3
Resective Periodontal Therapy
Case 1: Gingivectomy
T. Howard Howell, DDS, and Maria Dona, DDS, MSD
Case 2: Preprosthetic Hard Tissue and Soft Tissue Crown Lengthening
Guillaume Campard, DDS, MMSc, and Emilio I. Arguello, DDS, MSc
Case 3: Flap Osseous Surgery
Kevin Guze, DMD, DMSc
Case 4: Root Resection
Philip M. Walton, DDS, and Paul A. Levi, Jr., DMD
Case 1
Gingivectomy
CASE STORY
A 16-year-old Caucasian male presented with a chief complaint of: “My gums are puffy and bleed on flossing.” After 2 years of orthodontic therapy, treatment had been discontinued 2 months before due to nonresolvable gingival enlargement (Figure 1). The patient had been informed of his gingival overgrowth, and oral hygiene instructions had been reinforced. The patient had no significant gingival inflammation and/or enlargement before the start of orthodontic treatment. He stated that the gingival enlargement developed gradually during orthodontic treatment (Figures 2 and 3).
Figure 1: Clinical presentation after removal of orthodontic appliances: smile frontal and side views.

Figure 2: Clinical example of plaque-induced gingivitis with gingival enlargement: frontal occlusal views before orthodontic presentation (top) and during the orthodontic treatment (bottom).

Figure 3: Clinical presentation 2 months after removal of orthodontic appliances: intraoral frontal view in occlusion.

LEARNING GOALS AND OBJECTIVES
- To learn the indications for gingivectomy
- To understand the surgical technique for gingivectomy
Medical History
The patient reported no significant medical problems and no known allergies. He did not have a family history of gingival overgrowth or a history of chronic or current medication.
Dental History
The patient reported that orthodontic treatment began 2 years ago to align his teeth. Slowly during this time, his gums became “puffy,” and despite his best efforts at oral hygiene no improvement had been achieved. Therefore, 2 months ago, the orthodontic brackets were removed and the patient was referred to the Department of Periodontology for consultation and appropriate treatment. The patient was currently wearing a retainer. He denied a history of tooth extraction, restorations, or endodontic treatment. The anatomic crown of tooth #8 was previously chipped due to trauma.
Social History
The patient was a sophomore in high school and denied smoking and drinking alcohol.
Oral Hygiene
The patient used a manual toothbrush that was replaced every 3 months and reported tooth brushing and flossing in the morning only. He also used Listerine mouth rinse once a day.
Extraoral and Intraoral Examinations
- There were no significant findings. The patient had no masses or swelling, and the temporomandibular joint was within normal limits.
- With the exception of the gingiva, the soft tissues of the mouth appeared normal.
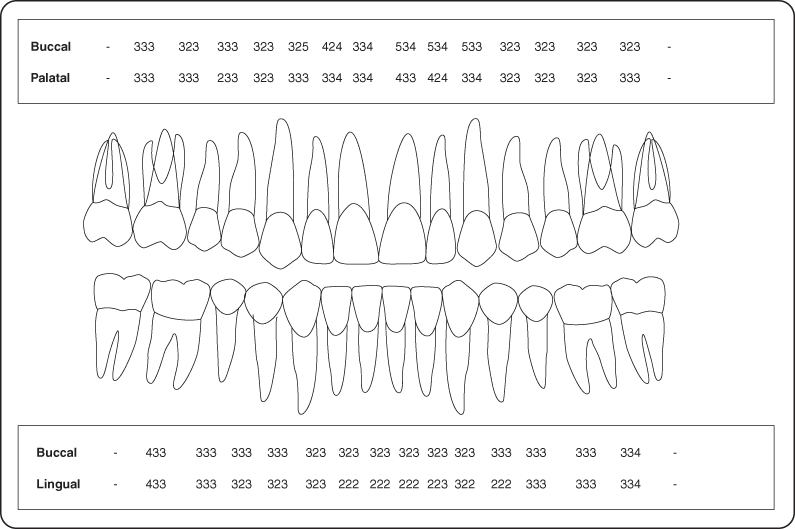
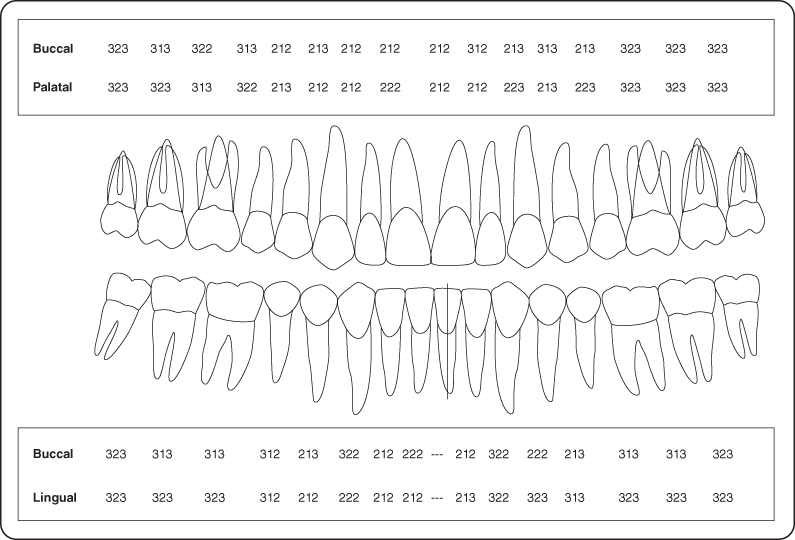
- A periodontal examination revealed localized mild marginal erythema, localized rolled margins, swollen papillae, bleeding on probing, no recession or mobility, probing depths ranging from 2 to 5 mm, and keratinized gingiva ranging from 3 to 8 mm (Figures 3 and 4).
- The hard tissue examination found no active decay and no dental restorations. Tooth #8 was reported as fractured.
Figure 4: Probing pocket depth measurements.
Occlusion
Class I angle occlusion was present after orthodontic treatment.
Radiographic Examination
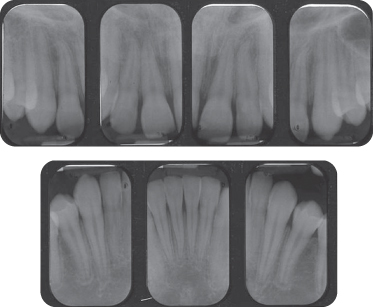
The full-mouth set of radiographs demonstrated crestal bone levels to be within normal limits (Figure 5 shows the patient’s anterior periapical X-rays).
Figure 5: Periapical radiographs depicting interproximal bone levels.
Diagnosis
After reviewing the history, clinical, and radiographic examinations, the patient was diagnosed with plaque-induced gingivitis resulting in gingival overgrowth.
Treatment Plan
The treatment plan for this patient included prophylaxis, improved oral hygiene, and surgical correction (with gingivectomy/gingivoplasty) of the gingival contour and periodontal maintenance.
Treatment
Treatment for this patient included oral hygiene instructions and supra- and subgingival scaling followed by reevaluation at 4 weeks. During the reevaluation appointment, an improvement in oral hygiene technique was noted. However, the gingival enlargement persisted. Therefore, surgical excision of excessive soft tissue was performed via external bevel gingivectomy technique (B). Following the administration of local anesthesia, bleeding points corresponding to the apical extent of the pocket depth were created on the external gingiva using a periodontal probe (Figure 6). Using #15C blades, a coronally directed external bevel incision was made starting slightly apical to the bleeding points and coronal to the mucogingival junction. The inner portion of the blade should contact the teeth at the base of the pocket at a position corresponding to the bleeding point. The incision line should be a straight-line incision that begins and ends in the gingival sulcus mesially and distally to the gingival area removed. The detached gingiva was removed with a scaler, and rotary diamond burs were used to reshape the gingival margin to normal physiologic contours, as shown in Figures 6 and 7. This reshaping of the gingival is referred to as gingivoplasty (A). Oral hygiene instructions were reinforced, and the patient was asked not to brush the wounded areas until the next appointment in 2 weeks and was given a prescription for Peridex rinse and ibuprofen 600 mg for pain control.
Figure 6: External bevel gingivectomy in anterior maxillary region; gingival marking for the external bevel incision (top) and immediately after gingivectomy (bottom).

Figure 7: External bevel gingivectomy in anterior mandibular region: immediate post-gingivectomy.

The patient was evaluated 2 weeks post-gingivectomy to assess the healing (Figure 8). Oral hygiene was reinforced, instructing on brushing the area of surgery.
Figure 8: Two-week post-gingivectomy: full smile frontal and side views.

Discussion
Patients undergoing orthodontic treatment may experience various oral clinical manifestations such as sensitivity, increased caries risk, and gingival enlargement [2,3]. Gingival enlargement associated with orthodontic therapy can begin as dental plaque–induced gingivitis followed by gingival overgrowth. The enlargement is usually associated with an inflammatory response triggered by the corrosion of the orthodontic appliances. The most likely component of the brackets creating this response is nickel. Therefore, the condition is frequently classified as nickel allergic contact stomatitis [1]. A recent study by Gursoy et al [2] describes the appearance of orthodontic treatment–induced gingival overgrowth as a specific fibrous and thickened gingiva, different from fragile gingiva with marginal gingival redness that is seen in allergic or inflammatory gingival lesions. The histologic analysis of orthodontic-induced gingival enlargement tissues demonstrated an increase in epithelial thickness and a significant increase in epithelial cell proliferation in response to low-dose nickel concentrations, and the in vitro results are suggestive of the continuing low-dose nickel release to epithelium as the initiating factor of gingival overgrowth induced by orthodontic treatment [2]). Complete resolution of gingival enlargement developed during orthodontic treatment may not appear even 3–12 months after the removal of the fixed appliances, as reported by Kouraki et al [3].
Therefore, because in the present case the gingival enlargement persisted 4 months after removal of orthodontic appliances and phase 1 therapy, including professional dental cleaning and reinforcement of home care dental hygiene, the surgical excision of excessive gingiva was planned and performed.
External bevel gingivectomy was performed using #15C blades and final reshaping of gingival contours using diamond burs. The postoperative follow-up showed excellent healing as well as a significant improvement in the aesthetic appearance that improved local access for proper oral hygiene. Similar results were described by Benoist et al [4] in two cases of gingival enlargement treated with gingivectomy in young Senegalese women undergoing orthodontic treatment with fixed appliances, with improvement in morphologic conditions of gingiva allowing better plaque control. The same authors emphasized that periodic evaluation of the child and adolescent during orthodontic therapy is required for healthy periodontium and that collaboration between orthodontist and periodontist is one of the most important keys to successful treatment.
Laser gingivectomy has been also pursued for the removal of excessive gingiva in the case of orthodontic treatment-associated gingival enlargement. In a study by Gama et al [5], the effect of the use of the CO2 laser on the treatment of gingival hyperplasia in orthodontic patients wearing fixed appliances was reported. This study concluded that the use of the CO2 laser was effective in the treatment of gingival hyperplasia. Additionally, the use of the Nd:YAG and diode laser in the surgical management of soft tissues related to orthodontic treatment, including recontouring of gingival overgrowth, was described in a study by Fornaini et al [6]. The laser-assisted surgery was particularly beneficial due to reported reduced bleeding during surgery with consequent reduced operating time and rapid postoperative hemostasis, thus eliminating the need for sutures, as well as improved postoperative comfort and healing, which make this technique particularly useful for very young patients [6].
In a comparative study of the histologic effects of scalpel, CO2 laser, electrosurgery, and constant-voltage electrosurgery, incisions were evaluated for mucosal incisions and excisions on a swine model [7]. The results of this study show that the speed of incisions and excisions was fastest with the scalpel and electrosurgery unit, the amount of bleeding was least for electrosurgery and CO2 laser, and the histologic damage was least with a scalpel, followed by constant-voltage electrosurgery.
ACKNOWLEDGMENT
The authors thank Dr. Athbi Alquareer, orthodontic resident at Harvard School of Dental Medicine, for referral and collaboration on the case presented in this chapter.
Self-Study Questions
A. What is gingivectomy/ gingivoplasty? What are the indications and contraindications for gingivectomy/gingivoplasty?
B. What are the surgical techniques for doing gingivectomy/gingivoplasty?
C. What is the oral hygiene protocol after gingivectomy?
D. What are the expected results and wound healing after gingivectomy?
Answers located at the end of the chapter.
References
1. Holmstrup P. Non-plaque induced gingival lesions. Ann Periodontol 1999;4:20–29.
2. Gursoy UK, Sokucu O, et al. The role of nickel accumulation and epithelial cell proliferation in orthodontic treatment-induced gingival overgrowth. Eur J Orthod 2007;29:555–558.
3. Kouraki E, Bissada NF, et al. Gingival enlargement and resolution during and after orthodontic treatment. N Y State Dent J 2005;71:34–37.
4. Benoist HM, Ngom PI, et al. Gingival hypertrophy during orthodontic treatment: contribution of external bevel gingivectomy. Case report. Odontostomatol Trop 2007;30(120):42–6.
5. Gama SK, De Araújo TM, et al. 2007 Use of the CO(2) laser on orthodontic patients suffering from gingival hyperplasia. Photomed Laser Surg 2007;25:214–219.
6. Fornaini C, Rocca JP, et al. Nd:YAG and diode laser in the surgical management of soft tissues related to orthodontic treatment. Photomed Laser Surg 2007;25:381–392.
7. Liboon J, Funkhouser W, et al. A comparison of mucosal incisions made by scalpel, CO2 laser, electrocautery, and constant-voltage electrocautery. Otolaryngol Head Neck Surg 1997;116:379–385.
8. Robicsek S. Ueber das Wesen und Entstehen der Alveolar-Pyorrhoe und deren Behandlung. 1884. The 3rd Annual Report of the Australian Dental Association (reviewed in J Periodontol 1965;36:265).
9. Grant DA, Stern IB, et al. Periodontics in the Tradition of Orban and Gotlieb. 5th ed. St. Louis, MO: Mosby.
10. Goldman HM. Gingivectomy. Oral Surg Oral Med Oral Pathol 1951;4:1136–1157.
11. Mavrogiannis M, Ellis JS, et al. The management of drug-induced gingival overgrowth [review]. J Clin Periodontol 2006;33:434–439.
12. Engler WO, Ramfjord SP, et al. Healing following simple gingivectomy. A tritiated thymidine radiographic study. I. Epithelialization. J Periodontol 1966;37:298–308.
13. Ramfjord SP, Engler SP, et al. A radiographic study of healing following simple gingivectomy. II. The connective tissue. J Peridontol 1966;37:179–189.
14. Listgarten M. Ultrastructure of the dento-gingival junction after gingivectomy. J Periodontal Res 1972;7:151–160.
15. Stahl SS, Witkin G, et al. Gingival healing II. Clinical and histologic repair sequences following gingivectomy. J Periodontol 1968;39:109–118.
TAKE-HOME POINTS
A. The gingivectomy procedure was first recognized by Robicsek [8] (straight incision technique) as an alternative surgical approach to subgingival scaling for pocket therapy. Grant et al later on [9] defined gingivectomy as “the excision of the soft tissue wall of a pathologic periodontal pocket” to eliminate the pocket and restore a physiologic gingival contour.
Gingivoplasty represents reshaping of the gingiva to a so-called physiologic form. Indications for gingivectomy/gingivoplasty are the following:
1. To eliminate gingival pockets – suprabony pockets – that persist after completion of oral hygiene instructions, scaling and root planning, and other disease control measures (Figures 3, 6, and 7)
2. To reduce gingival enlargements resulting from medications or genetic factors (Figure 9)
3. To create clinical crown length for restorative or endodontic purposes when ostectomy is not required (Figure 10)
4. To eliminate soft tissue craters resulting from disease or subsequent to other surgical procedures (Figure 11)
5. To create aesthetic gingival form in cases of delayed passive eruption
Figure 9: Clinical example of external bevel gingivectomy for phenytoin-induced gingival overgrowth. Frontal view in occlusion before gingivectomy (top left); external bevel gingivectomy in the anterior maxilla (top right); periodontal dressing applied at the end of gingivectomy (bottom left); 1 week after maxillary gingivectomy, after periodontal dressing removal (bottom right).

Figure 10: Clinical example of gingivectomy for restorative and aesthetic reasons. Smile at the initial presentation (top left); gingival marking using a vacuum-form template prior to gingivectomy (top right); delivery of temporary prosthesis at the end of gingivectomy (bottom left); smile at delivery of the final restoration #6–11, 5 months post-gingivectomy (bottom right).

Figure 11: Clinical example of an inverse bevel distal wedge. Palatal preoperative view (top left); outline of the initial scalloped incision and extended into the tuberosity region in a triangular shape (top right); osseous defect from the distal view after removal of the collar of tissue and distal wedge and thorough debridement (bottom left); the flaps positioned and sutured to gain primary closure (bottom right).

Contraindications to the performance of gingivectomy are as follows:
1. Acute inflamed gingiva
2. Inadequate oral hygiene
3. Inadequate keratinized gingiva: pocket depth is located apical to the mucogingival junction
4. Presence of interdental osseous craters and infrabony defects
5. Inadequate depth of vestibule
6. Presence of large exostoses and osseous ledges
7. When removal of the soft tissue would lead to an undesirable aesthetic compromise
8. In case of increased rate of caries that jeopardizes maintenance of dentition
B. Gingivectomy can be performed using the classical external bevel gingivectomy (as described by Goldman in 1951 [10]), internal bevel gingivectomy technique, or distal wedge procedures as well as by the use of electrosurgery, lasers, or chemical gingivectomy. Gingivoplasty can also be performed by using rotary instruments with appropriately shaped coarse diamond stones in addition to using the edge of a round-bladed gingivectomy knife.
External bevel gingivectomy (shown in Figure 6 for a case of dental plaque-induced gingivitis after orthodontic treatment and in Figure 9 for a case of phenytoin-induced gingival enlargement; the clinical case was previously detailed in Chapter 1, Case 4) consists of several steps:
- Pocket marking (placement of a series of bleeding points on the outside of the gingiva that correspond to apical extent of the pocket using either the periodontal probe or a mechanical device such as the Crane-Kaplan or Goldman-Fox pocket marker; usually three points are marked per tooth: mid-radicular area, mesial, and distal line angles)
- A primary coronally directed external bevel incision, of about 45 degrees, is next made using an appropriate surgical knife: broad-blade or round-blade gingivectomy knife such as the Goldman-Fox #7/8, or Kirkland #15K/16K, or #15/15C blade that starts slightly apical to the “dotted line” created by the bleeding points but always coronal to the mucogingival junction with an internal end point corresponding to the base of the pocket as indicated by the bleeding points
- A secondary interdental incision is made to sever the interproximal portion of the soft tissue pocket using a triangular narrow-blade knife such as the Goldman-Fox #8 or #11 or the Orban #1/2
- Removal of the excised soft tissue using a Prichard curette or any sharp universal curette provides a surface that is smooth and free of tags
- The exposed root surfaces are examined and instrumented to ensure proper and complete removal of calculus
- After debridement, refinement by gingivoplasty of the margins of the gingiva is performed if needed by means of knives or rotary diamond burs
- Periodontal dressing can be placed over the incised area during the initial period of healing (10–14 days) (Figure 9)
Internal bevel gingivectomy generally begins with a scalloped internal bevel incision placed several millimeters apical to the free gingival margin, following a scalloped contour associated with normal gingival margin. The gingival marking for the incision line can be performed by using a previously vacuum-form template representing the final gingival margins fabricated on the patient’s cast as shown in Figure 10 prior to gingivectomy to create clinical crown length for restorative and aesthetic purposes.
In the case of internal bevel gingivectomy, a mucoperiosteal flap is produced that can then be positioned and sutured to cover the alveolar bone (Figure 10, bottom left). This procedure is most frequently referred to as a partial-thickness flap procedure, rather than a true gingivectomy.
The inverse bevel distal wedge technique is usually associated with buccal and palatal inverse bevel access incisions and flap reflection for pocket reduction. Figure 11 is an example of the distal wedge (Mohawk) procedure distal of the second maxillary molar, presenting a preoperative palatal view of the enlarged tuberosity region with excessive probing depth (top left). The procedure included an initial scalloped incision apically to the gingival margin and coronal to mucogingival junction made around the first and second molars and extended into the tuberosity region in a triangular shape (top right). The palatal view shows the underlying bony defect with no distal furcation involvement. Once the distal triangular-shaped wedge was dissected from the underlying bone and removed, thick flaps were thinned and thorough debridement in the area was completed (bottom left). The buccal and palatal flaps are positioned and sutured apically using vertical mattress sutures obtaining a reduction in soft tissue height in the tuberosity region in addition to the palatal and buccal areas of the first and second molars (bottom right). Often this procedure is combined with osteotomy/ostectomy procedures, detailed in Chapter 3, Case 3.
Electrosurgery (reviewed in [11]) and chemical gingivectomy are currently outdated procedures due to delayed healing [7] and poor accuracy in reshaping of gingival tissue, as well as damage to the healthy adjacent hard and soft tissues.
Laser-assisted surgery has been introduced for the treatment of soft tissue, including removal and recontouring of gingiva in case of persistent gingival enlargement of various etiologies. Various types of lasers such as the ND:YAG laser and the CO2 laser have been used for a variety of intraoral soft tissue procedures, and the overall benefits of laser treatment include reduced bleeding during surgery with consequent reduced operating time and rapid postoperative hemostasis, no need for sutures, and improved postoperative comfort and healing [6,11].
C. The critical period for a complete healing of a gingivectomy wound is between 2 and 5 weeks after the surgery; therefore meticulous oral hygiene is essential for the establishment of a physiologic gingival sulcus [12].
D. The sequence of wound healing process after gingivectomy has been studied by various methods, in both animal models as well as humans. The initial study by Engler et al [12] looking at the epithelialization post-gingivectomy in rhesus monkeys using tritiated thymidine radiography found that migrating epithelial cells start to cover the wound between 12 and 24 hours after surgical excision. Complete healing of the sulcus aspect of the gingivectomy takes 4 to 5 weeks, although the surface appears to be healed after 2 weeks.
Moreover, the same group [13] published a follow-up paper describing the connective tissue aspect of healing and regeneration following simple gingivectomy in three monkeys with histologic and radioautographic techniques. Their results show that connective tissue proliferation is initiated 1–2 days after the surgery and reaches a peak 3–4 days after the surgery. However, functional arrangement and collagenous maturation of the gingival connective tissue fibers as well as the establishment of a physiologic restoration of a gingival crevice, with a sealing normal epithelial attachment that depends on a firm gingival tone, both require 3–5 weeks following gingivectomy.
Similarly, Listgarten [14], using an electron microscopic examination of the dento-gingival junction after gingivectomy in monkeys, found that epithelial reattachment against morphologically normal and superficially altered cementum may occur in ≤12 days after surgical excision.
Another study [15] investigating the clinical and histologic gingival healing in humans following gingivectomy reported that complete surface epithelization of the gingivectomy wound appears within 7–14 days after surgery; still active connective tissue repair was seen 28 days after gingivectomy, the last time point examined after the surgery.
Case 2
Preprosthetic Hard Tissue and Soft Tissue Crown Lengthening
CASE STORY
The patient was a 29-year-old male who had been referred to the Department of Periodontology for an evaluation of the anterior mandibular sextant based on a history of trauma. He had been accidentally hit in the anterior mandible with a racket while playing squash; #24 was extracted subsequently to the accident. His chief complaint was to save and restore as many teeth as possible. Figures 1–4 illustrate the clinical situation at the first periodontal examination.
Figure 1: Preoperative condition with the temporary fixed partial denture, facial view.

Figure 2: Preoperative condition with the temporary fixed partial denture, occlusal view.

Figure 3: Preoperative condition without the temporary fixed partial denture, facial view.

Figure 4: Preoperative condition without the temporary fixed partial denture, occlusal view.

LEARNING GOALS AND OBJECTIVES
- To identify the indications for crown lengthening
- To understand the prosthetic needs and periodontal requirements to restore altered teeth
- To understand key considerations at the time of surgery
Medical History
The patient was healthy and received a medical examination every year. He did not take medications and did not report any allergies or any medical problems.
Review of Systems
- Vital signs
- Blood pressure: 123/68 mm Hg
- Pulse rate: 62 beats/minute (regular)
Social History
The patient drank alcohol occasionally. He did not smoke and did not use recreational drugs.
Extraoral Examination
No significant findings were found (Figure 5). The patient had no masses or swelling and the temporomandibular joints were within normal limits.
Figure 5: Periodontal charting.
Intraoral Examination
- The soft tissues of the mouth appeared normal. The oral cancer screen was negative.
- The gingival examination revealed a thick and flat periodontium with generalized mild marginal erythema, rolled margins, and blunted papillae in the mandibular anterior sextant (Figures 1 and 3).
- A hard tissue examination was completed. There was a small amount of sound tooth structure available for the prosthetic restoration of teeth #22, 23, 25, 26, and 27 (Figures 3 and 4).
- The edentulous ridge (site #24) had deformities in the buccolingual and apico/coronal directions (Seibert class 3).
Occlusion
Findings included canine and molar angle class 1, group function on lateral excursion, and incisal guidance in protrusion.
Radiographic Examination
Incomplete root canal treatments on teeth #22, 23, 25, 26, and 27 and periapical radiolucencies on #25 & 26 were observed on the periapical radiographs. There was no horizontal bone loss, the lamina dura was visible and continuous, and bone trabeculations appeared normal (Figure 6).
Figure 6: Periapical radiographs of the mandibular anterior sextant. Incomplete root canal treatments and periapical radiolucencies on #25 and 26 are visible.
Treatment Plan
Periodontal, prosthodontic, and endodontic evaluations were performed to assess the restorability of the teeth. The multidisciplinary team deemed the teeth restorable with an endodontic retreatment for teeth #22, 23, 25, 26, and 27, crown lengthening, cast post and core, PFM crowns #22, 27, and a fixed partial denture (FPD) #23-X-25-26.
Treatment
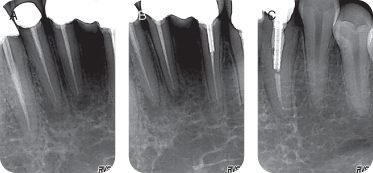
The patient received oral hygiene instructions and a prophylaxis. The endodontic retreatments were performed (Figure 7), and a temporary FPD #22-23-X-25-26-27 was fabricated (Figure 8).
Figure 8: Preoperative facial view.

Preoperative Consultation
The medical history was reviewed. A clinical and radiographic examination was performed. The amount of sound tooth structure present in the mandibular anterior sextant supragingivally was inadequate, and there was a lack of ferrule (Figure 3); the restorative margins were subgingival in some areas and were impinging on the biologic width (Figure 4). Upon radiographic examinations (Figure 6), the periodontal support for the incisors and canines was sufficient and could tolerate 3 mm of ostectomy.
The consent form addressing benefits and risks associated with the procedure was reviewed with the patient. Preoperative prescriptions were delivered to the patient: Ibuprofen 600 mg (every 4–6 hours for pain as needed) and Peridex 0.12% (bid).
Crown Lengthening Procedure
Bilateral mental nerve blocks and local infiltrations were achieved with lidocaine 2% (epinephrine 1/100,000). The temporary FPD was removed (Figures 8 and 9). A submarginal incision was performed around #22, 23, 25, 26, and 27 (Figure 10) to achieve 2–3 mm of gingivectomy (Figure 11). Buccal and lingual full-thickness flaps were elevated beyond the mucogingival junction to expose the cortical bone of the mandibular anterior sextant (Figure 12). Ostectomy was carried out to expose at least 4 mm of sound tooth structure above the crestal bone and allow for 2 mm of biologic width and at least 1.5 mm of ferrule. Osteoplasty allowed the removal of widow’s peaks, ledges, and bony irregularities (Figure 13). Odontoplasty was performed as needed when the embrasure space was too narrow (Figures 14 and 15). The buccal and lingual flaps were apically positioned and stabilized with vertical mattress sutures (Figure 16). The temporary FPD was cemented back (Figure 17). Postoperative instructions including oral hygiene instructions were delivered and an ice pack was placed against the patient’s lip.
Figure 9: Preoperative facial view after the temporary fixed partial denture is removed.

Figure 10: Submarginal incisions.
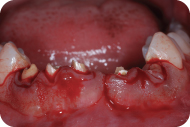
Figure 11: Gingivectomy.

Figure 12: A full-thickness flap is elevated and cortical bone is exposed.

Figure 13: Ostectomy and osteoplasty allow a greater exposure of sound tooth structure.
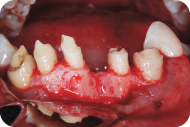
Figure 14: The embrasure between #21 and 22 is narrow.

Figure 15: Odontoplasty of the distal surface of #22 is performed to open the embrasure between #21 and 22.

Figure 16: The flaps are apically positioned and stabilized with vertical mattress sutures.

Figure 17: The temporary FPD is cemented back.

The patient was seen for a postoperative consultation 7 days and 21 days after the procedure. The prosthetic margins were refined 8 weeks after surgery, cast post and core (Figures 18 and 19) and final restorations (Figure 20) were cemented 3 weeks later.
Figure 18: Periapical radiographs after cementation of the final cast post and core.
Courtesy Dr. Pri/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



