Fig. 6.1
(a) Maxillary right first primary molar opened for RCT, showing the orifices of the three canals. (b) Maxillary right first primary molar, internal morphology (Courtesy of Prof. Eliezer Eidelman, Dr. Odont., M.S.D.). (c) Silicone models of maxillary first primary molars obtained after injection under pressure into the root canals and complete dissolution of the tooth material. Notice the intricate morphology of the root canal system
Like the first primary molars, second primary maxillary molars (Fig. 6.2a) have three roots, and some exhibit fusion between the DB and palatal roots, with the palatal root being the longest, followed by the MBone. The DB root is the shortest and roundest of the three roots [6]. Second primary maxillary molars have either three canals (70 %) or four canals (30 %) (Fig. 6.2b) [8].
Fig. 6.2
(a) A second primary maxillary molar opened for RCT, showing the orifices of the three canals. (b) Maxillary right second primary molar, internal morphology (Courtesy of Prof. Eliezer Eidelman, Dr. Odont., M.S.D)
Mandibular primary molars can have one to three roots; the double-rooted variant is the most common.
Figures 6.3a, b illustrate mandibular first primary molars. Mandibular first molars have normally two roots; both are wider in the buccal-lingual dimension, narrower mesiodistally, and often grooved [6]. Mandibular first molars have either three canals (80 %) or four canals (20 %), the mesial roots usually have two root canals, and the distal root has one or two canals [4]. Mean root canal length of first mandibular molar: mesiobuccal 16.4 mm, mesiolingual 14.2 mm, distobuccal 13.1 mm, and distolingual 12.7 mm [9].
Fig. 6.3
(a) Mandibular first primary molar opened for RCT, showing the orifices of the three canals in the first molar. (b) Mandibular right first primary molar, internal morphology (Courtesy of Prof. Eliezer Eidelman, Dr. Odont., M.S.D)
Mandibular second molars have normally two roots, mesial and distal, and four canals (Fig. 6.4a, b) [6]. Mean root canal length of second mandibular molar: mesiobuccal 15.8 mm, mesiolingual 14.4 mm, distobuccal 14.9 mm, and distolingual 14.9 mm (Fig. 6.4b) [9].
Fig. 6.4
(a) Mandibular second primary molar opened for RCT, showing the orifices of the three canals. (b) Mandibular second primary molar, internal morphology (Courtesy of Prof. Eliezer Eidelman, Dr. Odont., M.S.D)
6.3 Primary Tooth Root Canal Physiology and Anomalies
Roots of the primary teeth will begin to resorb as soon as the root length is completed. This resorption causes the position of the apical foramen to change continually [5]. Because of accessory canals, interradicular bone lesion in inflamed primary molars can be found anywhere along the root and especially in the furcation area [4, 10]. Other root canal anomalies that should also be taken into consideration include taurodontism, a tooth with an enlarged pulp chamber, apical displacement of the pulpal floor, and no constriction at the level of the cementoenamel junction as characteristic features, single-rooted primary maxillary molars or C-shaped canal orifice [4], but as they do not require modification of the pulpectomy technique, this entity would not be dealt with separately.
6.4 Pulpal and Periapical Diagnostics
An undistorted radiograph before performing root canal treatment is essential to assess canal morphology (Fig. 6.5) [11].
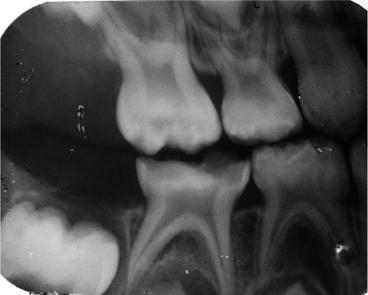
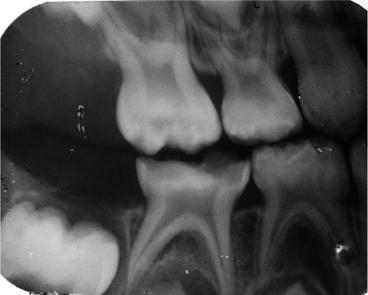
Fig. 6.5
The radiograph performed before root canal treatment (in this case, of the lower right second primary molar) should demonstrate the pulp chamber and the full length of the canals
The success of endodontic treatment depends on elimination of the infecting bacteria accomplished through adequate root canal debridement (instrumentation), antibacterial irrigations, and antibacterial filling materials [12]. Root canal treatment is considered successful if after a follow-up period the tooth (1) is not mobile; (2) remains in function without pain, discomfort, or infection until the permanent successor is ready to erupt; and (3) undergoes physiologic resorption [13]. Radiographically the tooth should present absence or reduction in size of preexisting pathologic radiolucent defects and no new lesions.
6.5 Indications and Contraindications for RCT in Primary Teeth
Root canal treatment in primary teeth is indicated when the radicular pulp exhibits clinical signs of irreversible pulpitis or pulp necrosis, while the roots show minimal or no resorption. Contraindications for RCT in primary teeth are discussed lengthily in the literature [5, 13, 14]. Root canal treatment in primary molars is contraindicated in teeth: (1) with non-restorable crowns, (2) perforation to the pulpal floor, (3) serious reduction in bone support and/or extreme tooth mobility, (4) radiographic indication of extensive internal or external root resorption, (5) periradicular radiolucency involving the follicle of the permanent tooth, and (6) underlying dentigerous or follicular cysts and of medically compromised children [15, 16].
Lateral and accessory canals exist in most primary molars and are more prevalent in mandibular molars compared with maxillary ones [17]. Accessory canals in the furcation of primary molars can explain the frequent presence of radiolucency in the furcation area of necrotic of teeth [10, 18].
A RCT in a primary second molar with a poor prognosis is sometimes indicated, even if that tooth is maintained only until the first permanent molar has erupted, and then the primary molar is extracted and replaced with a space maintainer [19].
6.6 Root Canal Treatment (RCT) Techniques
RCT in primary teeth may be completed in one visit. Under local anesthesia and rubber dam isolation, caries is removed and access to the pulp chamber is gained.
6.6.1 Access and Debridement
The inflamed or necrotic pulp is removed and access preparation is refined to make sure that entrance to all of the canals is possible and clearly visible.
Primary molar roots are usually curved to allow for the development of the succedaneous tooth. During instrumentation, these curves increase the chance of perforation of the apical portion of the root or the coronal one-third of the canal into the furcation [5]. After each canal orifice has been located, a properly sized barbed broach is selected. The broach is used gently to remove as much organic material as possible from each canal. Endodontic files are selected and adjusted to stop 1–2 mm short of the radiographic apex, with the preliminary working length estimated according to the preoperative radiograph. The instruments should be slightly bent to adjust to the curvature of the canals, thus preventing perforations on the outer and inner portions of the root (Fig. 6.6) [5].
Fig. 6.6
Perforations on the convex (1) and concave (2) aspects of a root of a primary molar caused by injudicious use of root canal instruments
Removal of organic debris is the main purpose of canal instrumentation. Mechanical removal of remnants from the canal is performed using a series of 21 mm long K-type endodontic files (Unitek Corp., Monrovia, CA) up to file No. 30 or 35 (Fig. 6.7). The initial working length is estimated with the x-ray. When the file is inserted into the canal, the apical stop is felt for with tactile sense and this measurement is then compared to the radiograph. Avoid unnecessary shaping of the canal since that can damage the tooth and lead to perforation in the furcation or the lateral walls.


Fig. 6.7
Mechanical removal of remnants from the canal is performed using a series of 21 mm long K-type endodontic files (Unitek Corp., Monrovia, CA) up to file No. 30 or 35
6.6.2 Irrigation
Disinfection with irrigating solutions is an important step in assuring optimal bacterial decontamination of the canals. The root canals are irrigated with either 0.2 % up to 2 % chlorhexidine solution or with 1 % up to 5 % sodium hypochlorite (limited to one percent sodium hypochlorite according to the AAPD guidelines) (Fig. 6.8) [3, 4, 20–23].


Fig. 6.8
The root canals are first irrigated with either 0.2 % up to 2 % chlorhexidine solution or with 1 % up to 5 % sodium hypochlorite and then with normal saline
The use of sodium hypochlorite in the primary dentition should be performed cautiously since it is a potent tissue irritant and must not be extruded beyond the apex [24–27] (Fig. 6.9).


Fig. 6.9
Sodium hypochlorite accident in a pediatric patient. (a) Presentation in the postanesthesia care unit. (b) Presentation 1 day after the surgery. (c) Presentation 2 days after surgery. (d). Complete uneventful recovery 6 weeks after the surgery (Copyright © Klein and Kleier [26]. American Academy of Pediatric Dentistry and reproduced with their permission)
Irrigation with normal saline before drying with appropriately sized sterile paper points (shown in Fig. 6.10) is also recommended. There is insufficient evidence supporting the outright superiority of any specific individual irrigation material or irrigating regime. Except anecdotal case reports, no evidence-based studies reported any adverse effects, and it is not clear if there were none or that they were just not reported, and thus the safety profile for each of the irrigating solutions remains unclear [28].


Fig. 6.10
Drying the canals should be performed with appropriately sized sterile paper points
6.6.3 Filling the Canal(s)
The instruments employed to fill the canals depend mainly on the material used.
Thick paste such as ZOE is inserted and condensed with root canal pluggers, while thinner pastes like iodoform and calcium hydroxide-based materials are inserted with a spiral lentulo mounted on a slow-speed engine (Fig. 6.11: a spiral lentulo). Other materials are inserted with plastic syringes and tips provided by the manufacturer (Fig. 6.12: plastic syringe).
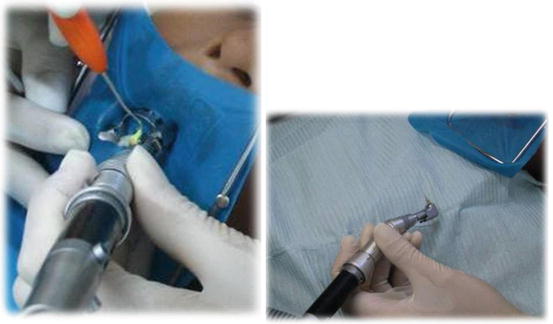

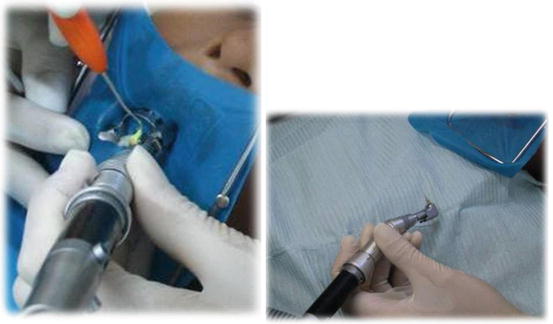
Fig. 6.11
Materials are inserted with a spiral lentulo mounted on a slow-speed engine

Fig. 6.12
Insertion of paste with a plastic syringe
6.7 Root Canal Filling Materials
The ideal root canal filling material should resorb at the same pace as the physiologic resorption of the roots, be nontoxic to the periapical tissues and to the permanent tooth germ, resorbs readily if forced beyond the apex and be antiseptic, easy to insert, nonshrinkable, and easily removed if necessary [19].
A number of root canal filling materials can be used for primary teeth, with no known ideal root canal filling material. Table 6.1 describes various popular root canal sealers for primary teeth. According to the literature, the most adequate material appears to be a calcium hydroxide-iodoform mixture [37]. Calcium hydroxide provides the high pH (>10) environment that, along with iodoform, has a high bacteriostatic effect [38].
Table 6.1
A description of various root sealers for primary teeth
|
Root filling material
|
Zinc oxide-eugenol
|
Calcium hydroxide with iodoform
|
Calcium hydroxide
|
Iodoform based
|
Zinc oxide and iodoform
|
|---|---|---|---|---|---|
|
Components
|
Vitapex (New Dental Chemical Products Co. Ltd., Tokyo, Japan)/ Diapex: 30 % calcium hydroxide, 40.4 % iodoform, and 22.4 % silicone oil.
|
Sealapex
Calcicur
|
Metapex (Meta Biomed Co., Ltd. Cheongju City, Korea): calcium hydroxide with iodoform
Kri paste(Pharmachemie AG, Switzerland): iodoform (80.8 %), camphor, parachlorophenol, menthol
|
Maisto’s paste: zinc oxide and iodoform, with parachlorophenol camphor, lanolin, and thymol
Endoflas (Sanlor & cfa. S. en C.S. from Columbia South America): tri-iodmethane and iodine dibutilorthocresol (40.6 %), zinc oxide (56.5 %), calcium hydroxide (1.07 %), and barium sulfate (1.63 %) with a liquid consisting of eugenol and paramonochlorophenol
|
|
|
Usage
|
Without setting accelerators may be pushed into the root canals using a suitable root canal plugger
|
Introduced into the root canal using disposable tips or a spiral lentulo mounted on a slow-speed handpiece
|
Introduced into the root canal using a spiral lentulo. Also available in automix syringes or application cannula
|
Sterile syringe with disposable plastic needles injects the paste into the canal
|
Introduced into the root canal using a spiral lentulo mounted on a slow-speed handpiece
|
|
Difficulties
|
Aqueous vehicles cause depletion of paste from root canals before the time of physiological tooth replacement [31]a
|
Showed minimal antibacterial activity against most pure cultures [34]
Overfilling and voids [35]
|
|||
|
Antibacterial activity
|
Showed no antibacterial activity against most pure cultures [36]
|
Kri paste showed stronger antibacterial effectiveness than did ZOE [36]
|
The following paragraph describes several commonly used root canal filling materials. The characteristics of each material contribute its efficacy and biological behavior.
Zinc oxide-eugenol paste
A thick mix of ZOE (Zinc Oxide BP, Eugenol BP, Associated Dental Products Ltd, Purton, England) without setting accelerators may be pushed into the root canals using a suitable root canal plugger. ZOE tends to resorb at a slower rate than the roots of the primary teeth [29–31], so placing it in the root canals can create a problem to the clinician: When extruded beyond the apices, the material sets into a hard cement that resists resorption (Fig. 6.13) [1, 39–42], it appeared in the tissue after loss of the pulpectomized tooth in 49.4 % of the cases [42], and it might remain in the alveolar bone for months or years (27.3 % of cases after a mean time of 40.2 months [42]). Remnants of ZOE may cause a mild foreign body reaction [43]. While in the USA, the use of ZOE without setting accelerators has been previously recommended [44]; currently the tendency is to use iodoform/calcium hydroxide filler [45].


Fig. 6.13
ZOE extruded beyond the apices set into a hard cement that resists resorption (left and center). The remnants of the ZOE are still present after the eruption of the permanent central incisor
Calcium hydroxide pastes with iodoform
The antimicrobial action of calcium hydroxide is associated with its ionic dissociation. The aqueous, viscous, or oily vehicle used in the formulation of the root canal filling paste impacts the speed of ionic dissociation. As aqueous vehicles favor a high degree of solubility, they will cause a depletion of the paste from the root canals before the time of physiological root resorption [31]. Viscous vehicles promote a lower solubility of the paste, and oily vehicles have the lowest solubility and diffusion of calcium hydroxide pastes showing better results [32, 33]. Iodoform-containing pastes such as Vitapex (prefilled syringe with 0.5 g paste, Dia Dent Co., Tokyo, Japan) are introduced into the root canal using disposable tips or a spiral lentulo mounted on a slow-speed handpiece, and the teeth are sealed with reinforced zinc oxide-eugenol (IRM – L.D. Caulk, Dentsply Milford, DE). Vitapex is a combination of 30 % calcium hydroxide, 40.4 % iodoform, and 22.4 % silicone oil. It is radiopaque, premixed, easy to use (plastic syringe tip) (Fig. 6.12) and to remove and absorbed if inadvertently extruded past the apex [38]. In primary teeth with irreversible pulpal changes, ZOE pulpectomies yielded similar outcomes as Vitapex and more favorable than Sealapex, a calcium hydroxide cement (SybronEndo, Orange, CA), although there was no agreement with regard to filling materials’ resorption [46]. Vitapex is sold in North America as Diapex (DiaDent Group International, Burnaby, BC, Canada). When extruded into furcal or apical areas, it can either diffuse or be resorbed in 1 or 2 weeks. Bone regeneration has been clinically and histologically documented [47]. Tchaou et al. employed pure cultures of bacteria that have been reported to inhabit non-vital root canals of primary teeth and found that Vitapex did not inhibit the growth of S. mutans, S. aureus, or L. casei and showed no antibacterial activity against most pure cultures [36].
Iodoform-based pastes
Maisto’s paste, introduced in 1967, includes both zinc oxide and iodoform, with parachlorophenol camphor, lanolin, and thymol. The presence of zinc oxide slows it resorption, and it was reported to have significantly higher success rates (100 %) compared to ZOE alone [38, 49, 50].
KRI paste (Pharmachemie, Zurich) is a mixture of iodoform (80.8 %), camphor, parachlorophenol, and menthol [38, 51, 52]. KRI paste showed stronger antibacterial effectiveness than did ZOE against pure cultures of obligate anaerobes with Bacteroides (currently Porphyromonas Prevotella) species and anaerobic streptococci isolated from non-vital root canals of primary teeth [36].
6.8 Supplementary Methods
Dental operating microscopes, electronic apex locators, rotary nickel-titanium files and irrigation techniques are at the front of endodontic armamentarium today [4, 13, 53–64].
The use of dental operating microscope [4] is not essential when treating primary teeth. Preparation of root canals in primary teeth (contrary to permanent teeth) is based on chemical means rather than on mechanical debridement [13].
When considering the use of electronic apex locators, only few studies exist and most of them are either in vitro [53, 65] or studies performed under general anesthesia [54, 55, 66–68]. Those studies recommend further evaluation of the application of apex locators in primary teeth, but as of now it is not yet an established procedure.
As for rotary instrumentation techniques in primary molars, in vitro studies found equal cleaning capacity but reduction of instrumentation time by the rotary technique [56–60]. The use of the rotary technique reduced the time of instrumentation and obturation to 63 and 68 %, respectively, and also improved the quality of the root canal filling [56, 61, 63]. The reduction of RCT procedure time is a relevant clinical factor in the treatment of children, but, due to lack of in vivo appropriate studies, it is not yet possible to recommend the use of rotatory filing technique as a standard procedure.
Er,Cr:YSGG laser provided similar cleanliness as rotary instrumentation technique and was superior to manual instrumentation. The laser technique required less time for completion of the cleaning and shaping procedures when compared with both rotary or hand instrumentation [64]. Here too, due to the limited clinical studies and the lack of adequate follow-up, this technique cannot be yet recommended for common practice, and so manual instrumentation is still the preferred debridement method for root canals in US dental schools and practiced by Diplomats of the American Board of Pediatric Dentistry in the USA [45].
6.9 Evaluation of RCT
RCT is considered successful if clinically pretreatment clinical signs and symptoms resolve within a few weeks and the tooth is painless, presenting healthy surrounding soft tissues and no increased mobility. The treatment should permit resorption of the roots of the primary tooth and filling material and allow normal eruption of the succedaneous tooth.
Radiographic lesions present preoperatively should resolve within 6 months, as evidenced by bone deposition and a decrease or disappearance or at least no change in pretreatment radiolucent areas. No pathologic root resorption, furcation/apical radiolucency [31, 50], or new lesion should appear after treatment.
Radiographically, success is defined either as when the radiolucency observed at the baseline did not increase [69] or is decreased in size [30, 70, 71] or when there is no radiolucency in the furcal or periradicular areas In all trials, success rates were equal to or above 78 %.
Treatment is considered a failure when preexisting radiolucent defects have grown in size or new defects appeared.
Success rate of root canal treatments in primary teeth has been discussed in the literature. Success rates were around 53 % in an early study [72] that used a different technique than the average pulpectomy that is performed today. Later studies have reported success rates of 95 and 99 % [5]. More recent studies achieved a success rate of 82 to 90 % for primary molar RCT with a ZOE filling material [73, 74]. The success rate of RCT in the anterior teeth varied from 76 to 82.8 % [1, 30, 75–78]. When using Kri Paste, the rate of successful treatments with no clinical or radiographic signs or symptoms was from over 80 % up to as high as 95.6 % [16, 40, 41, 51, 79–81].
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


