Fig. 8.1
Clinical management of reversible and irreversible pulpitis in the mixed/permanent dentition. Note if the apex is open, then root-end closure procedures or pulpal regeneration may be indicated to allow for continued root development
Indirect pulp capping is a treatment modality that has gained increased popularity recently that can be undertaken in a single-visit appointment (indirect pulp capping) or a two-stage procedure (stepwise excavation) [3, 16, 17]. The premise of either treatment is to prevent exposure of the pulp during deep carious excavation by leaving the deepest carious dentine overlying the pulp in place to preserve vitality. Residual dentine thickness is an important prognostic factor for reactionary dentinogenesis and the ability of surviving odontoblasts to secrete tertiary dentine allowing continued pulp survival.
A suitable lining material is placed to allow for reparative dentine stimulation [18]. There is no general agreement as to what type of lining material is ideal although calcium hydroxide, mineral trioxide aggregate (MTA), composite resins and glass ionomer cements have all appeared to be satisfactory in their ability to induce a calcific barrier formation [19]. The placement of a high-quality temporary and final restoration is essential for success.
In the stepwise approach for caries excavation, various amounts of carious dentine are sealed off by a temporary restoration for a period of time. Re-entry is carried out in anticipation of the possibility of remineralisation of softened noninfected dentine over the pulp and hard tissue repair. The intent is to carry out further excavation of remaining caries without ensuing pulpal exposure [20, 21].
A potential disadvantage of carrying out these types of procedures is delaying the inevitable pulpectomy and possible difficulties thereof due to ensuing pulpal reactions and calcifications that can lead to negotiation difficulties. Unfortunately, treatments are guided to either invasive pulp therapy or procedures aimed at maintaining pulpal integrity based on the probable pulpal status, which can only be verified following careful follow-up. The advantage in an immature tooth with continued root development is obvious, but in a mature tooth, the obvious benefits must be weighed up against the possibility of developing a peri-radicular apical lesion, which reduces the success rate of root canal treatment [22].
Direct pulp-capping procedures are required when an inadvertent pulp exposure has occurred. The decision to avoid a pulpectomy is based on the assumption that the radicular pulp remains vital and only superficial inflammation is present confined to a few millimetres at the site of exposure. Controversy has plagued this treatment modality, and its success depends on various issues including the size of pulpal exposure, presence of infected dentinal chips, control of haemorrhage, type of pulp-capping material used and the quality of the ‘dentinal bridge’ formed [23]. The technique is not normally advocated for carious primary molars [24].
A pulpotomy procedure should be performed on a tooth that is judged vital. The coronal pulp is amputated, and then the radicular pulp is either fixed using formocresol, preserved using a haemostatic agent such as ferric sulphate or sodium hypochlorite solution to form a clot barrier or bridged by using calcium hydroxide or mineral trioxide aggregate [30–32]. The success of the technique is highly dependent on achieving a good coronal seal, which will effectively cut off the nutritional supply for any remaining dentinal bacteria and will prevent further bacterial micro-leakage. It has been strongly recommended that adhesive restorations or preformed crowns be employed following any primary molar pulp therapy procedure [25–28].
There has been a suggestion that the use of formocresol in paediatric dentistry is unwarranted due to safety concerns. Studies have linked formocresol with nasopharyngeal cancer in both human and animal studies based on exposure to formaldehyde at very high doses. The evidence in the literature suggests that formocresol is probably not a potent human carcinogen under low-exposure conditions. Nevertheless, the fixation of radicular pulp stumps using formocresol is no longer recommended, and alternatives using either ferric sulphate or mineral trioxide aggregate have been advocated using clinical studies to demonstrate equal if not better results [27–30].
Ferric sulphate (5–15 %) promotes pulpal haemostasis by forming a protective metal-protein clot at the surface of the vital radicular pulp stumps. A zinc oxide eugenol base is then usually applied over the radicular pulpal tissue.
MTA has been used successfully in adult endodontic procedures since 1993 and has been recommended for pulp capping, pulpotomy, apical barrier formation in teeth with open apexes, repair of root perforations and root canal filling. The constituents include tricalcium silicate, dicalcium silicate, tricalcium aluminate, tetracalcium aluminoferrite, calcium sulphate and bismuth oxide. The material has excellent bioactive properties and essentially stimulates cytokine release from pulpal fibroblasts, which in turn stimulates hard tissue formation. In pulp-capping or pulpotomy procedures, it is mixed with sterile water to a sandy consistency, which is gently packed against the radicular pulp stumps. The material is hydrophilic and takes up to 4 h to set completely [32].
Desensitising pulp therapies have been recommended primarily for deciduous teeth and also used by some clinicians for the permanent dentition [33]. This two-stage technique uses paraformaldehyde paste to fix and devitalise hypersensitive coronal pulp tissue. In view of increasing concerns about the use of formaldehyde (as previously mentioned), an alternative approach, using Ledermix paste, has been recommended [34]. Ledermix is a readily available paste containing triamcinolone acetonide (steroid) and demeclocycline (antimicrobial). It is used widely in adult endodontic procedures and has been shown to reduce pulpal inflammation and pain.
Pulpectomy is indicated where the radicular pulp is nonvital or irreversibly inflamed. It is contraindicated when there is evidence of extensive internal or external root resorption or if more than one-third of the root length has been lost. The most commonly used medicaments for primary molar root canal therapy are zinc oxide eugenol (ZnOE) paste, iodoform paste and calcium hydroxide [35, 36]. Slow-setting pure zinc oxide eugenol paste has traditionally been the material of choice as a primary molar root filling material. However, concerns have been expressed regarding the slow removal of zinc oxide eugenol by the body (if extruded through the root apex) and the differential rate of resorption between this material and the tooth itself. The use of Vitapex (a mixture of calcium hydroxide and iodoform paste) has a superior success rate to that of zinc oxide eugenol and is removed more readily if extruded through an apex [37].
A recent systematic review of the literature summarised that because of the lack of good studies, it is not possible to determine whether an injured pulp as a result of deep caries can be maintained or whether it should be removed and replaced with a root canal filling. Both randomised studies and prospective observational studies are needed to investigate whether a pulp exposed to deep caries is best treated by measures intended to preserve it or by pulpectomy and root filling [38]. Current practice is dictated by best clinical judgement as to the pulpal diagnosis and appropriate treatment thereafter. Indirect pulp-capping, pulpotomy and pulpectomy procedures are indicated in deciduous teeth in order to remain as space maintainers avoiding crowding if the tooth was lost early. Immature teeth with incomplete root formation would be teeth that gain most benefit from pulp preservation procedures rather than less conservative pulpectomy treatments. Root canal procedures are reserved for those cases where apical periodontitis has been confirmed and extraction is to be avoided.
8.2 Indirect Pulp Capping
The procedure is acceptable for the management of a deep carious lesion where the patient has no signs or symptoms indicative of pulpal pathosis. The aim is to remove the entire carious lesion except for the last remaining stained dentine overlying the pulp. The rationale is to arrest the carious process and to provide conditions conducive to the formation of reactionary dentine. The remaining carious dentine (stained) is allowed to remineralise, promoting pulpal healing and preserving the vitality of the pulp without inadvertent frank carious exposure.
The procedure consists of the following steps:
- 1.
Preoperative radiograph such as a parallel bitewing and parallel periapical confirming carious lesion and proximity to pulp.
- 2.
Standard local anaesthetic protocol to provide adequate anaesthesia.
- 3.
The use of rubber dam to isolate the tooth being treated.
- 4.
All caries is removed at the enamel-dentine junction (periphery of the cavity).
- 5.
Careful removal of soft deep carious dentine (using slow-speed hand-piece with a round stainless-steel bur and excavators) overlying the pulp region with care avoiding a pulpal exposure.
- 6.
Placement of appropriate lining material such as hard-setting calcium hydroxide cement, reinforced glass ionomer cement or zinc oxide eugenol.
- 7.
Placement of a definitive restoration. An excellent coronal seal needs to be provided to prevent further micro-leakage (Fig. 8.2).
 Fig. 8.2Diagrammatic representation of the indirect pulp capping procedure. (a) Preoperative view demonstrating deep caries (DC) overlying pulp (P) and (b) post-operative following caries removal. Note stained dentine overlying pulp (S) is left in situ. A suitable lining material [L] and an excellent coronal seal (CS) are placed
Fig. 8.2Diagrammatic representation of the indirect pulp capping procedure. (a) Preoperative view demonstrating deep caries (DC) overlying pulp (P) and (b) post-operative following caries removal. Note stained dentine overlying pulp (S) is left in situ. A suitable lining material [L] and an excellent coronal seal (CS) are placed
8.3 Modified Stepwise Excavation
The stepwise excavation technique has been used for the management of deep carious lesions to avoid inadvertent pulpal exposure. A less invasive approach, whereby the deepest caries is left in situ at the first appointment, has been modified at an attempt to change an active carious lesion into an arrested lesion. The aim of the first excavation is to change the carious environment without removing the softened carious dentine, which is in close proximity to the pulp. If one were to try and remove all the caries close to the dentine-pulpal border, then a pulpal exposure may be created. The active soft yellowish dentine will eventually become darker, harder and drier demineralised dentine resembling a slowly progressing lesion. The tooth is re-entered at a later stage to complete the caries removal process.
The stepwise excavation technique consists of the following steps:
- 1.
Preoperative radiograph such as a parallel bitewing and parallel periapical confirming carious lesion and proximity to pulp.
- 2.
Standard local anaesthetic protocol to provide adequate anaesthesia.
- 3.
The use of rubber dam to isolate the tooth being treated.
- 4.
All caries is removed at the enamel-dentine junction (periphery of the cavity).
- 5.
Careful removal of the central outermost softened carious dentine using an excavator only to ensure that a provisional restoration can be placed.
- 6.
No attempt is made to excavate as close to the pulp as possible in order to remove all infected dentine, thereby reducing the risk of pulpal exposure.
- 7.
A provisional restoration is selected on the basis of the interim dressing period from 6 to 8 months.
- 8.
A second final excavation is carried out whereby careful removal of deep carious dentine (using slow-speed hand-piece with a round stainless-steel bur and excavators) overlying the pulp region with care avoiding a pulpal exposure. As per the indirect pulp-capping treatment, any hard stained dentine overlying the pulp can be left in situ to avoid exposure.
- 9.
Placement of appropriate lining material such as hard-setting calcium hydroxide cement, reinforced glass ionomer cement or zinc oxide eugenol.
- 10.
Placement of a definitive restoration. An excellent coronal seal needs to be provided to prevent further micro-leakage (Figs. 8.3 and 8.4).
 Fig. 8.3Diagrammatic representation of the modified stepwise excavation technique. (a) Preoperative view showing deep caries (DC) overlying the pulp (P), (b) interim caries removal from periphery and infected deep carious dentine (DC) which is sealed with a temporary restoration (TR) for 6–8 months (c) note deep carious dentine has changed to a harder demineralised dentine (DD) which is easier to remove without causing a pulpal exposure at the 6–8-month second appointment and (d) final coronal seal (CS) with appropriate lining (L) overlying the pulp
Fig. 8.3Diagrammatic representation of the modified stepwise excavation technique. (a) Preoperative view showing deep caries (DC) overlying the pulp (P), (b) interim caries removal from periphery and infected deep carious dentine (DC) which is sealed with a temporary restoration (TR) for 6–8 months (c) note deep carious dentine has changed to a harder demineralised dentine (DD) which is easier to remove without causing a pulpal exposure at the 6–8-month second appointment and (d) final coronal seal (CS) with appropriate lining (L) overlying the pulp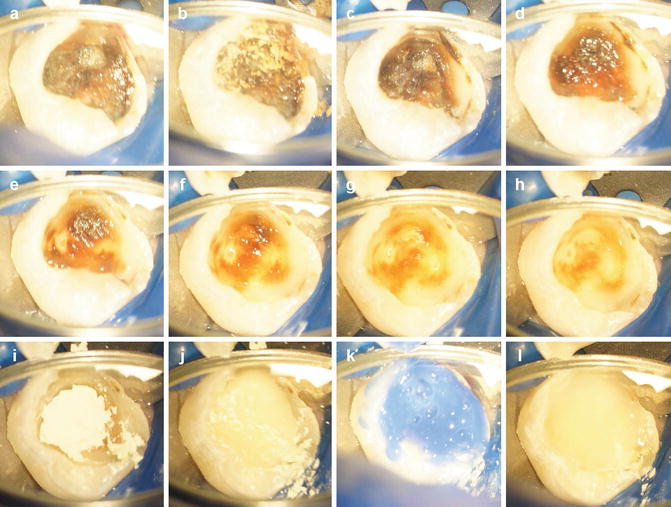 Fig. 8.4Clinical photographs demonstrating indirect pulp capping procedure using MTA. Note (a–h) caries removal leaving in situ stained dentine overlying pulp, (i) MTA placement, (j) GIC base, (k) acid etching and (l) placement of composite resin restoration
Fig. 8.4Clinical photographs demonstrating indirect pulp capping procedure using MTA. Note (a–h) caries removal leaving in situ stained dentine overlying pulp, (i) MTA placement, (j) GIC base, (k) acid etching and (l) placement of composite resin restoration
8.4 Direct Pulp Capping
This treatment option is limited to the permanent dentition and not recommended for the management of pulpal exposures in the primary dentition. The aim of the treatment is to encourage the formation of a dentine bridge at the site of pulpal exposure by encouraging the formation of reparative dentine. This allows the preservation of the underlying pulp and its continuing vitality based on the assumption that the tooth is asymptomatic and the tooth is considered vital.
The procedural steps include:
- 1.
Preoperative radiograph such as a parallel bitewing and parallel periapical confirming carious lesion and proximity to pulp.
- 2.
Standard local anaesthetic protocol to provide adequate anaesthesia.
- 3.
The use of rubber dam to isolate the tooth being treated.
- 4.
Gross caries is removed using either a sharp spoon excavator or a large, round slow-speed tungsten carbide bur. Caries detector dye can be used with appropriate magnification (operating dental microscope).
- 5.
As the pulp is approached, the cavity can be flushed with sodium hypochlorite solution to reduce the bacterial load.
- 6.
The remaining affected carious tissue is removed.
- 7.
Pulpal bleeding can be controlled by either gentle application of cotton wool pledget soaked in water/saline or sodium hypochlorite for up to 10 min. Care should be taken to avoid the application of too much pressure on the pulp.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


