








Porcelain use decreased following the introduction of silicate cements in 1908. Although silicates, a combination of silica alumina and calcium fluoride, showed significant solubility in salivary fluids, the fluoride component provided anticariogenicity. Acrylic resins, introduced in 1946, immediately replaced silicate resins as the esthetic material of choice. Although they exhibited better long-term retention, they did not contain fluoride, which resulted in an increased incidence of recurrent decay. Advances in acrylic resin systems, compared with earlier restorations, controlled some of the polymerization shrinkage, but they still exhibited poor overall dimensional stability. In addition, like silicates, acrylic resins required mechanical retention. The introduction of the acid-etch technique and filled composite resins further diminished the use of porcelain as an internal restorative material. Porcelain, in the form of all-porcelain and porcelain-fused-to-metal restorations, was relegated to full coverage restorations.
In the late 1970s, direct and indirect laminate veneers were introduced. Direct veneers, which used light-cured composite resin to overlay the entire facial surface, allowed great flexibility in both shaping and shading teeth. However, they were time consuming and required substantial artistic skill. In addition, they exhibited poor color stability and wear resistance.
Indirect or preformed veneers attempted to overcome some of these limitations.3 Composed of acrylic, they were treated with ethyl acetate, methylene chloride, or methyl methacrylate and then luted to the etched tooth with a composite resin. Although they exhibited greater color stability and stain resistance than early direct composite resin veneers, the composite resin-to-laminate veneer bond proved to be a fatal weak link.4 The acrylic veneer also exhibited a dull and monochromatic appearance, poor abrasion resistance,5 and resulted in unsatisfactory gingival inflammation.
Porcelain-bonded restorations
Early research6 indicated that it was possible to chemically bond silica to acrylic or bis-GMA using a silane coupling agent. Most research7–9 focused on the direct chemical bonding of porcelain teeth to acrylic denture bases. Early silane bonds prevented seepage of oral fluids between the porcelain-acrylic interface.10 However, differences in the coefficient of thermal expansion between porcelain and acrylic caused bond deterioration during bench cooling of the heat-cured acrylic.
The need for a technique to repair ceramometal restorations with debonded porcelain prompted interest in the composite resin to porcelain bond. It was discovered that no bond formed between the glazed porcelain and composite resin, even with silane,10, 11, 12 unless the surface was roughened.13
In 1983, the porcelain-laminate veneer was introduced.14 It combined the esthetic and positive tissue response of porcelain with the adhesive strength of acid-etch retained restorations and the convenience of a laboratory-fabricated restoration.
Basic chemistry
The porcelain-bonded restoration consists of four components
Porcelain
Dental porcelains are composed of natural feldspar (both potassium and sodium aluminosilicate glasses).15 Early porcelain-laminate veneers used the same porcelains used in all-porcelain restorations. Later, high-strength porcelains specifically designed for bonded restorations were introduced. These materials are stronger than conventional porcelains and composite resin.
Acid etching
Retention of the acid-etch retained porcelain restoration is accomplished by the creation of microporosities in both the porcelain and enamel. Porcelain porosities are derived from treating the internal surface of the restoration with a 10% acid solution, such as hydrofluoric acid. Studies show that etching with or without the use of a silane coupling agent greatly increases bond shear strength, which can even surpass resin-enamel bond strength (Table 7-1).16, 17
Table 7-1
Effects of Etching and Silane on Bond Shear Strength
| Group | Etch | Silane | Bond Shear Strength |
| A | Yes | No | 2907 ± SD 165 |
| B | Yes | Yes | 3485 ± SD 340 |
| C | No | No | 564 ± SD140 |
| D | No | Yes | 978 ± SD390 |
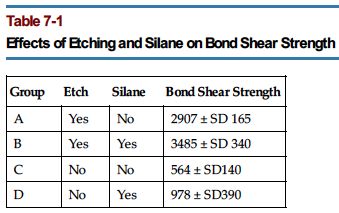
Data from Hsu CS, Stangel I, Nathanson D. Shear bond strength of resin to etched porcelain [abstract 1095]. In Abstracts of papers: 63rd general session, International Association for Dental Research/Annual session, American Association for Dental Research, Las Vegas (1985) J Dent Res 64: 162-379, 1985.
Salivary contamination of the etched porcelain can significantly reduce bond strength. Application of 37% phosphoric acid for 15 seconds has been shown to restore the etched surface.18
Silane coupling agents
The function of a coupling agent is to alter the surface of a solid to facilitate either a chemical or physical process.10 Numerous silane coupling agents exist and are used in dentistry to increase the shear strength of the porcelain-to-composite resin bond.
These agents are believed to be capable of chemically bonding to silica in both the porcelain laminate veneer and the composite resin matrix. Scanning electron micrographs reveal that silane and etching eliminate the polymerization contraction gap, which forms in both etched, nonsilanated and unetched, silanated restorations by allowing the resin to better wet the surface.17 An in vitro study using two different types of feldspathic porcelain concluded that silane combined with the action of hydrofluoric acid gel is the most effective surface treatment for ceramics.19
Composite resin luting cements
Initially, laminate veneers were retained with auto-curing composite resins. Light-activated composite resin luting cements provided increased working time. Numerous viscosities are available. Different shades and opacities allow for color modification of the restoration.
Light-activated resins are ideally suited for most laminate veneers. However, they require sufficient light from a curing light to initiate curing. Therefore they should not be used when the light must travel through a thickness of porcelain that exceeds the manufacturer’s recommendations. Factors affecting this maximum depth include the specific light source, the age of the bulb, the shade and opacity of the laminate, and the shade and opacity of the composite resin cement.
Basic laboratory technique
Porcelain-laminate veneers can be fabricated by the laboratory in one of four ways: platinum foil backing, refractory casts, direct castings, or CAD-CAM machining.
Platinum foil backing.
This method can also be used to construct the all-porcelain crown. A very thin layer of platinum foil is placed on the die. The porcelain is layered on the foil. Then the porcelain-foil combination is removed from the die and fired in an oven. Before try-in, the foil is removed and the porcelain is etched.20
The use of platinum foil permits the porcelain to be repeatedly removed from and replaced onto the die during restoration fabrication. This permits easier access to the proximal margins. In addition, the thickness of foil creates a space for opaques and tinting agents.
Refractory casts.
The use of refractory casts is the most commonly used method of porcelain laminate veneer fabrication.21
The restoration is fired directly on a refractory die. This eliminates the platinum layer but makes repeated firings difficult once the laminate veneer has been removed from the die unless a duplicate refractory die is fabricated.
The advantages of the refractory cast include tighter contacts and the absence of the gap created by the use of platinum foil. The disadvantages are less room for coloring agents and more difficulty in adjusting proximal areas by the technician.
Direct castings.
Cast ceramic restorations are fabricated using the “lost wax” technique. This eliminates the need for multiple firings but requires extrinsic staining for coloration (see Chapter XX).
CAD/CAM machining.
Ceramic restorations can be manufactured either in the dental office or in the laboratory. A cast or video image of the preparation is required, and the restoration always requires modification of the surface porcelain to obtain proper color esthetics. (For a complete discussion, see the section on CAD/CAM systems in Chapter 23.)
Advantages of bonded porcelain restorations
The main advantages of bonded porcelain restorations are the following:
1. Excellent esthetics. Porcelain offers unsurpassed esthetics. Unlike direct laminate veneers, the porcelain laminate veneers depend less on the esthetic skill of the clinician.
2. Excellent long-term durability. Porcelain is both abrasion resistant and color stable. In addition, porcelain has excellent resistance to fluid absorption.
3. Inherent porcelain strength. Porcelain exhibits excellent compressive, tensile, and shear strengths when properly bonded to tooth structure.
4. Marginal integrity. Porcelain restorations bonded to enamel exhibit exceptional marginal integrity.
5. Soft tissue compatibility. Properly polished porcelain is highly biocompatible with gingival tissue.
6. Minimal tooth reduction. Anterior porcelain laminate veneers are considerably more conserving of tooth structure than porcelain-fused-to-metal and all-porcelain full coverage restorations.
Disadvantages of bonded porcelain restorations
The primary disadvantages of bonded porcelain restorations are the following:
1. Time. Multiple visits are required.
2. Cost. Laboratory involvement and additional chair time are required when compared with direct restorations, resulting in higher costs to the patient and clinician.
3. Fragility. Although strong when bonded to the tooth, bonded porcelain restorations are extremely fragile during the try-in and cementation stages.
4. Lack of repairability. Porcelain restorations are difficult, if not impossible, to repair.
5. Difficulty in color matching. Although porcelain restorations are color-stable, precise matching of a desired shade tab or an adjacent tooth can be difficult. In addition, shade alteration is impossible after cementation.
6. Irreversibility. Tooth reduction, although often minimal, is required.
7. Inability to trial cement the restoration. Unlike traditional indirect restorations, bonded porcelain restorations cannot be temporarily retained with a provisional cement for evaluation purposes.
Indications
Porcelain laminate veneers may be indicated in areas traditionally restored with single crowns or composite resin veneers for the following:
Contraindications
Porcelain laminate veneers may be contraindicated for the following:
1. Patients who exhibit tooth wear as a result of bruxism
3. Teeth with insufficient or inadequate enamel for sufficient retention (e.g., severe abrasion)
4. Existing large restorations or endodontically treated teeth with little remaining tooth structure
5. Patients with oral habits causing excessive stress on the restoration (e.g., nail biting, pencil biting)
Diagnostic and treatment planning AIDS
Porcelain laminate veneers can be used to change any or all of the following characteristics of a single tooth or multiple teeth:
Wax and paint simulation
White orthodontic wax and acrylic paint provide an extremely effective diagnostic and patient education aid. This is especially helpful when evaluating the treatment of single or multiple diastemas, and fractured, misshaped, or malpositioned teeth. The wax can be used to quickly and inexpensively simulate (and thereby “preview”) the effects of porcelain laminate veneer placement.
Armamentarium
Clinical technique
1. Isolate the teeth with a one-piece lip retractor (Fig. 7-1 A).
3. Apply the wax to the teeth and grossly mold to shape with the index finger.
4. Refine the wax with the plastic instrument (Fig. 7-1 B, C).
Computer imaging
Computer imaging provides a two-dimensional prediction similar to the three-dimensional preview provided by wax simulation and acrylic paint. This system has the added advantage of previewing the effects of color and characterization changes and providing a more lifelike prognostication. Computer imaging systems can also provide instant printouts of the predicted changes (see Chapter 22).
Diagnostic wax-up / polyurethane clinical mock-up
Armamentarium
Clinical technique
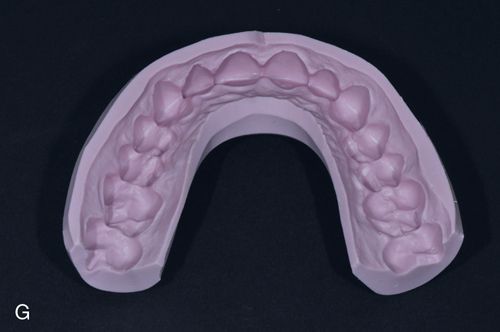
1. The dental laboratory technician fabricates a diagnostic wax-up to simulating the proposed final porcelain laminate veneer restorations (Fig. 7-1 F).
2. Adjust the diagnostic wax-up if necessary until it is acceptable to the clinician and the patient.
3. Make a trayless PVS impression of the diagnostic wax-up using laboratory putty (Fig. 7-1 G). This will be used as a matrix when fabricating a polyurethane intraoral mock-up of the proposed restoration.
4. Scallop the buccal areas of the matrix with the Bard-Parker knife (Fig. 7-1 H).
5. Select the appropriate shade of polyurethane provisional restoration material and place an appropriate amount into the matrix (Fig. 7-1 I).
6. Seat the matrix intraorally and allow the polyurethane material to polymerize (Fig. 7-1 J). Remove the matrix.
7. Finish and polish the mock-up until it is acceptable to the clinician and the patient (Fig. 7-1 K).
Patient education
Photography.
One of the most effective patient education tools is a book or photograph album containing before and after images of representative cases. These educational materials can be purchased commercially or be produced by the dentist (see also Chapter 22).
Demonstration porcelain laminate veneers.
Sample porcelain laminate veneers fabricated to fit on prepared denture teeth or stone casts are valuable patient education aids. They effectively demonstrate the conservative nature of this technique and the lifelike appearance of the definitive restorations.
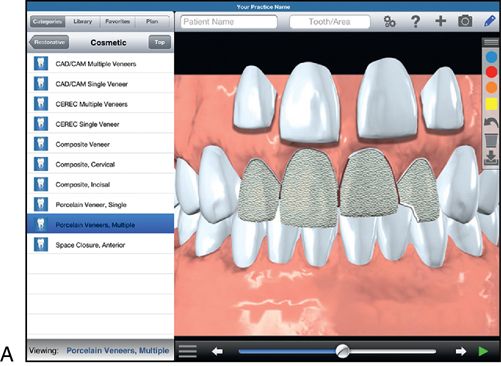
Tablet software.
Computer tablet demonstration software or computer demonstration software is another patient education modality (for example, DDS GP for the iPad, Kick Your Apps, [Fig. 7- 2 A] and Guru Patient Communication Suite for the PC, Reality Engineering LLC, Reno [Fig. 7-2 B]).

Tooth preparation
The outline form of the porcelain laminate veneer tooth preparation depends largely on the degree of desired color alteration. This consideration particularly influences the location of the interproximal and gingival finish lines.
Static area of visibility versus dynamic area of visibility
The entire facial tooth surface, including the gingival area and the area immediately facial to the contact area with the adjacent tooth (the facial embrasure), is visible if the available light and the perspective of the viewer are optimal. This static area of visibility occurs when the patient is seated in the dental chair under adequate lighting and with the lips fully retracted. The static area of visibility significantly differs from the actual dynamic area of visibility exhibited during normal function.
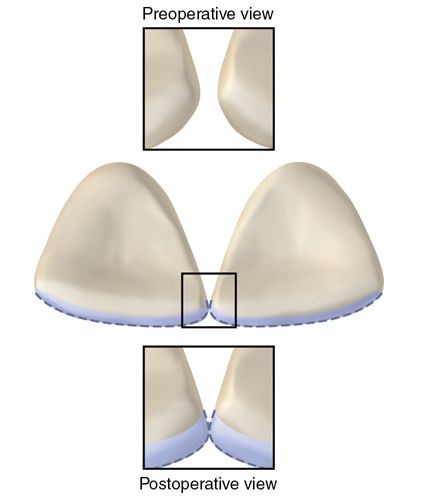
The dynamic area of visibility of the facial embrasure is partially a function of viewing perspective. It is particularly influenced, however, by shadows cast from surrounding structures. The lip, adjacent tooth contour and position, and gingival architecture, as well as the contour, shade, and position of the tooth under observation are all important factors (Fig. 7-3).
The dynamic area of visibility of the gingival area is governed by the position of the lip during maximal smiling (the high smile line).
Minimal or no color change
Proximal finishing lines.
A proximal chamfer finishing line is preferred except when diastemata are present. Proximal areas adjacent to diastemata should receive a feather-edged finishing line (Fig. 7-4).
Proximal contact area.
When the shade difference between the tooth (after preparation) and the desired definitive restoration is minimal, proximal chamfer finish lines are placed slightly facial (approximately 0.2 mm) to the contact areas of the adjacent tooth. This provides for the following:
1. Ease in evaluating marginal fit during the try-in stage
2. Access for performing and evaluating finishing procedures
3. Access for home care (margins in “self-cleansing” area)
4. Ease in evaluating marginal integrity during follow-up maintenance visits
The major disadvantage of this design is the possibility of eventual staining at the tooth-restoration interface. However, the factors influencing the dynamic area of visibility often negate this disadvantage. (See the section on static versus dynamic area of visibility in this chapter.)
Proximal subcontact area.
The proximal subcontact area (PSCA) consists of the interproximal tooth structure, which is immediately gingival to the contact area with the adjacent tooth. This area is usually not visible from a direct frontal view of the tooth (Fig. 7-5 A) and is therefore often left underprepared or totally unprepared. It is visible, however, from an oblique view. Therefore preparation of the PSCA is essential22 and is particularly crucial when the definitive restoration significantly differs in shade from that of the unprepared tooth structure and to avoid esthetic display of the restoration margins, which may eventually stain (see Fig. 7-5).


Diastemata.
The proximal area adjacent to a diastema should receive a feather-edged finishing line (see Fig. 7-4). This finishing line extends from the incisal edge to a point adjacent to the height of the gingival papilla.
Gingival finishing lines.
A chamfer is preferred for all gingival finishing lines. Supragingival finishing lines provide the same advantages as proximal finishing lines, which terminate facial to the contact areas. In addition, impressions are easier to make with supragingival preparations as compared with subgingival preparations. Supragingival finishing lines also increase the likelihood that restoration margins will end on enamel. The major disadvantage, however, is that any subsequent staining or color changes at the restoration margin will be visible. Therefore supragingival margins are limited to clinical situations in which this area remains concealed by the lip during maximum smiling (high smile line).
When the entire clinical crown is included in the facial display, the gingival margin should be placed 0.1 mm below the free gingival margin. If gingival recession is anticipated, the gingival finishing line can be extended deeper subgingivally as long as the biologic width is not violated.
Incisal preparation.
Incisal reduction should ideally provide for 1 mm of porcelain thickness. Therefore if the incisogingival height of the definitive restoration is to be 0.5 mm longer than the existing tooth, only 0.5 mm of incisal reduction is required. If the preoperative teeth are to be lengthened by 1 mm, only a rounding of the incisal edge and placement of a finishing line are required.
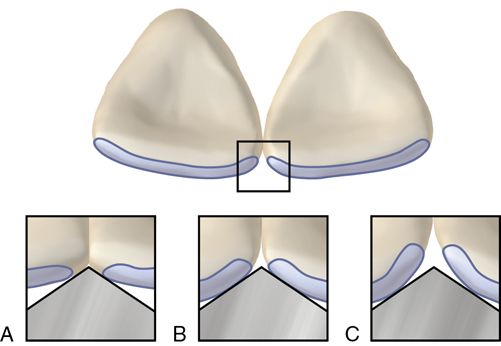
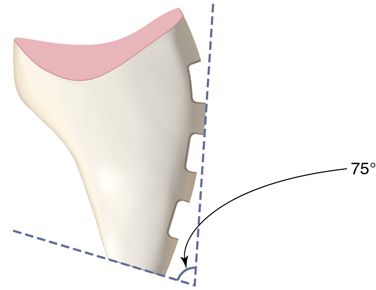
A butt joint finishing line provides for the proper thickness of porcelain at the margin to prevent restoration fracture. The finishing line should slope slightly gingivally (approximately 75 degrees from the facial). This augments resistance to facial displacement of the definitive restoration (Fig. 7-6).
After ideal preparation, the incisal outline of the tooth, when viewed from the facial aspect, should be identical to the incisal outline of the proposed definitive restoration, except for a 1-mm incisal reduction. This allows for an even thickness of porcelain. Incisal line angles must be rounded to reduce internal restoration stresses.
Facial depth reduction.
A facial reduction of approximately 0.5 to 0.7 mm is sufficient for most maxillary teeth and 0.3 mm for smaller teeth, such as mandibular incisors, if adequate thickness of enamel is present. Inadequate thickness of enamel, such as in the gingival one third of the tooth, may require a more conservative tooth reduction. Teeth or portions of rotated tooth surfaces that are in lingual version require proportionately less reduction. Preparation into dentin is sometimes necessary; however, this should involve less than 50% retention of the prepared surface.16
The entire finishing line should ideally remain in enamel.
Major color change
In addition to considerations of preparation design for minimal color changes, major color differences between the prepared tooth and the desired definitive restoration may also require other adjustments. Visibility of the contact area may necessitate extension of the interproximal finishing line into the contact area to a depth of approximately one-half the labiolingual dimension of the contact area. (See the sections on minimal or no color change and static versus dynamic area of visibility in this chapter.) The gingival finishing line can be extended 1 mm subgingivally, assuming the biologic width is not violated. Supragingival margins are indicated, however, if this area remains concealed by the lip during maximal smiling (high smile line). (See Clinical Tip in the section on gingival finishing lines.) The preparation depth may be increased if sufficient thickness of enamel is present. This will allow for an increased thickness of porcelain.
Armamentarium
• Lip retractor (e.g., One-piece Self-Span, Ellman International, Inc. Manufacturing Co.; Expandex, Parkell, Inc. or Lip Expanders, Denmat, Inc.)
• High-speed (friction grip) diamond three-tiered depth cutting burs (e.g., LVS-1 [0.3 mm depth cut] and LVS-2 [0.5 mm depth cut], Brasseler USA)
• High-speed (friction grip) two-grit burs (LVS-3, LVS-4, Brasseler USA)
• High-speed (friction grip) diamond wheel bur (e.g., 5909, Brasseler USA
• Unwaxed regular dental floss
• Retraction cord packer (e.g., Fischer’s Ultrapak Packer, Ultradent Products, Inc.)
• Nonimpregnated gingival retraction cord (e.g., Ultrapak No. 0 or No. 1, Ultradent Products, Inc.; Gingibraid No. 0 or No. 1, Van R Dental Products, Inc.)
• Gingival retraction instrument (e.g., Zekrya Gingival Protector, DMG America, Inc.) (optional)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


