Pre-operative Evaluation
Kyle D. Hogg
Principles
Planning for the replacement of a missing tooth or missing teeth in the aesthetic zone requires a thorough pre-operative evaluation to facilitate a predictable treatment outcome, meeting the functional and aesthetic requirements as well as the expectations of both patient and provider. A number of treatment modalities can be selected to achieve these requirements, including:
- Orthodontic space closure
- Removable partial denture
- Adhesive or resin-bonded fixed partial denture
- Fixed partial denture
- Dental implant-supported restoration.
Successful prosthetic rehabilitation in the aesthetic zone hinges on selecting the most appropriate treatment option for the individual patient; within the confines of the specific localised clinical situation; and within the broader comprehensive restorative treatment plan.1
Recent systematic reviews have validated the use of dental implant-supported restorations as a means of reliably replacing single or multiple missing teeth, showing excellent survival rates.2
A thorough and meticulous patient assessment based on comprehensive evaluation of the patient is paramount for adequate diagnosis and treatment planning of any dental rehabilitation. A template flow diagram for undertaking a comprehensive patient assessment has been proposed by Mehta et al.3 (Figure 11.1.1).
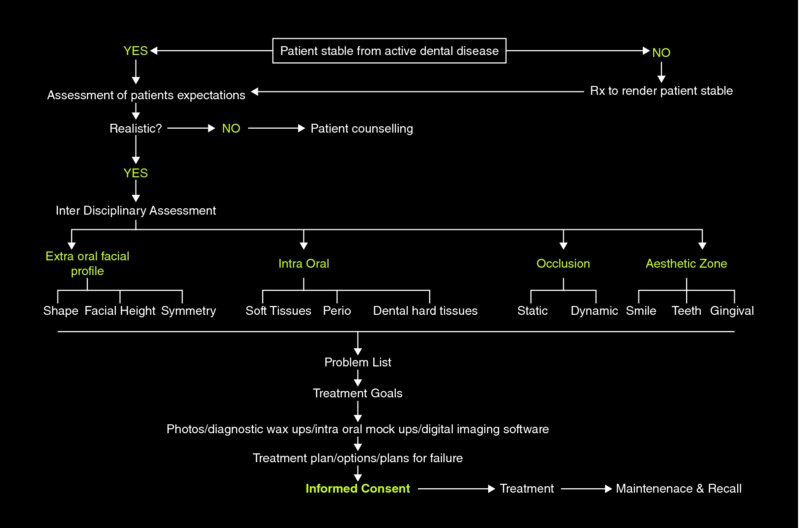
Figure 11.1.1 Flow diagram for undertaking a comprehensive patient assessment. Source: Mehta, Banerji, and Aulakh, 2015. Reproduced with permission from George Warman Publications UK Ltd.
Dental implant rehabilitation is inherently interdisciplinary, with both surgical and prosthetic phases of treatment that require a coordinated assessment. The comprehensive pre-operative assessment for dental implant rehabilitation should begin with the establishment, from the perspective of the patient, of the chief complaint. A thorough medical history review must be undertaken to ensure that the patient is fit to undergo the required surgical and prosthetic procedures. It is important to bear in mind that dental implant therapy is typically elective treatment. Therefore, the patient must not be placed at any undue risk in the pursuit of treatment. Specialist referral for medical consultations may be required or advisable in patients with more compromised conditions or with complex medical histories. The patient must also be satisfactorily stable from active dental disease and have reasonable treatment outcome expectations prior to embarking on a more focused interdisciplinary assessment of the prospective implant sites.
The interdisciplinary assessment includes an intra-oral and extra-oral examination of the patient with an evaluation of the facial aesthetics, temporomandibular joint, muscles of mastication, dental hard and soft tissues, occlusion and both the static and dynamic nature of the aesthetic zone. A thorough and detailed evaluation of the site to be restored with implants is imperative to achieve a successful, restoratively driven treatment outcome. Special diagnostic records, radiographic imaging and diagnostic wax-ups of the proposed restoration provide the surgical and restorative team with valuable information that enables appropriate planning and execution of treatment in a predictable fashion.
Patients must ultimately be educated on the risks, benefits and maintenance requirements of all treatment options that might be suitable for them. In addition to developing a treatment plan, the clinician must also discuss with the patient the steps involved in rendering care, the duration of the planned rehabilitation, the number of visits required, maintenance and the financial obligations of the selected treatment in order to achieve informed consent.
Procedures
Refer to the procedures in Chapter 2.3, ‘Evaluation of the Aesthetic Zone’, for a review of how to perform a comprehensive aesthetic zone evaluation. Evaluating a patient for implant rehabilitation in the aesthetic zone is an extension of the comprehensive aesthetic zone evaluation, with additional patient factors and site-specific factors to be considered.
With your patient comfortably seated upright in the dental chair, and you seated at the same height facing them, ask the patient to describe in their own words what their dental problem is and what they would like to have done to correct the problem. Allow the patient to speak, listening carefully to the patient’s description of both their condition and desired solution without interruption, and repeat it back to the patient in a paraphrased manner. This exercise, while seemingly simplistic, establishes the patient’s chief complaint, provides valuable information on the patient’s preferences, expectations for rehabilitation and level of dental knowledge, and develops trust and rapport between patient and provider.
In the same manner, perform a detailed review of the patient’s medical and social history. Of particular note would be patients with a positive history of radiation therapy to the head and neck, history of taking bisphosphonate medications or who have had bisphosphonate-related osteonecrosis of the jaw (BRONJ), insulin-dependent diabetics, patients with unfinished cranio-facial growth and incomplete tooth eruption (females younger than 18–19 years, males slightly older), patients undergoing immunosuppressant therapy, patients undergoing chemotherapy and heavy smokers. Caution should be taken when considering treating patients with these conditions or others that might prevent or hinder the predictability of soft- or hard-tissue healing, and the long-term survival and success of dental implant rehabilitation. Specialist referral to appropriate medical colleagues for pre-operative evaluation and clearance is advisable for patients who have a complicated medical history or a high American Society of Anesthesiology (ASA) score.
Next, perform an extra-oral clinical examination, as outlined in detail in Chapter 2.3.
Continuing with the intra-oral examination, note the arrangement and condition of the patient’s remaining dentition, occlusal scheme, temporomandibular joint function, presence of parafunctional activity, oral hygiene, periodontal status, caries rate and additional restorative, periodontal, endodontic and orthodontic needs. A complete radiographic survey and periodontal charting are necessary to determine fully whether the patient is stable from active disease, which should be a prerequisite before proceeding to implant rehabilitation.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


