Head and Neck Burn Injury
Epidemiology
A burn is defined as a traumatic injury to the skin or other organic tissue primarily caused by thermal or other acute exposure. Burn injury to tissues is caused by the contact with heat, flame, chemicals, electricity, or radiation. Timely and adequate management of burn injuries is paramount. Such injuries are painful and can result in mutilating and scarring, amputation or necrosis of affected tissue or, in extreme cases, death. Peripheral nervous system, vasculature, skeletal muscles, and bones could be affected at a distant site to the burn.1 Burns are one of the most distressing injuries and contribute to major global morbidity and mortality.2,3 Each year, approximately 450,000 people in the United States seek medical care for burns.4,5 The mortality rate for the hospitalized patients reaches 3.9%. An estimated 3,000 deaths result from residential fires and 500 from other sources, including motor vehicle accidents (MVAs) and aircraft crashes and contact with electricity, chemicals, or hot liquids and substances. About 75% of these deaths occur at the scene or during initial transport. Fire and burn deaths are combined because deaths from burns in fires cannot always be distinguished from deaths from smoke poisoning. Most burn injuries, approximately 66%, occur in the home setting. The 2011 National Burn Repository has reported that burns due to fire and flame predominate in the 5-year and older age group. Scalds were most frequent in children younger than 1 to 5 years. In Middle East countries, burning from oil explosion are among the most common types of the burn in oil well workers.6 Self-burning suicide also is prevalent in these countries. Patients with a total burn size of 40% burn surface or more accounted for only 4.2 % of cases. Fatality clearly increases with burn size. The burn size associated with a 50% case fatality appears to be approximately 70% total burn surface (TBSA). Complications such as pneumonia, cellulitis, and urinary tract infections are the most prevalent complications noted in burn center patients. Many burn injuries are minor and do not require hospital admission.7,8 The mean length of hospital stay was approximately 9 days in 2010.
Mechanisms of Burn Injury
Burns may be caused by several different mechanisms with associated complications:
Thermal Injury
The depth of the burn injury is related to contact temperature, duration of contact of the external heat source, and thickness of the skin. Thermal injury is generally classified as scald or flame injury.5 As the temperature rises, increasing molecular collisions occur, resulting in altered molecular conformation and the disruption of intermolecular bonds. This process leads to cell membrane dysfunction as ion channels are disrupted, resulting in sodium and water intake. As the temperature rises further, protein denaturation occurs, oxygen radicals are liberated, and eventually cells die with the formation of the burn scar.9
Scalds
These types of burns result when skin comes into contact with hot liquids. About 70% of burns in children are caused by scalds.10
Chemical Burns
These burns result from contact of the skin with chemicals or by ingestion of chemicals. Most chemicals that cause chemical burns are strong acids or bases. Contact with acid produces tissue coagulation, whereas alkaline burns generate colliquation necrosis.11
Electrical Burns
Electrical energy is transformed into thermal injury as the current passes through poorly conducting body tissues (Fig. 28-1). The amount of heat generated, and hence the level of tissue damage, is equal to 0.24 multiplied by (voltage)2 times resistance. Domestic electricity is low voltage and tends to cause small deep contact burns at the exit and entry sites. Electricity greater than 1000 V may cause muscle damage, rhabdomyolysis, and renal failure.10
Pathophysiology of Burns
Skin Anatomy
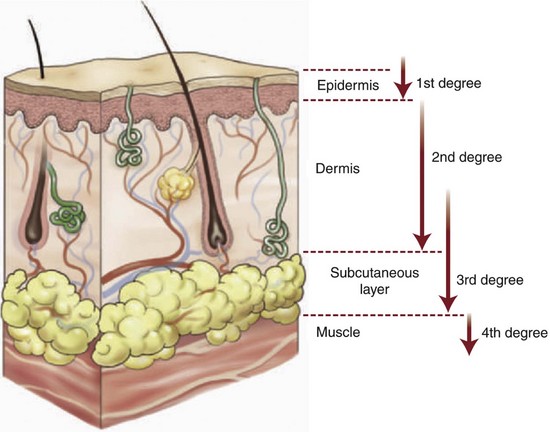
The skin is the largest organ of the body. It functions as a neurosensory organ and protects against the invasion of foreign bodies and organisms. It has specific immune and metabolic functions and is important in regulating body temperature and fluid, protein, and electrolyte homeostasis. Loss of the functional skin barrier after thermal injury remits increases the susceptibility to infection, which is the major cause of morbidity and mortality postburn.12 Skin thickness varies with age and body location, but averages only 1 to 2 mm (0.04 to 0.08 inch) thick. The skin is composed of several layers, with the two primary layers being the epidermis and underlying dermis (Fig. 28-2). The thickness of skin affects susceptibility to burning. The skin on the palms of the hands and on the soles of the feet, for example, is thick and more resistant to burning than that of the forearms or eyelids. Skin consists of three different layers of varying thickness throughout the body. The epidermis is the outermost layer of the skin with self-renewal properties and protects the skin from the exogenous environment. The average thickness of the epidermis is 0.1 mm.13 The dermis has an average thickness of 2 mm and is a fibrous network of tissue that gives resiliency to the skin. Major proteins found in the dermis are collagen and elastin produced by fibroblasts. The vasculature in the dermis helps with thermoregulation and provides nutrients for the epidermis. The superior part of the dermis is called the papillary dermis, which abuts the epidermis. It consists of loose connective tissue with a lower amount of collagen and elastic fibers. The inferior part of the dermis, the reticular dermis, with lower cell density, contains higher amounts of collagen and elastin fibers. An areolar subcutaneous tissue lies below the dermis and is the third anatomic layer of the skin.
Body Responses to Burns
Local Responses
Fairly high temperatures can be sustained by the skin because of its substantial water content. As long as the water content is not totally eliminated by the heat in thermal injury, the temperature of the skin will not exceed 82° C (179.6° F).14 Areas of increased vascularity allow heat to be transferred from the burn site because of high blood flow. This heat dissipation may decrease the depth of burn in such areas.15 Major burns have three distinct zones of injury (Jackson’s thermal wound theory), which usually appear in a bull’s-eye pattern.16
Systemic Responses
Where the area of the burn wound exceeds 20% TBSA, there is a risk that the protective inflammatory response becomes overwhelmed, with proinflammatory mediators and subsequent significant systemic manifestations. The early phase of burn edema, lasting from minutes to 1 hour, is attributed to mediators such as histamine, products of platelet activation, eicosanoids, and proteolytic products of the coagulation, fibrinolytic, and kinin cascades. Vasoactive amines may also act by increasing microvascular blood flow or vascular pressures, accentuating the burn edema.18
Cardiovascular Changes.
Capillary permeability is increased, leading to loss of intravascular proteins and fluids into the interstitial compartment. Histamine is probably responsible for the early phase of increased vascular permeability after burn injury because it is released in large quantities from mast cells in burned skin immediately after injury.19 Peripheral and splanchnic vasoconstriction occur. The cardiomyocyte shock state is a result of impaired calcium homeostasis and subsequent intracellular signaling dysregulation.20
Metabolic Changes.
The basal metabolic rate increases up to three times its original rate.17 Glucose metabolism is elevated in almost all critically ill patients, including those with burn injuries. Gluconeogenesis and glycogenolysis are increased in burn patients. In addition, plasma insulin levels typically are elevated in burn patients. The basal rate of glucose production is elevated despite this hyperinsulinemic state, which can be defined as hepatic insulin resistance.21 Exogenous insulin administration to achieve euglycemia has been shown to decrease donor site healing time and decrease length of stay while ameliorating skeletal muscle catabolism.22 Lipolysis occurs at a rate in excess of the requirements for fatty acids as an energy source due to alterations in substrate cycling. Proteolysis is increased in burn patients. Following utilization, protein is excreted primarily in the urine as urea. This results in an increased efflux of amino acids from the skeletal muscle pool, including gluconeogenic amino acids. Protein intake greater than 1 g/kg/day has been recommended for all thermally injured patients and, for burn patients with normal renal function, the recommended protein intake is 2 g/kg/day.
Severity Index
Assessing the severity of a burn injury requires accurate clinical staging, which permits appropriate therapy to be initiated in the proper medical facility. It is important to determine the source and circumstances of the injury, probable depth of cutaneous destruction, and extent of the body surface involved.14
Classifications of Burn Depth
A precise classification of burn injury may be difficult. The depth of a burn can be assessed clinically by its appearance. Punch biopsy of burned tissue with subsequent histologic assessment has been regarded by some as the criterion standard of depth diagnosis, serving as the basis for comparison of other diagnostic modalities.23 Burn lesions are originally classified based on the clinical signs and symptoms, from first- to fourth-degree burns. The American Burn Association in 2009 released a newer classification based on anatomic depth involvement of the skin:
• Superficial or epidermal (first-degree burn; Fig. 28-3)
Burns extending beneath the subcutaneous tissues and involving fascia, muscle, and/or bone are considered fourth-degree burns (see Fig. 28-2 and Table 28-1).5,11,24
TABLE 28-1
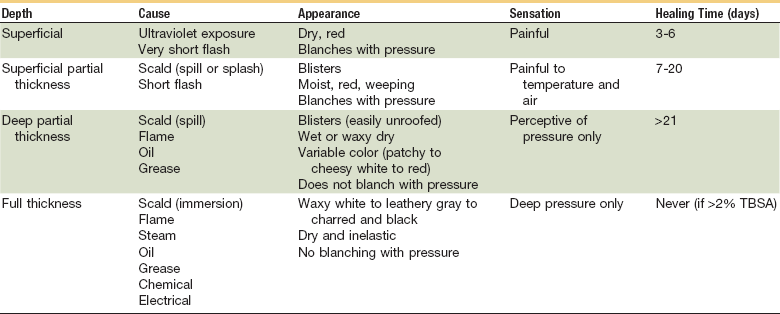
Mertens DM, Jenkins ME, Warden GD: Med Clin North Am 1997: 32:343, Peate WF, Am Fam Physician, 1992:45:1321; Clayton MC, Solem LD: Postgrad Med 1995:97:151.
Superficial Burn (First-Degree)
These burns affect the outer layer of skin, causing pain, redness and swelling (see Fig. 28-3). Superficial burns equal to first-degree burns involve minimal tissue damage and involve the epidermis (skin surface). Sunburn is a good example of this type of burn.
Partial-Thickness Burns (Second-Degree)
Partial-thickness burns involve the epidermis and portions of the dermis and can be clinically categorized as superficial partial-thickness or deep partial-thickness burns (see Fig. 28-4). Superficial partial-thickness burns characteristically form blisters between the epidermis and dermis. Because blistering may not occur for some hours after injury, burns that initially appear to be only epidermal in depth (first degree) may be determined to be partial-thickness burns 12 to 24 hours later. Most superficial partial-thickness burns heal spontaneously in less than 3 weeks, and do so typically without functional impairment or hypertrophic scarring. Deep partial-thickness burns extend into the lower layers of the dermis. They possess characteristics that are distinctly different from superficial or mid-dermal partial-thickness burns. If infection is prevented and spontaneous healing is allowed to progress, these burns will heal in 3 to 9 weeks. However, they invariably cause considerable scar formation. These burns are best treated by excision and grafting. For the patient, a partial-thickness burn that fails to heal within 3 weeks is functionally and cosmetically equivalent to a full-thickness injury.
Full-Thickness Burns (Third-Degree)
Full-thickness burns extend down into the hypodermis or subcutaneous tissue (see Fig. 28-5). These burns in themselves are generally not painful; however, there may be surrounding areas of partial-thickness burns that are painful. Skin appearance can vary from waxy white to leathery gray to charred and black. The skin is dry and inelastic and does not blanch with pressure. Hairs can easily be pulled from hair follicles. Vesicles and blisters do not develop.
Fourth-Degree Burns
Fourth-degree burns are deep and potentially life-threatening injuries that extend through the skin into underlying tissues such as fascia, muscle, and/or bone.11 However, the clinical methods outlined may not provide sufficient accuracy of evaluation of burn depth to support crucial treatment decisions, such as the extent of excision and grafting required. Laser Doppler imaging (LDI) has been shown to provide a more objective measurement on which to base the decision to operate.25
Burn Assessment
To determine the need for referral to a specialized burn unit, an assessment tool is needed to aid in the decision making process.5,11 Under this system, burns can be classified as major, moderate, and minor. This is assessed based on a number of factors, including TBSA burnt, involvement of specific anatomic zones, age, and associated injuries (Table 28-2).
TABLE 28-2
American Burn Association: Burn Injury Severity Grading System
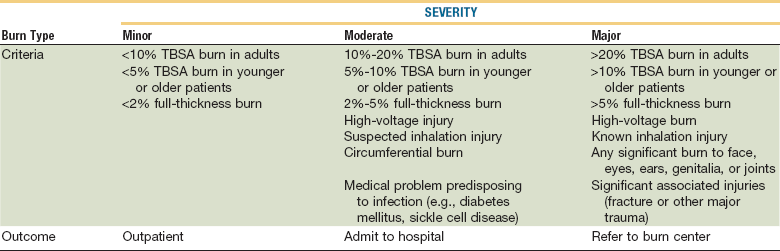
Reproduced with permission from Hartford CE, Kealy CP: Care of outpatient burns. In Herndon DN (ed): Total Burn Care, ed 3, Philadelphia, 2007, Elsevier.
Burn Size
The Rule of Nines.
To approximate the percentage of burned surface area, the body has been divided into eleven sections: head, right arm, left arm, chest, abdomen, upper back, lower back, right thigh, left thigh, right leg (below the knee), left leg (below the knee). Each of these sections takes about 9% of the body’s skin to cover it. Added all together, these sections account for 99%. The genitals make up the last 1% (Fig. 28-6). This rule is relatively accurate in adults, but inaccurate in children. In children, the Lund-Browder chart is the recommended method because it takes into account the relative percentage of body surface area affected by growth (Table 28-3).11 In small burn injuries, the extent of injury can be quickly estimated because the palm of a patient’s hand represents approximately 1% of the TBSA.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses