Fig. 3.1
Facial swelling and cellulitis as result of dentoalveolar abscess affecting maxillary primary molar (Courtesy of Dr. Abi Adewumi, University of Florida)
Fig. 3.2
(a) Facial cellulitis involving buccal and infraorbital space of a 7-year-old patient; (b) periapical radiograph reveals deep caries lesion affecting teeth #64 and #65 which are non-restorable; (c) normal facial appearance 6 days post-extraction of affected teeth (Courtesy of Dr. Chelsea Brinkman, Pediatric Dental Resident, University of Florida)
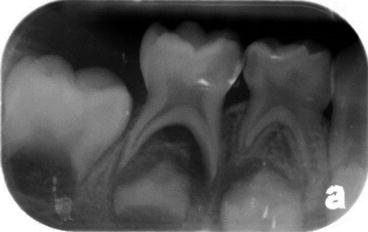
Fig. 3.3
Deep carious lesion of tooth #85 with large furcation and periapical involvement with close proximity to developing second premolar
During intraoral examination, the clinician should perform a careful soft tissue assessment searching for signs of swelling of the vestibule, presence of sinus tracts which may be associated with teeth affected by trauma (Fig. 3.4), caries, or deep restorations in close proximity to the pulp (Fig. 3.5a–d).


Fig. 3.4
Traumatic injury affecting tooth #61 resulting in discoloration, pulp necrosis, and sinus tract
Fig. 3.5
(a, b) Intraoral sinus tract caused by a necrotic pulp and a deep amalgam restoration on tooth #54. Note that the crown is partially covered by the lower lip. (c, d) Healing of the area after extraction of tooth # 54, 10 weeks’ post-extraction (Courtesy of Dr. Jeffery Jackson, Pediatric Dental Resident, University of Florida)
When examining hard tissues, teeth with questionable diagnosis should be evaluated for abnormal mobility and sensitivity to percussion. With the presence of open proximal carious lesions between adjacent teeth, the space can serve as reservoir causing food impaction providing false-positive response to percussion test (inflammation of interdental papilla rather than acute pulpal inflammation). In order to avoid behavior management problems, when performing percussion and palpation tests in children, the tip of the finger should be gently used in combination with Tell, Show, and Do (TSD) technique [5]. The clinician should start the test with a contralateral non-affected tooth to familiarize the patient with a normal response to the stimuli.
3.3 Pain Characteristics
Young children are not good historians. For this group, parents are the ones better prepared to reporting existing symptoms. Stimuli-related responses that cease when the insult is removed (provoked or elicited pain) generally indicate a favorable, reversible status of the pulp which could lead to a more conservative treatment approach such as indirect pulp therapy (IPT) or pulpotomy. Complaints of persistent, lingering, or throbbing pain disturbing sleep and preventing regular activity are generally referred as “spontaneous pain.” This most probably indicates an irreversible status of the pulp. The information in combination with clinical examination and radiographic image(s) will lead the clinician to treatment options such as pulpectomy or extraction.
3.4 Sensibility Tests
Sensibility and percussion tests are not indicated in primary teeth due to inconsistent results [6]. Younger patients may also be more anxious and less reliable because of the subjective nature of the test [7]. The most commonly used pulpal sensibility tests are cold and electric pulp tester (EPT) [7, 8]. For a reliable response, teeth need to be dried and well isolated. Adjacent and/or contralateral teeth to the one in question are generally tested first, as controls, to observe a baseline normal response. Refrigerant spray is the most commonly used. It is convenient, user-friendly, and reliable with a level of accuracy higher than EPT [7, 9, 10]. The cold test may be used to differentiate between reversible and irreversible pulpitis. If pain subsides when the stimulus is removed, a diagnosis of reversible pulpitis is appropriate. If a lingering pain persists, irreversible pulpitis is more likely [11]. Jespersen et al. evaluated the pulpal response to cold and EPT in the presence and absence of caries. They found that presence of caries in vital teeth resulted in a more accurate response to cold testing. However, no response to cold on carious teeth makes a diagnosis of pulpal necrosis more accurate [7]. Patients in early mixed dentition and with deep carious lesions affecting permanent molars well tolerated cold test as proof of pulpal vitality before caries excavation [12].
3.5 Preoperative Diagnosis of Deep Caries Lesions
When facing deep carious lesions affecting the primary dentition, limitations exist regarding the determination of the vitality status of the pulp. Percussion and palpations tests, combined with bitewing and selected periapical radiographs, are complimentary information that must be obtained. Good quality bitewing radiographs showing clearly the furcation area are essential for an accurate diagnosis. However, in young children in primary and early mixed dentition, especially when using size #0 or #1 films, visibility of the apical third of the primary molar roots and the apical formation of first permanent molars is not always possible. In these situations, a periapical radiograph should be obtained to rule out the presence of internal resorption or periapical involvement. Figure 3.6a shows a left bitewing of an asymptomatic tooth #75 with a deep carious lesion. The supplemental periapical radiograph discloses neither furcation nor periapical pathology, indicating good prognosis for a conservative pulp treatment such as IPT (Fig. 3.6b). Conversely, a periapical radiograph reveals furcation pathology in tooth # 85, indicating pulp necrosis, not evident in a bitewing (Fig. 3.6c, d). In Fig. 3.6e, internal root resorption and furcation involvement can be observed in a periapical radiograph of a symptomatic tooth #85.
Fig. 3.6
(a) Left bitewing of an asymptomatic tooth #75 with a deep carious lesion; (b) periapical radiograph reveals no furcation pathology indicating good prognosis for a conservative pulp treatment such as IPT. (c) Right bitewing of a 4-year-old patient with spontaneous pain affecting tooth #85 which is sensitive to percussion; (d) a periapical radiograph reveals furcation pathology indicating pulp necrosis; (e) on a different patient, but a similar situation, a periapical radiograph of symptomatic tooth #85 showing internal root resorption and furcation involvement. (f) Bitewing radiograph of a 7-year-old patient showing limited visibility of the roots of the first permanent molar (#36) with a deep carious lesion. (g) A supplemental periapical radiograph reveals normal root development and absence of pathology (Courtesy of Dr. Nicole Eastham, Pediatric Dental Resident, University of Florida)
Success of pulpotomies performed previously in the primary molars of a 7-year-old patient can be observed in a bitewing radiograph. However, the visibility of the roots of the first permanent molar (#36) with a deep carious lesion is limited (Fig. 3.6f). A supplemental periapical radiograph reveals normal root development and absence of pathology (Fig. 3.6g).
Integrity and continuity of the lamina dura together with the presence of trabecular bone in the bifurcation area of primary molars are indicative signs of a vital pulp (Fig. 3.7).
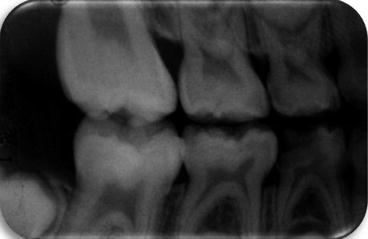
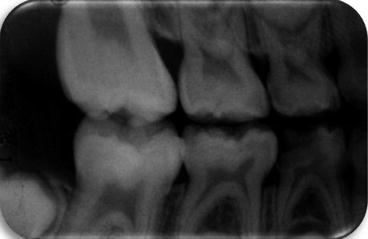
Fig. 3.7
Deep carious lesion affecting tooth #84. Tooth is asymptomatic, lamina dura is continuous, and furcation area is filled with trabecular bone
Due to anatomical differences and superposition of images, clear visualizations of these structures may be difficult to obtain in the maxillary arch [2]. In asymptomatic primary and permanent teeth, the amount of sound dentin (at least 1.0 mm) separating the deepest layer of the caries lesion and the pulp horn can also play an important role when determining if a conservative approach such as IPT is recommended [13]. Recently, a clinical attempt to possibly assess pulpal diagnosis status of deep caries lesions affecting primary molars using interim therapeutic restorations has been advocated [14]. This technique will be discussed in detail in Chap. 4.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


