeneration procedures [11]. After palatal reflection, a layer of connective tissue is dissected away from the base (apical) of the flap while maintaining its connection at the coronal portion. This method helps achieve tension-free primary closure over the grafted site. Nemcovsky et al have demonstrated a technique that uses rotated palatal tissue to achieve primary tissue closure over extraction sites [12]. They reported the use of full- and partial-thickness rotated palatal flaps to cover extraction sites as well as coverage of immediate implants placed in the maxilla. In the technique demonstrated here, a subepithelial connective tissue graft is harvested adjacent to and one tooth distal to the extraction site. This graft is rotated to cover the grafted extraction site while maintaining its attachment adjacent to the area. This technique helps achieve primary closure to aid in the formation of adequate bone and soft tissue formation (Figures 6–8).
Figure 7: Allograft placed in extraction socket and connective tissue rotated under sulcular tissue on palate.
Courtesy of Kasumi Barouch, DDS.
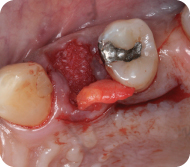
Figure 8: Connective tissue sutured in place while maintaining connection at base of graft.
Courtesy of Kasumi Barouch, DDS.
Case 2
Connective Tissue Grafts
CASE STORY
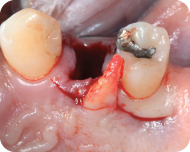
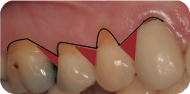
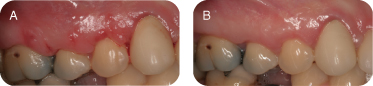
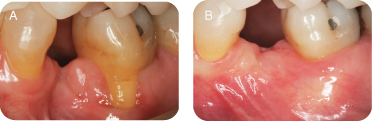
This patient was a 36-year-old male whose general dentist had noticed the recession on teeth #3, 4, and 5 was progressing and had referred him to a periodontist. The dentist had also been concerned with the cervical abrasion/erosion, lack of keratinized tissue, and associated frenum close to the gingival margin on tooth #5 (Figure 1).
Figure 1: Preoperative clinical presentation.

LEARNING GOALS AND OBJECTIVES
- To identify the indications and rationales for soft tissue grafting
- To understand the surgical technique for subepithelial connective tissue grafting including:
- Zucchelli incision designs and technique for multiple recession sites.
- Root preparation
- Harvesting of donor tissue
- Suturing of graft and flap
- To understand the rationale for root preparation
- To understand the presurgical and postsurgical considerations
Medical History
The patient’s medical history was not significant. The patient was not taking any medications and denied having any allergies.
Review of Systems
- Vital signs
- Blood pressure: 128/76 mm Hg
- Pulse rate: 68 beats/minute
- Respiration: 14 breaths/minute
Social History
The patient admitted to smoking cigarettes as a young adult but had not smoked for at least 10 years. He denied using chewing tobacco. He was a social drinker and admitted to drinking one or two alcoholic beverages three to four times a week.
Dental History
The patient had received fairly regular dental care throughout most of his childhood and adult years, with periodic cleanings and examinations approximately every 6 months. He had had orthodontic care as a teenager; treatment lasted approximately 2 years.
Oral Hygiene Status
The patient brushed his teeth three to four times a day, using a medium or soft brush, and admitted to brushing somewhat “aggressively.” He flossed three to four times a week.
Family History
One of his parents had been treated for recession, but both parents had all or most of their own teeth.
Extraoral Examination
No significant findings were present.
Intraoral Examination
- Oral cancer screening was negative. Soft tissues including buccal mucosa, hard and soft palate, floor of the mouth, and tongue all appeared normal.
- There was generally an adequate amount of attached keratinized gingiva present on all remaining teeth (Table 1).
- The patient had excellent oral hygiene with a minimal amount of plaque accumulation and gingival inflammation.
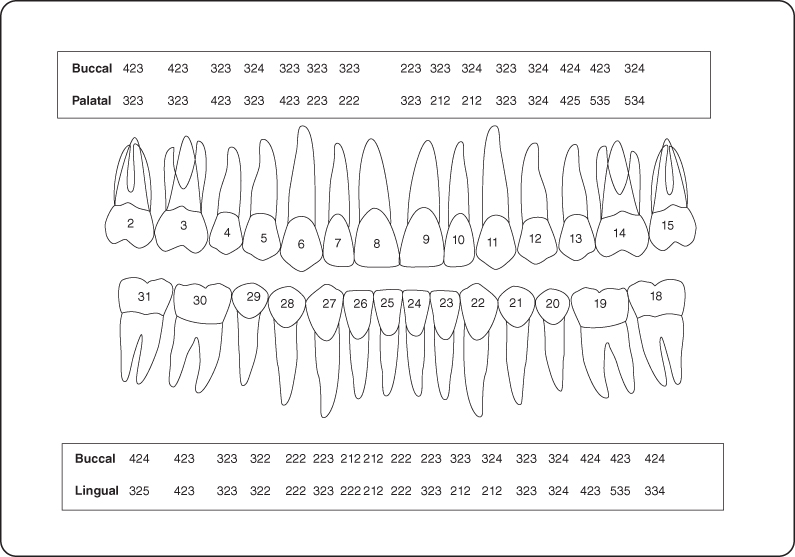
- See Figure 2 for periodontal charting.
- There was some mild clinical attachment loss with no probing depths >3 mm, no tooth mobility, and no furcation invasion.
- Tissue color, contour, and consistency: Generalized pink color with normal contour except for recession as noted below. Consistency was firm with normal stippling.
- Bleeding on probing was localized and very slight.
Table 1: Keratinized/Attached Gingiva
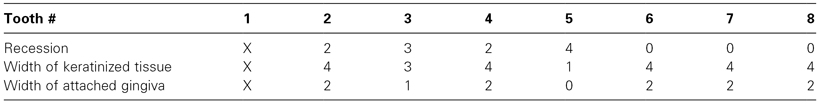
Figure 2: Probing pocket depth/recession measurements during initial visit.
Radiographic Examination
There was no bone loss evident on radiographic examination.
Diagnosis
- Recession with inadequate attached gingiva, localized #3 and 5.
- Cervical abrasion/erosion, #3–5.
Treatment Plan
- Oral hygiene instructions to modify traumatic brushing technique
- Subepithelial connective tissue graft, #3, 4, and 5.
Treatment
After evaluation of the thickness and anatomy of the palate by “sounding,” administration of local anesthetic, and evaluation of the amount of keratinized tissue present on the facial of teeth #3–5, treatment of #3–5 with a SCTG using the right palate as a donor site was recommended.
A decision was made to reposition the overlying flap coronally to completely or almost completely cover the graft. Because there was still a small width of keratinized tissue on #5 and 2–3 mm of keratinized tissue on #2, 3, and 4, the cosmetic result would be better than it would be if several mm of CT was left exposed.
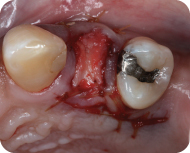
With the Zucchelli technique (Figure 3), the incisions are made at an angle extending from the cementoenamel junction (CEJ) of one tooth to the height of the recession on the adjacent tooth. Where multiple teeth are involved, a tooth in the middle is designated and the incisions are angled apically from the mesial and distal at the level of the CEJ to the height of recession of the tooth to the mesial and to the tooth to the distal.
Figure 3: Zucchelli technique.
The purpose of this design is to (1) avoid vertical releasing incisions, and (2) create papillary shapes that, when coronally repositioned, will rotate mesially or distally and cover the deepithelialized papillae and the underlying CT graft.
In this case, tooth #5 was selected (Figure 4A), and Zucchelli incisions were made mesial and distal starting at the CEJ. Additional incisions were made starting at the distal CEJ of #4, angling to the apical extent of the recession of #3. Another similar incision was made starting at the distal cervical of tooth #3.
Figure 4: (A) Initial incisions; (B) reflection; (C) deepithelialization of the papillae.
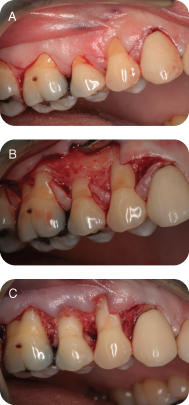
A partial-thickness flap was reflected (Figure 4B), freeing the flap apically to allow the flap to easily be coronally repositioned. To avoid perforating the flap with sharp dissection, it may be necessary to elevate carefully over any exostoses.
The papillae are carefully deepithelialized (Figure 4C) using a 12b scalpel blade. The amount of tissue removed is approximately ≤1 mm, leaving as much of the underlying connective tissue papilla as possible.
Root Preparation
Root plane to smooth the roots and remove or round out” any grooves, at times creating a saddle shape (Figure 5). It may be necessary to use a high-speed handpiece lightly and carefully with football-shaped finishing burs, medium, fine, and extrafine diamonds if the grooving on the root is severe or if an existing restoration needs to be removed.
Chemically treat the root with EDTA solution 17% (Pulpdent) for 2 minutes by applying saturated cotton pellets or burnishing with a saturated cotton pellet for 45 seconds (Figure 6).
Figure 5: Root planing.

Figure 6: Application of EDTA solution.

After measuring the length of graft needed to cover the roots, mark the approximate positions at the beginning and end of the graft on the palate with the point of the probe.
Make the first incision 4 mm from the gingival margin. Make the second incision 1–2 mm closer to the tooth and parallel to the first incision (Figure 7A).
Figure 7: (A) Harvesting of the graft; (B) trimming of the graft.
The depth of the incisions can safely extend 7 mm from the CEJ on a shallow palate, 12 mm on an average palate, and 17 mm on a high palate [1].
If the palate is thin, it may be necessary to elevate the graft form the palatal bone instead of making a second incision.
At the apical extent of the incision, angle the scalpel toward the palate to free the graft. Do the same at the mesial and distal borders of the graft.
Remove the epithelium by trimming it with a sharp scalpel (Figure 7B).
Suturing
Suture the graft with individual sling sutures using 5-0 chromic gut suture. Tie on the lingual, if possible, to allow for better flap to graft contact (Figure 8A). Suture the flap with 6-0 monofilament nylon or Gore CV-6 suture. Use one sling suture per tooth (Figure 8B).
Figure 8: (A) Suturing of the connective tissue graft; (B) suturing of flap.
Enter the flap from the facial about 3 mm from the gingival margin, approximately at the mesial line angle of the tooth. Proceed interproximally, not engaging the interproximal connective tissue papilla but going coronal to it, wrapping around the lingual, passing through the distal embrasure to the facial, again keeping the suture coronal to the papilla. Pass the suture needle through the facial flap 3 mm apical to the gingival margin at the distal line angle, pass through the distal embrasure coronal to the papilla, wrap around the lingual to the mesial embrasure, pass through it, and tie the suture on the facial. Repeat for each tooth. Also place a sling suture to secure the gingival flap one tooth mesial and one tooth distal to the graft.
Postoperative Instructions
- Ice the area for 24–48 hours, 20 minutes on and 20 minutes off
- Sleep on back with head slightly elevated
- Rinse with chlorhexidine 0.12% rinse bid
- Avoid brushing or flossing for 2–4 weeks
- Eat a soft diet and try to avoid eating on the side of the surgery
- After 2 weeks can use an ultra-soft brush to gently remove debris with roll technique
Prescriptions
- Motrin 800 mg: 1 tablet tid starting 1 hour before procedure
- Vicodin 5/500: 1–2 tablets every 4–6 hours as needed for pain
- Doxycycline: 100 mg. 1 tablet bid day of surgery, then 1 tab every day for 10 days
- Chlorhexidine rinse 0.12%: rinse for 30–60 seconds bid
Postoperative Follow-up
Patients should be seen 7–14 days after the surgery to remove dressing/sutures (Figure 9A). Additional follow-up to observe patient home care and healing should be planned accordingly (Figure 9B).
Figure 9: (A) Suture removal at 2 weeks; (B) 8 weeks postsurgery.
Discussion
Indications
The need for an adequate band of attached gingiva has been a topic in the periodontal literature for at least 50 years. It has been argued that without an adequate band of attached gingiva, the stability of the gingival margin would be at risk with the potential for further attachment loss, recession, pocket formation, and inflammation.
The amount of attached gingiva needed to prevent further recession and attachment loss has also been debated and is unclear. Early papers suggested that 5–6 mm of keratinized tissue with a probing depth of 2–3 mm would result in a functional band of attached gingiva of 2–3 mm that was necessary to obtain stability of the marginal gingiva. Lang and Loe [2] stated that 80% areas ≥2 mm keratinized gingiva (KG) and 1 mm attached gingiva (AG) remained healthy while inflammation persisted in areas with <2 mm KG and 1 AG even with good oral hygiene. Several other studies found that areas with minimal width of KG were no more prone to inflammatory changes.
The 1989 World Workshop [3] concluded there were several parameters that should be considered when determining if an adequate zone of attached gingiva is present and the minimum amount of attached gingiva that is acceptable.
The American Academy of Periodontology Consensus Statement on Mucogingival Conditions [4] defines an inadequate amount of keratinized tissue as <2 mm of width, of which <1 mm is attached gingiva. It states that a minimal amount or absence of attached gingiva alone is not a justification for gingival augmentation. The presence of “recession, loss of supporting bone, absence or reduction of keratinized tissue, and probing depths extending beyond the mucogingival junction” must be considered as well as resulting “root sensitivity, loss of tooth structure (abrasion), increased length of the clinical crown, and inflammation and bleeding of the marginal tissue.” Ultimately, the clinician’s best judgment must be used to determine whether or not to treat mucogingival conditions [4].
With those considerations, gingival grafting to increase the width of attached gingiva may be indicated if there is <2 mm width of keratinized tissue in which <1 mm is attached gingiva, the recession is progressive, the gingival margin would be stressed by a restorative margin at or below the gingival margin, a removable partial denture would stress the gingival margin, orthodontic treatment is planned (and the teeth are to be moved labially), in progress or completed, or an inability to maintain the gingival margin free of inflammation, bleeding, and/or plaque accumulation [3]. Grafting for root coverage should also be considered when recession has resulted in root abrasion, root sensitivity, and/or compromised aesthetics.
There are several reasons for performing connective tissue grafts. These include areas where there is inadequate attached gingiva (Figures 10A and B), to improve aesthetics, decrease root sensitivity, improve cleansibility, and reduce the exposure of furcations (Figures 11A and B), stop progressive recession (Figures 12A and B), treat root wear/erosion/cervical abrasion (Figures 13A and B) cover exposed crown margins (Figures 14A and B), cover an exposed implant collar (Figures 15A and B), covering lingual recession (Figures 16A and B), and root coverage and ridge augmentation prior to a fixed bridge (Figures 17A and B).
Figure 10: (A,B) Inadequate attached gingiva with recession.
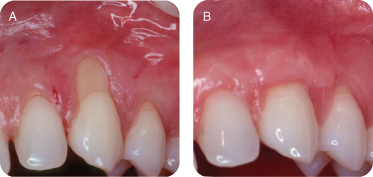
Figure 11: (A,B) Treatment with subepithelial connective tissue graft.
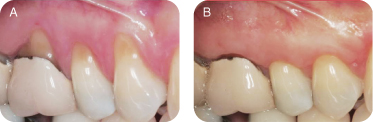
Figure 12: (A,B) Progressive recession.
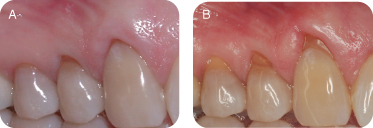
Figure 13: (A,B) Root wear/erosion/cervical abrasion.
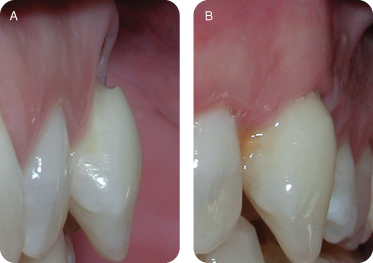
Figure 14: (A,B) Covering exposed crown margins.
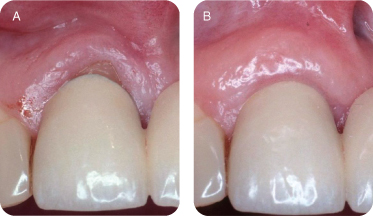
Figure 15: (A,B) Covering an exposed implant collar.
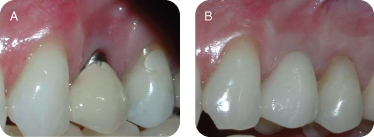
Figure 16: (A,B) Covering lingual recession.
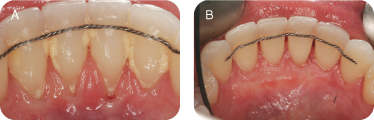
Figure 17: (A,B) Root coverage and ridge augmentation prior to a fixed bridge.
Treatment with subepithelial connective tissue graft can accomplish the following (see Figures 3 and 4):
- Improve aesthetics
- Decrease root sensitivity
- Improve cleansability
- Reduce exposure of furcations (improving long-term prognosis)
Techniques
The early procedures developed to augment the zone of attached gingiva included denudation of the bone, denudation of the periosteum, apically repositioned flap, and free gingival grafts. The bone denudation procedure produced a beautiful result but also caused attachment loss and significant morbidity, taking months to heal with the need to wear periodontal packing for most of the time. Leaving exposed periosteum decreased the bone loss, but the morbidly and healing period were still significant. Free gingival grafts, using the stratified squamous epithelium and the underlying connective tissue from the palate as donor material, decreased morbidity at the recipient site, but morbidity at the palatal donor site gave free gingival grafts an unpleasant reputation among patients.
All of these procedures were quite successful in creating adequate zones of attached gingiva and eliminating or minimizing the risk of further recession. However, these procedures were not indicated for root coverage, and there was little that could be done to correct the recession that often resulted in unsatisfactory aesthetics, root sensitivity, chemical erosion, mechanical abrasion, and caries. Pedicle flap procedures were developed and used successfully to obtain root coverage, but an adequate adjacent donor site was needed and not always available limiting the use of this procedure.
Root coverage with a free gingival graft was described by Holbrook and Ochsenbein [5] in 1983. The procedure required taking a rather large graft from the surface of the palate, often measuring 12–15 mm in the vertical dimension, and suturing the graft in place with a complex pattern of mattress sutures to closely adapt the graft to the root and periosteum apical and lateral to the root. Root coverage was fairly predictable with this procedure, but an acrylic appliance was needed to cover the donor area because of the large palatal wound. However, even with the best attempts at wound coverage, postoperative morbidity was prolonged.
The subepithelial connective tissue graft was developed by Langer and Langer [6] to create an increased zone of attached gingiva and to partially or completely cover roots, improving aesthetic outcomes, decreasing root sensitivity, covering areas of erosion and abrasion, and protecting the root from additional root wear.
The subepithelial connective tissue graft has become the standard of care for treatment of recession. The techniques used for subepithelial connective tissue grafts are varied, and well-publicized modifications of the Langer technique were developed by P. D. Miller [7], John Bruno, and Pat Allen, among others.
Conclusion
As the demand for aesthetics in dentistry has increased, subepithelial connective tissue grafts have increasingly become an integral component of periodontal therapy. Although the purest indication for soft tissue grafting is a lack of attached gingiva, indications for subepithelial connective tissue />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses