Quality of the endodontic treatment
Quality of the coronal restoration
% success (absence of peri-radicular inflammation (API))
Good
Good
91.4
Good
Poor
44.1
Poor
Good
67.7
Poor
Poor
18.1
A retrospective study carried out over 3 years on 55 patients who had adequately root-filled teeth that had inadequate coronal restorations due to decay or that had been lost were investigated. At the end of the observation period 78 % of the teeth showed identical periapical conditions compared to the preoperative status showing no signs of apical periodontitis [15]. A further histological examination using Brown and Brenn staining of longitudinal sections of 39 root specimens in 32 extracted teeth was used to determine the role of coronal bacterial leakage and periapical health outcomes. All teeth had been lacking coronal restorations for a minimum of 3 months and in some specimens for several years. They concluded that despite prolonged exposure to the oral environment, bacterial penetration only seemed to occur in the coronal portion of roots in the majority of cases. It thus appears that well prepared and optimally sealed root canals resist bacterial penetration even after long exposures to the oral environment [16] (Fig. 2.1).
Fig. 2.1
Preoperative radiographs demonstrating root canal treatments of teeth 11 and 21. (a) Tooth 21 has a technically deficient root canal filling with a void in the apical 1/3rd. The coronal restoration is nevertheless deemed good with no marginal discrepancies noted. An intact periodontal ligament space is observed. Tooth 11 has a well obturated root canal with an obvious peri-radicular radiolucent lesion (dotted green line). (b) A horizontal tube shift radiograph confirms marginal discrepancies (red arrows) which may account for bacterial ingress and recontamination of the root canal space
Numerous in vitro studies, using radioisotopes, dyes and microbes, have shown that exposure of coronal gutta-percha to bacterial contamination can lead to migration of bacteria and bacterial by-products to the apex in a matter of days. In 1990 Torabinjead and colleagues studied the penetration of Staphylococcus epidermidis and Proteus vulgaris on 45 single-rooted extracted teeth sealed by lateral condensation and Roth’s sealer, but without coronal restorations. In 19 days, 50 % of teeth were contaminated to their full length after exposure to S. epidermidis. In 52 days, 50 % of teeth were contaminated to full length after exposure to P. vulgaris. Magura and colleagues evaluated the effect of salivary percolation in 150 single-rooted extracted teeth over a time period of 3 months. The teeth were sealed by lateral condensation and Roth’s sealer prior to salivary exposure. Teeth were evaluated by means of dye and histology. They concluded that retreatment should be considered in any case that has been exposed to the oral environment for over a 3-month period prior to placement of a definitive coronal restoration. In 1993 Khayat and colleagues showed that when the coronal 3 mm of root filling was removed and sealed with sticky wax, no leakage of bacteria occurred, whereas all root fillings sealed by lateral condensation and Roth’s cement without a coronal orifice barrier were penetrated within 30 days. Although both in vitro and in vivo studies have questioned this correlation, taken together it seems essential to prevent coronal leakage secondary to restorative failures, both during endodontic treatment and following completion. Both temporary/interim and final definitive restorations must be placed, keeping in mind not only the capability of withstanding the physical, chemical and thermal stresses within this harsh oral environment but also to provide a further barrier against the rich resident microflora that exists [17–21].
Prior to commencing endodontic therapy, it is essential to minimize potential bacterial ingress into the tooth via caries, cracks, exposed dentine and broken-down restoration margins. Complete removal of caries and defective restorations, establishment of sound supragingival tooth margins (required for optimal rubber dam placement) and restorability assessment are mandatory for all cases. Potential cracks and fracture lines should be identified using dyes or fibre optics to ensure that long-term success is both predictable and achievable. If the existing restoration, crown or onlay appears to be clinically and radiographically satisfactory and replacement is not planned, then the internal chamber and restorative material should be carefully inspected using magnification to ensure that neither caries or marginal gaps exist [22–27].
Many different temporary materials and techniques have been proposed for the restoration of teeth during endodontic therapy (see Table 2.2). Commonly used materials within endodontics include gutta-percha, glass ionomer cements (GIC), resin-modified GIC, composite resin, amalgam, reinforced interim restorative material in a zinc oxide eugenol base (IRM, Dentsply Caulk, Milford, USA) and calcium sulphate-based filling material (Cavit, 3 M ESPE, Seefeld, Germany). Cavit and IRM have withstood the rigours of testing and evaluation and can be used in combination to produce a “double seal”. Alternatively GIC can be used in conjunction with Cavit as the external material of this desirable “double seal” [28–37].
Table 2.2
Various materials used for temporization in endodontics
|
Situation
|
Materials
|
|---|---|
|
Temporization of access cavity
|
Gutta-percha, zinc phosphate cement, polycarboxylate cement, zinc oxide/calcium sulphate, zinc oxide eugenol, GIC, composite resin
|
|
Broken-down teeth
|
Copper bands, orthodontic bands, temporary crown, pin-retained amalgam, GIC, composite resin
|
|
Nonvital walking bleach
|
IRM, polycarboxylate, zinc phosphate, GIC, Cavit
|
|
Long-term temporization
|
GIC, composite resin, amalgam cuspal coverage restorations
|
Prior to temporary filling placement during multi-visit endodontic treatment, an intra-canal inter-appointment medicament such as calcium hydroxide can be placed in the root canal to act as a barrier to the ingress of microorganisms. A dry cotton wool pledget can be placed to occlude the canal orifices preventing temporary filling material from displacing into the canals. The cotton wool can also act as a guide when reaccessing the tooth preventing iatrogenic errors such as inadvertent over-drilling and possible perforation, thus simplifying access for subsequent endodontic or restorative procedures. The cotton wool should also be thin enough to allow for sufficient space between the cotton wool and cavosurface margin of the access preparation permitting placement of an adequate thickness of temporary filling material. Some authors do not believe there is an indication for cotton wool pledget use with an increased inadvertent risk of fibres adhering to cavity walls and serving as a wick [28, 38, 39] (Fig. 2.2).
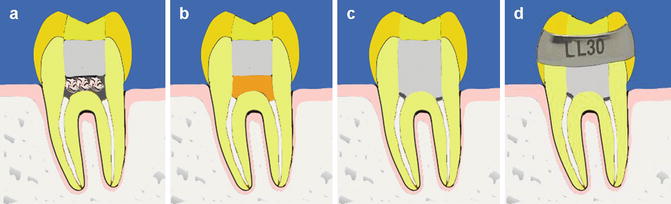
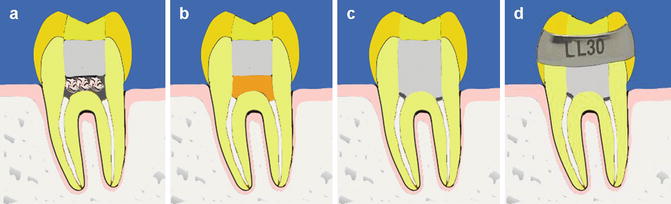
Fig. 2.2
Diagrammatic representation of various methods of interim restorations. Note (a) cotton wool pledgets placed over the canal orifices (dressed with medicament) to prevent dislodgment of overlying temporary restorations into the canals. The cotton wool must not have fibers adhering to the adjacent walls and externally that can result in a salivary wicking effect and recontamination. (b) Gutta-percha material placed over medicated canals to prevent material extrusion, (c) no temporary barrier used below the “double seal” restoration of IRM and glass ionomer cement, and (d) example of an orthodontic molar band with equal mesial and distal heights supragingi
Stainless steel orthodontic bands have been recommended for the use of endodontically treated posterior premolar and molar teeth in conjunction with the placement of interim restorations. The main purpose of using bands is to protect the tooth from cuspal fracture (particularly in cracked teeth) and aid in strengthening and retaining the interim restoration during the endodontic phase of treatment [29, 40].
The copper band provisional restoration is an ideal choice for ensuring adequate sealing and isolation of badly broken-down teeth. Its use can often transform a complex endodontic access preparation with minimal retentive walls into a class I cavity with adequate retention and strength for the interim temporary core [41, 42].
Following dismantling of a cuspal coverage cast restoration, the use of a well-fitting provisional restoration is desirable to prevent both tooth movement and coronal microleakage during endodontic procedures. A multitude of materials are available including direct chairside materials such as preformed crowns (made of plastic or metal), self-cured or light-cured resins or resin composites and cements. Laboratory-formed temporaries are generally made in self-cured or heat-cured acrylic or cast metal. Common self-cured or light-cured resins used either directly or indirectly include polymethyl methacrylate (e.g. Snap, Trim), bis-acryl composite (e.g. Protemp) and restorative composite. Bis-acryl composites produce less heat and shrinkage during polymerization than other resins, resulting in better marginal fit. Proprietary temporary cement materials are used to retain the provisional restoration in place and allow for easy removal if required (e.g. Tempbond) [43, 44].
When a custom-made post and core restoration is planned, a temporary post crown restoration may be required. Due to the inadvertent risk of further bacterial contamination of the root canal space, the temporary post and core restoration should be left in place for as short a time as possible. The use of prefabricated post and core systems immediately after completion of endodontic treatment has the advantage of minimizing microleakage and recontamination. An alternative method to reduce the possibility of coronal seal disturbance would be the use of a full coverage vacuum-formed retainer to replace the missing coronal tooth structure. These types of removable prosthodontics options have been used for temporization in the aesthetic zone after implant fixture placement [45–47].
Temporization for internal bleaching (walk-in bleach technique) requires the use of both a protective barrier overlying the orthograde gutta-percha material and suitable temporary restorative materials to be placed over the bleaching agent in between bleaching appointments. Polycarboxylate, zinc phosphate, glass ionomer, IRM or Cavit of at least 2 mm thickness are recommended for the purpose of barrier protection. Cavit and Coltosol with sufficient bulk can be used as interim restorations during the bleaching procedures (see Chap. 18).
After completion of endodontic treatment gutta-percha can be cut back to within the canal orifices, and an intra-orifice barrier can be placed to protect it. The uses of intra-orifice barriers, which are restorative materials placed over the canal orifices and covering the pulp chamber floor, have been advocated to provide a secondary seal. Criteria have been proposed for the ideal intra-orifice barrier. They should: (a) be easily placed and bond to tooth structure (retentiveness), (b) seal effectively against coronal microleakage, (c) be easily distinguished from the natural tooth colour and (d) not interfere with the final restoration of the access preparation. This material can be any material that will bond or seal the dentine and have a distinguishable colour from dentine. Common orifice barriers include Tetric Chroma (Vivadent), Permaflow Purple (Ultradent), Flow-it clear (Pentron) or resin-modified glass ionomer material [48, 49].
No current restorative material can claim to prevent microleakage completely. Interim temporary restorations serve to reduce contamination of the root canal system until permanent restorations have been placed. Due consideration when selecting a temporary material should be given based on the amount of remaining tooth structure, occlusal forces likely to be placed and length of intended time prior to three-dimensional obturation and permanent restoration procedures. Adequate thickness of material and accurate placement are crucial in minimizing recontamination. Clinicians should consider all factors and ensure that optimal temporary/interim restorations are placed to ensure optimal clinical outcomes.
2.2 Specific Materials for Temporization
Cavit
Cavit is a premixed temporary filling material that contains zinc oxide, calcium sulphate, zinc sulphate, glycol acetate, polyvinyl acetate resins, polyvinyl chloride acetate, triethanolamine and pigments. It is a hygroscopic material, and its ability to attract and hold water molecules results in a high coefficient of linear expansion with excellent marginal sealing ability. At least 3–4 mm of thickness is required to ensure optimal sealing ability. The material is ideal when used in conjunction with glass ionomer cement as a “double seal” restoration during root canal treatment and following completion prior to permanent restoration.
Coltosol
Coltosol is a zinc oxide, zinc sulphate and calcium sulphate hemihydrate-based material that hardens within 20–30 min when in contact with moisture. According to the manufacturer, the temporary filling can be subjected to masticatory forces within 2–3 h of placement. This material is recommended for short-term temporization not exceeding 2 weeks.
Zinc oxide eugenol
Zinc oxide eugenol is a widely used temporary restorative material consisting of powder (zinc oxide, pulverized glass or silica) and liquid (zinc chloride and borax). Reinforced zinc oxide eugenol preparations (Kalzinol) using a polystyrene polymer results in doubling of the compressive strength important in areas subjected to mechanical loading. Reinforced zinc oxide eugenol preparations (IRM) using polymethyl methacrylate provide improved compressive strength and hardness. During inter-appointment temporization, the use of a low powder to liquid ratio of zinc oxide eugenol preparations including IRM can provide adequate resistance to microbial penetration. A double seal technique using glass ionomer cement to overlay an adequate thickness of IRM will be effective in maintaining a good marginal seal.
Glass ionomer cement
Conventional glass ionomer cements contain a fluoroaluminosilicate ion leachable glass and a water-soluble polymer acid, which reacts to form cement. Current materials may contain a poly(alkenoic acid), which contains a copolymer of acrylic acid with itaconic or maleic acid. The polymer is often supplied as a dry powder blended with the glass. The powder is either hand mixed with water or supplied as capsules for mechanical mixing. Tartaric acid is often added to provide a clinically acceptable setting time. On mixing an acid-base reaction between the aqueous poly(alkenoic acid) and glass occurs. The outer layers of the glass particles decompose, releasing calcium and aluminium ions. These ions migrate into the aqueous phase forming cross-linked polyalkenoate chains, resulting in gelation and setting of the material. The set cement consists of a core of unreacted glass particles surrounded by a salt-like hydrogel bound by the matrix of reaction products. Glass ionomer cements can chemically bond to tooth structure, further reducing any marginal discrepancies between restorative and tooth interface. In endodontics they are ideal temporary restorations but need to be replaced over the long term due to low tensile strengths making them unsuitable in load-bearing areas of the mouth.
Composite resin restorations
Composite restorations consist of four main components, namely, the resin (organic polymer matrix), filler particles (inorganic), coupling agent (silane) and the initiator-accelerator of polymerization. The most common resin monomers used in composite restorations is BisGMA. To accommodate better filler load, triethylene glycol dimethacrylate (TEGDMA) or urethane dimethacrylate (UDMA) is added. Filler particles provide dimensional stability for the soft resin matrix and vary in size. Common filler particles include crystalline quartz, silica and glasses such as barium and strontium silicate. The size of the filler particles incorporated in the resin matrix has evolved over the years. Filler particles determine the mechanical properties of the composite material including wear, translucency, opalescence, radiopacity, surface roughness and polishability. Filler particle sizes can be classified into microhybrid, microfill or nanofiller. Microhybrid filler particles consist of glass or quartz particles ranging in sizes of 0.2–3 and 0.04 μm microfine particles. Microfill particles sizes range from 0.02 to 0.04 μm and nanohybrids are 0.01–0.04 μm. The coupling agent silane helps form a bond between the resin matrix and filler particles during the polymerization setting reaction. Initiators and accelerators are added for either chemical (aromatic tertiary amines) or photo-activated light curing (camphorquinones).
Enamel consists of 96 % inorganic hydroxyapatite prisms, 1 % organic material and 3 % water. In 1971 Buonocore showed that it was possible to bond resin to enamel after etching with 20–50 % phosphoric acid. Dentine consists of approximately 70 % inorganic hydroxyapatite, 20 % organic material (mainly collagen) and 10 % water. Dentine also consists of dentinal tubules that contain water making the hydrophobic resin difficult to penetrate. In addition the cut surface of dentine is covered by a smear layer composed of deranged dentine and bacteria, further reducing the potential adherency of resin to the underlying dentine. In 1982 Nakabayashi treated the dentine surface with an acidic primer, resulting in a demineralized dentine surface of approximately 10 μ prior to application of the bonding resin 4-META (4-methacryloyloxyethyl trimellitate). This resulted in micromechanical interlocking of the resin by collagen mesh, termed the hybrid layer.
Numerous bonding systems have evolved, broadly classified into either resin-based systems with an etch and rinse approach or self-etch adhesive systems. The fourth-generation bonding systems (Scotchbond 1, 3 M, ESPE, St Paul, MN, USA, or Optibond, Kerr, Orange, CA, USA) allowed for the removal of the smear layer using 30–40 % phosphoric acid involving several steps of etching, washing with water, drying, application of a primer or adhesion-promoting agent and finally applying a dentine-bonding agent. The fifth-generation dentine-bonding agents aimed at reducing/simplifying the number of steps by combining the primer and bonding agent in one bottle. The sixth-generation self-etch adhesive systems were introduced that differ from the previous etch and rinse systems by the use of an acidified resin which is not washed off like the previous phosphoric acid in the etch and rinse systems. Two types of dentine-bonding agent systems are available. A two-step application of self-etching primer followed by bonding agent application (Prime&Bond NT, Dentsply, Wybridge, UK) and one-step application where the etching and bonding components are mixed, prior to their application as one solution (One-up Bond F, Tokuyama, Tokyo, Japan). The sixth-generation one- and two-step adhesives dissolve the smear layer, and their components become incorporated into the hybrid layer in contrast to previous generations where the smear layer was removed by washing following application of phosphoric acid.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


