A 33-year-old woman with severe facial asymmetry and unilateral lingual crossbite was treated with orthodontics combined with differential maxillary impaction and intraoral vertical ramus osteotomy. After 12 months of preoperative orthodontic treatment, 2-jaw surgery was performed. The total active treatment time was 18 months. Both her occlusion and facial appearance were significantly improved by the surgical-orthodontic treatment. The occlusion was stable after 5 years of retention. Posttreatment records after 5 years showed excellent results with good occlusion and long-term stability.
Patients with crossbite have significantly more cuspal interferences than those who have a normal transverse occlusion. Frequently, a functional shift occurs when an occlusal interference exists as the mandible closes into centric occlusion. It has been reported that a lateral functional shift of the mandible occurs in about 80% of deciduous and mixed dentitions with posterior unilateral lingual crossbite. Thus, the mandibular dental midline deviates toward the crossbite side relative to the maxillary midline and results in a subdivision malocclusion on the crossbite side. Previous studies have indicated that posterior unilateral lingual crossbite develops early and has a low rate of spontaneous correction. In addition, the condylar position becomes asymmetric when the condyle on the crossbite side is forced upward and backward, while the condyle on the noncrossbite side is distracted downward and forward relative to the glenoid fossa.
In contrast to children, a functional shift is rarely found in adults with a posterior unilateral lingual crossbite. Age-related adaptive remodeling changes in the temporomandibular joint might lead to a skeletal asymmetry. However, studies that have documented the skeletal remodeling of the temporomandibular joints of untreated adults with unilateral posterior crossbite are inconsistent. Pirttiniemi et al concluded that complete adaptation of the temporomandibular joint did not occur in adults with posterior unilateral lingual crossbite. On the contrary, O’Byrn et al and Cohlmia et al demonstrated that the temporomandibular joint complex adapted to mandibular displacement by remodeling of the glenoid fossa and the condyle.
In growing patients, several studies have hypothesized that a functional condylar adaptation to mandibular displacement can develop into a morphologic asymmetry. Schmid et al found that the mandibular ramal height on the crossbite side remained relatively shorter in the growing patient. They proposed that the lateral occlusal interferences cause changes in the mandibular remodeling process. Mandibular growth modification and displacement subsequently progress into mandibular and facial asymmetry.
Although there is still a considerable lack of knowledge concerning the underlying etiology, facial asymmetry appears to originate from a combination of genetic and environmental factors. Correction of unilateral lingual crossbite with facial asymmetry has been a difficult treatment in orthodontics.
This article reports the treatment of a woman with severe facial asymmetry. She had mandibular deviation to the right, vertical maxillary asymmetry, severe midline deviation, and unilateral lingual crossbite. Her treatment included differential maxillary impaction and intraoral vertical ramus osteotomy combined with orthodontic therapy.
Diagnosis and etiology
A 33-year-old woman was referred to an orthodontist (K.T.) for evaluation. She was healthy and had no specific medical problems. Her chief complaints were her mandibular asymmetry and unilateral crossbite. She did not have a history of injury to her head or jaw. Her frontal facial photograph showed severe facial asymmetry, and the mandible was deviated to the right. The cause of the facial asymmetry seemed to be the difference between the right and left heights of the maxilla and the length of the mandibular left and right body ( Fig 1 ).

Clicking sounds were detectable in the right and left temporomandibular joints. However, the patient did not have muscle or joint pain or other symptoms typically associated with temporomandibular disease.
Intraorally, she had anterior and posterior crossbites from the maxillary right lateral incisor to the second molar. The maxillary left segment was constricted on the opposite side of the posterior crossbite and was asymmetric. The mandibular second premolars were severely tilted mesially and were not in occlusion. The mandibular first molars were also tilted mesially. The mandibular left third molar was not in occlusion and was positioned buccally. The maxillary right lateral incisor had a yellowish discoloration. She had moderate crowding in the maxillary arch and severe crowding in the mandibular arch. She had Class III canine and molar relationships on the left side, and a Class II canine relationship and a Class I molar relationship on the right side. The maxillary dental midline was coincident with the labial frenum when she smiled; however, compared with her facial midline, her maxillary dental midline was deviated to the right about 1.2 mm. Her mandibular dental midline was shifted 8.4 mm toward the right. When her mandible was guided into centric relation, a functional shift was seen, because of the anterior and posterior crossbites ( Figs 1 and 2 ).

The posteroanterior cephalometric radiograph showed that the occlusal plane canted down on the left side. In addition, with asymmetric mandibular growth, the chin deviated to the right side ( Fig 3 , A ). The Rocky Mountain transverse analysis showed that the difference between the expected and actual differentials of the mandibular and maxillary widths was 1.4 mm, considerably less than 5 mm. Therefore, surgically assisted rapid palatal expansion might not be indicated, even though the maxillary left segment showed constriction.
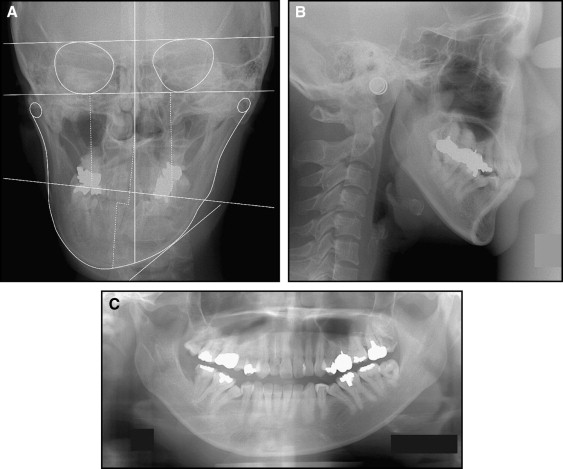
Cephalometric analysis indicated a skeletal Class II pattern (ANB, 6.2°). However, because of the clockwise rotation of the jaws relative to the sella-nasion line, the Wits appraisal was −2.1 mm, along with a hyperdivergent growth pattern (SN-MP, 45.6°). The maxillary incisors had normal inclinations (U1 to SN, 104.0°), whereas the mandibular incisors were retroclined (IMPA, 85.6°) ( Fig 3 , B ; Table I ).
| Measurement | Japanese norm | Pretreatment | Posttreatment | 5 years posttreatment |
|---|---|---|---|---|
| SNA (°) | 82.0 | 89.4 | 85.1 | 83.2 |
| SNB (°) | 80.0 | 83.2 | 79.4 | 78.3 |
| ANB (°) | 2.0 | 6.2 | 5.7 | 4.9 |
| Wits (mm) | 1.1 | −2.1 | −3.3 | −5.1 |
| SN-MP (°) | 32.0 | 45.6 | 47.7 | 47.8 |
| FH-MP (°) | 25.0 | 39.8 | 41.5 | 38.5 |
| LFH (ANS-Me/N-Me) (%) | 55.0 | 57.3 | 59.7 | 59.4 |
| U1 to SN (°) | 104.0 | 104 | 97.3 | 94.7 |
| U1 to NA (°) | 22.0 | 14.6 | 12.4 | 11.5 |
| IMPA (°) | 90.0 | 85.6 | 85.4 | 84.6 |
| L1 to NB (°) | 25.0 | 34.3 | 32.6 | 30.7 |
| Upper lip (mm) | 1.2 | −2 | −0.5 | −0.3 |
| Lower lip (mm) | 2.0 | 0.8 | −1.8 | −0.2 |
In the panoramic radiographic evaluation, the left condyle was enlarged and elongated, and the left ramal height and mandibular left body length were increased. The right lower border of the mandible was bowed downward more than the left side ( Figs 3 , C , and 4 ; Table II ). She was missing her mandibular right third molar. She also had root canal treatments of the maxillary right lateral incisor, the maxillary left second premolar, and the maxillary left second molar, and several restorations of her posterior teeth. Radiolucent areas were found under the crowns of the mandibular right second molar and the maxillary left third molar ( Fig 3 , C ).
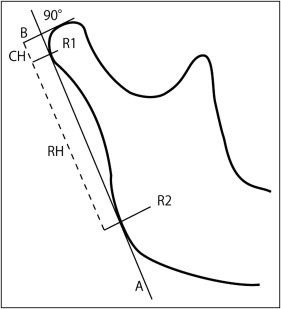
| Parameter | Pretreatment | Posttreatment | ||
|---|---|---|---|---|
| Right | Left | Right | Left | |
| CH (mm) | 3.8 | 4.3 | 3.6 | 3.8 |
| RH (mm) | 34.0 | 38.3 | 35.0 | 36.6 |
| CH + RH (mm) | 37.8 | 42.6 | 38.6 | 40.4 |
| Condylar asymmetry index | 6.2 | 2.7 | ||
| Asymmetry index | 5.9 | 2.2 | ||
The etiology of the severe facial asymmetry and unilateral lingual crossbite appeared to be a combination of hereditary and environmental factors.
Treatment objectives
The following treatment objectives were established: (1) correct the jaw deformities of the maxilla and the mandible; (2) coordinate the skeletal and dental midlines; (3) correct and coordinate the maxillary and mandibular arch forms; (4) obtain normal overjet and overbite; (5) establish Class I canine and molar relationships; (6) correct the irregularities in her teeth; and (7) improve her facial esthetics and symmetry.
Treatment objectives
The following treatment objectives were established: (1) correct the jaw deformities of the maxilla and the mandible; (2) coordinate the skeletal and dental midlines; (3) correct and coordinate the maxillary and mandibular arch forms; (4) obtain normal overjet and overbite; (5) establish Class I canine and molar relationships; (6) correct the irregularities in her teeth; and (7) improve her facial esthetics and symmetry.
Treatment alternatives
Because of the severe skeletal asymmetry, orthognathic surgery was unavoidable. The Rocky Mountain transverse analysis indicated that a surgically assisted rapid palatal expansion would not be considered as a treatment option. However, because of the severity of the lingual unilateral crossbite, the possibility of surgically assisted rapid palatal expansion would be reevaluated after preoperative orthodontic treatment. To improve her facial symmetry, 2-jaw surgery was considered. After comprehensive assessment of the diagnostic records, because the patient had a vertical maxillary height difference and an occlusal plane cant, counterclockwise differential impaction of the maxilla and concurrent mandibular osteotomy would be performed to improve her facial symmetry. Both sagittal split ramus osteotomy and intraoral vertical ramus osteotomy have been widely used for mandibular osteotomy to set back the mandible, but intraoral vertical ramus osteotomy is more likely to improve temporomandibular disorder symptoms and disc position. Therefore, an intraoral vertical ramus osteotomy was selected to improve the facial esthetics and the temporomandibular disorder symptoms. Because of the severe occlusal cant and mandibular asymmetry, the oral surgeon (A.N.) suggested additional plastic surgery, including a genioplasty after 2-jaw surgery. Since surgically assisted rapid palatal expansion and maxillary LeFort I osteotomy cannot be performed simultaneously, the patient would require 2 stages of surgery if it was deemed that the surgically assisted rapid palatal expansion was needed as an adjunctive treatment. However, many patients are reluctant to undergo multiple surgical procedures, and the demand for reducing the number of surgeries might increase. Phillips et al reported considerable relapse after expansion with LeFort I and concurrent segmental osteotomy. Surgically assisted rapid palatal expansion before maxillary LeFort I osteotomy, therefore, was expected to show superior stability compared with LeFort I and concurrent segmental osteotomy, since it allows tissue adaptation during the expansion and subsequent consolidation period. However, the possible increases in surgical trauma, morbidity, and costs were concerns to both the practitioner and the patient.
Nonsurgical palatal expansion is more feasible than surgically assisted rapid palatal expansion; however, to prevent detrimental periodontal effects such as bony dehiscence and to establish proper posterior occlusion, ample orthopedic expansion of the basal bone that minimizes dentoalveolar tipping is essential. To achieve more basal expansion, the appliance should be designed to appropriately maximize the skeletal effects. Despite promising clinical results, miniscrew-assisted rapid palatal expansion cannot force the separation of obliterated sutures in older patients. The indications for miniscrew-assisted rapid palatal expansion should be confined to young adults from the late teens to the midtwenties, based on an earlier study. For older patients, surgically assisted rapid palatal expansion is still the treatment of choice, so a miniscrew-assisted rapid palatal expander was not proposed to this patient. The usefulness of titanium screws for orthodontic anchorage to correct a canted occlusal plane was presented to her, but she did not want temporary skeletal anchorage devices.
Treatment progress
Before orthodontic treatment, the patient was referred to specialists for evaluation of her periodontal conditions, root canal treatments, restorations, and extraction of third molars. Full fixed 0.022-in tip-edge (TP Orthodontics, LaPorte, Ind) appliances were placed in both arches. The maxillary and mandibular arches were leveled with continuous archwires, starting with 0.014-in nickel-titanium and working up to 0.019 × 0.025-in beta-titanium. During treatment, to correct the lingual crossbite, a 0.016-in Australian archwire (A J Wilcock Pty Ltd, Whittlesea, Australia) with active omega loops was used for 3 months. The lingual crossbite was corrected without surgically assisted rapid palatal expansion, and a complete arch alignment and coordination were done in preparation for the orthognathic surgery. Before the surgery, 0.019 × 0.025-in stainless steel archwires were placed. At 12 months, the 2-jaw orthognathic surgery was performed involving a maxillary LeFort I osteotomy for posterior differential impaction and a concurrent mandibular setback with an intraoral vertical ramus osteotomy. The distal segment of the mandible was repositioned 5 mm to the left side to correct the midline with the intraoral vertical ramus osteotomy. Maxillomandibular fixation was maintained for 2 weeks followed by neuromuscular and occlusal rehabilitation for 3 months with elastics and self-physical therapy involving mouth-opening exercises. Occlusal settling was performed with vertical elastics. All brackets and bands were removed 6 months after surgery. Fixed retainers were attached on the maxillary and mandibular anterior teeth. A maxillary circumferential retainer was also used to secure the stability of the maxillary arch ( Figs 5 and 6 ).




