

High strength ceramic cores require less tooth reduction than PFMs, which require a minimum of 1.5 to 2.0 mm of axial reduction. This reduction is necessary to create space for layers of opaque and veneering porcelains over an opaque metal core. Lithium disilicate and leucite-reinforced ceramic cores possess superior strength.3–6 Alumina and zirconia cores possess superior strength as well but do not have the translucent characteristics of lithium disilicate.
The cost of high noble metals such as gold has increased dramatically in recent years. Without the costs associated with precious metal, the all-ceramic crown can be less costly.
IPS e.Max
IPS e.Max (Ivoclar Vivadent) is an all-ceramic system consisting of five different components:
• e.Max Press (lithium disilicate glass-ceramic ingot for the “press” technique)
• e.Max Zirpress (fluorapatite glass-ceramic ingot for the press technique)
• e.Max CAD (lithium disilicate glass-ceramic block for the CAD/CAM technique)
• e.Max Zir CAD (zirconium oxide block for the CAD/CAM technique)
IPS e.Max CAD is a lithium disilicate glass-ceramic for CAD-CAM applications. The ingots are produced using sophisticated glass technology, which prevents the formation of defects in the ingots. Because the ingots are only partially crystallized, the blocks are easily machined. The ingots at this point are in their blue, translucent state. The partial crystallization process leads to the formation of lithium metasilicate crystals, which are responsible for the material’s relatively high strength and marginal integrity.
Following milling, the restorations are tempered and thus reach a fully crystallized state. At this point the lithium disilicate crystals are formed. Although improvements have been made in all categories, the most notable is in the material strength wherein 360 MPa has been achieved, allowing a number of restorative possibilities. Achievable fit is excellent when properly fabricated.7 If the core is cut back after pressing or waxed and pressed to less than full contour, porcelains may be baked in layers to achieve depth of color in the definitive restoration (“layering technique”). In addition to full coverage restorations, e.Max is particularly well suited for posterior inlays, onlays, and anteriorly for porcelain veneers.5 A simple acid etching (using 5% hydrofluoric acid) of all the internal aspects of the restoration during bonding or “luting” procedures enhances retention (Fig. 8-2 A).







Following the complete removal of all preexisting alloy and excavation of any caries present, the teeth are isolated and the internal surfaces are etched with 10% phosphoric acid for 15 to 30 seconds, rinsed well, and lightly air dried. This is followed by application of Gluma desensitizing liquid (Heraeus Kulzer Inc.) using a microbrush or equivalent, to all exposed dentin surfaces.
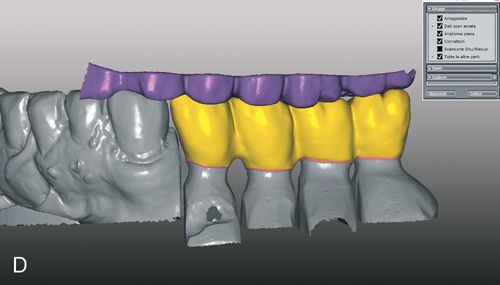
Next, radiopaque light-polymerized reinforced glass ionomer (Fuji II LC, GC America, Inc.) is mixed, powder/liquid, then syringed using a needle syringe (AccuDose, Centrix, Inc.) into the cavity preparation to create a base and fill any undercuts. It is immediately light polymerized and prepared to create ideal preparation designs (Fig. 8-2 B). The impression is made and poured in stone or scanned intra-orally and reproduced digitally to reproduce the clinical situation (Fig. 8-2 C). Alternatively, the stone cast may be scanned and the digital information used to manufacture the restorations using CAD-CAM technology, milling from a block.
Waxing, spruing, pressing, divesting, fitting, and margin refinement are all done utilizing the sectioned stone cast where dies are removable and may be inspected and handled individually (see Fig. 8-2 C). The second, solid, uncut cast is used to verify interproximal contacts in the laboratory (Fig. 8-2 D).
At the restoration delivery appointment, provisional restitutions are removed and the cavity preparations are thoroughly cleaned with Tubulicid (Dental Therapeutics AB) using a microbrush or equivalent. This chemical removes the superficial smear layer without opening tubules, while cleaning and distributing fluoride simultaneously. Next, the restorations are tried in individually and adjusted where necessary for complete seating (see the section on Crown Try-in and Placement later in this chapter). Once all the restorations have been tried in together and are ready to be placed permanently, they are internally acid etched with IPS ceramic etching gel (5% Hydrofluoric acid) for 20 seconds, rinsed, and air dried. As a recommendation, these internal surfaces should be “conditioned” using Monobond Plus (silanization) for 60 seconds then air dried. Next, the internal surfaces of the teeth including enamel are etched with 10% phosphoric acid for 15 to 30 seconds, rinsed well, and lightly air dried. Immediately apply Gluma desensitizing liquid on dentin surfaces using a microbrush. Studies have shown that Gluma that touches enamel surfaces will have no effect on the bond strength of the restorations to the tooth.7 One-Step universal light-polymerized dental adhesive (Bisco, Inc.) is then applied with a microbrush to all internal surfaces to be bonded (enamel, dentin, and base) and is light-polymerized for 60 seconds.
Dual luting composite resin cement or Variolink (Ivoclar Vivadent) are well-suited luting agents for these types of restorations. The luting cement is best filled into a needle syringe (ex., AccuDose) and delivered into the isolated cavity preparation. The restoration is then placed and fully seated using a metal-pointed instrument pressing into the central fossa to ensure complete seating. A plastic disposable bristle brush (Bendabrush, Centrix, Inc.) may be used to wipe away excess cement and while still applying seating pressure, floss should be passed between teeth to clear the interproximal excess before light curing.
Once all the restorations have been luted into place and excess cement has been cleared, final occlusal refinements need to be made. For this, use two-color, double-sided articulating paper Accufilm II (Parkell, Inc.) and 7-micron–thick metal foil (Almore International Inc.), football-shaped diamond burs, (e.g., Fine 8369DF-31-025, and Extrafine 369DEF-31-025 [Brassler USA]) and rubber wheels (Dialite LD adjustment, finishing, and polishing kit [Brassler USA]) all designed specifically for use with lithium disilicate. See the section on Occlusal Adjustments later in this chapter (Figs. 8-2 F and G).
Porcelain laminate veneers
In addition to inlays and onlays, e.Max can be used for porcelain laminate veneers (Fig. 8-3). e.Max is available in a variety of ingot choices ranging from translucent to opaque (HT, LT, MO, and HO). Due to the material’s somewhat low-value quality, depth of color and translucency can be achieved giving lifelike results. The more opaque ingots can block unwanted substrate color, for example, gold posts or dark, discolored dentin, typically seen in endodontically treated teeth. The degree to which these dark substrate colors may be blocked may be a function of the skill of the dental ceramist when compared with what might be achieved with more conventional metal-ceramic systems.





Besides e.Max there are a number of other restorative material options, which possess a high-strength ceramic core and are available as either a monolithic or a layered technique. These include LAVA (3M ESPE), Cercon (Dentsply Ceramco) and Procera (Nobel Biocare).
Zirconia
An all-ceramic system known as Procera AllCeram (Nobel Biocare) has been available since 1993.8–15 Unique to this method is the use of computer-assisted design and computer-assisted manufacturing (CAD/CAM) to fabricate a densely sintered, high-purity aluminum oxide coping, which is later veneered with porcelain. A scanner “reads” the stone die into a specialized unit that processes the data and creates either a two-dimensional cross-section or a three-dimensional view on a computer monitor. The shape of the crown (e.g., an emergence profile angle) may be selected and modified before actual coping fabrication (CAD). The production unit (originally in Sweden but now milling centers are available throughout the world), receives this information via modem and the coping is fabricated and mailed to the dentist without the need for any stonework leaving the dentist’s office (see Chapter 23).
The primary advantage in this methodology is the ability to ensure quality control in the coping manufacturing process using industrial standards, which eliminates the many operator variables possible in coping fabrication. The marginal preparation design may be more chamfer-like than a true shoulder because of the increased strength of this sintered understructure. Sharp internal line angles and stress points are undesirable because they create internal stress in the coping. The zirconia coping or understructure has proved to be very strong but the feldspathic porcelains layered on the coping have been less than fully reliable.16 Delamination or chipping is common (Figure 8- 4 A)









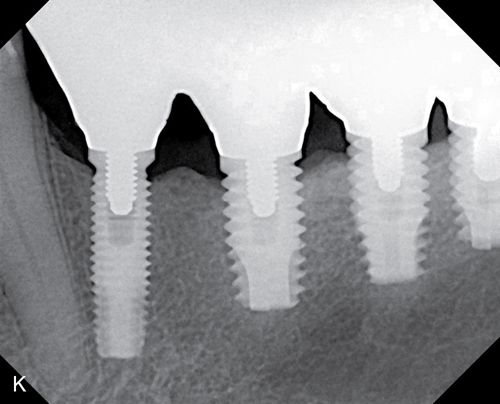
Originally, coping design was implicated as the primary reason for delamination. Greater attention given to porcelain support improved but did not eliminate the problem. More recently, use of zirconia in monolithic designs has been gaining popularity. The milling of blocks produces a full contour restoration, which is colored by new techniques developed for this purpose.16 New techniques in copy milling have enabled technicians to reproduce patterns for multiple unit frameworks and implant frameworks or complete monolithic designs (Figs. 8-4 B– K).17 It is expected that this monolithic restoration simply will not chip or break in any way.
Continued research and study in the use of zirconia has led to new technology and techniques, bringing us closer and closer to esthetics we have come to expect with more conventional feldspathic materials. A major advantage with this material is its virtually indestructible strength.
Light absorption and refraction
The metal component of PFM restorations prevents the transmission of light. Even diffusion of light through the porcelain is diminished when metal is present beneath the veneering porcelain.18, 19 The marginal soft tissues adjacent to subgingivally placed metal collars often appear dark, especially if the gingival tissues are thin. This effect may occur in PFM restorations with facial butt joint designs, because the small amount of porcelain covering the metal is opaque and creates a shadow of the root surface by blocking the normal transmission of light through the facial gingival tissues (Fig. 8-5 A and B).


All-ceramic crowns and natural teeth allow the transmission of light to occur because of the absence of a metal coping. The ability to allow light to pass through itself varies with different materials. For example, feldspathic porcelains characteristically refract light differently than cast glass or pressed ceramics and natural enamel. The unorganized, random crystalline form of porcelain refracts approximately 25% of the available light and opacifying porcelain refracts even less. e.Max refracts as much as 75% of entering light, because its organized crystalline form has a refractive index similar to that of enamel.20 Zirconia restorations do not possess the same optical qualities as lithium disilicate. Researchers have concluded that light transmission is significantly diminished in zirconia restorations.21, 22 LAVA restorations (3M ESPE) are the most translucent of the zirconia restorations at 0.3-mm and 0.5-mm core thicknesses. Studies 23 have also demonstrated that the thickness of the zirconia core directly affects translucency. Therefore monolithic zirconia restorations are opaque and, as such, are usually less desirable for use in the esthetic zone.
Biocompatibility
Rough, uneven, porous surfaces tend to encourage bacterial colonization. Poor margin adaptation or design, improperly glazed porcelains, and rough acrylics contribute to gingival inflammation.24 Clinically, superb gingival response and esthetics routinely occurs when margins are placed well above attachment levels and, as such, do not invade or infringe upon the biologic width. Biofilm formation differs significantly among restorative materials.25, 26 Polished zirconia exhibits sharply reduced plaque accumulation compared with metal-ceramics, making it ideal for subgingival margin placement.27
Control of margin placement
The gingival extent of the interproximal shoulder of a full crown restoration may be deeper than ideal because of caries or a preexisting deep restoration. Deep subgingival margins complicate retraction, impression techniques, and margin evaluation. Biologic width violation and compromised oral hygiene access can result in gingival inflammation, pocket formation, and other periodontal problems.28–31 If the preparation has ideal substrate color, it is usually not necessary to place the preparation into the gingival sulcus. An exception to this occurs when a restoration is used to correct a diastema. A subgingival margin allows for a more gradual increase in restoration interproximal emergence contour by avoiding an abrupt transition of tooth to restorative material. In addition, especially when using lithium disilicate or another translucent core, and assuming ideal tooth substrate color, the margin placement can be supragingival, thus avoiding any physical challenge to biologic width.32, 33
Ideal preparation requirements
Preparations for single tooth restorations have evolved primarily with the goal of creating excellent natural esthetics. Retention is aided by parallel axial wall design, dentin bonding techniques, and acid etching the internal portion of the restoration if possible34 Restorations made of zirconia, are currently not internally etchable. The finishing line can be 90 degrees to the external unprepared axial root surface, with rounded internal line angles. Thin margins or beveled preparations are contraindicated because they would create an unacceptably weak ceramic margin.
Perhaps the most difficult aspect of the butt joint preparation design is the shoulder or actual butt joint. When viewed from the occlusal, adequate reduction is important to guard against breakage during function, because classically, thin areas tend to chip as the tooth flexes. A 360-degree chamfer with a minimum depth of 1 mm is recommended; however, 1.5 mm is ideal, because the restoration will be thicker and therefore stronger. More research is needed to determine the ideal preparation depth, because the increased strength of the materials suggest that less tooth reduction and thinner restoration wall thickness may be acceptable. In addition, greater thickness always provides the ceramist with a better opportunity to achieve more lifelike esthetics and affords greater ability to block underlying unfavorable substrate color. However, greater material thickness achieved by more reduction than recommended (over preparation) may lead to pulpal involvement and can weaken the tooth.
Technique
Armamentarium
• “Great White” #2 carbide for prior crown removal (S.S. White Technologies Inc.)
• Chamfer, round end taper, 5856L-31-018 (Brasseler USA)
• Modified chamfer, 5878K-31-018 (Brasseler USA)
• Cingulum reduction bur, football, 6379-31-023 (Brasseler USA)
• Incisal reduction bur, #35010-31-5 and 30006-106 (Brasseler USA)
• Occlusal reduction bur, 30010-018424U0 or 36006-011817U0 (Brasseler USA)
• White polishing points, 649-31-420 (Brasseler USA)
• Protection/visualization cord, No. 000 Ultrapak, black, nonimpregnated (Ultradent Products, Inc.)
• Deflection/retraction cord, No. 1 Ultrapak, blue, nonimpregnated, (Ultradent Products, Inc.)
Clinical technique
Anterior preparation (Fig. 8-6)
1. Place protection cord; see the section on Impressioning in this chapter. This may need to follow interproximal axial reduction first in order to break the interproximal contact and allow easy cord placement.
2. Reduce the tooth a minimum of 1.0 mm facially and axially. (Note: Reduction of more than 2.0 mm is considered overreduction and can substantially weaken the integrity of the remaining tooth structure, possibly leading to fracture of the abutment. Additionally, pulpal involvement and sensitivity become potential problems.)
3. Reduce the tooth 1.5 to 2.0 mm incisally if sufficient tooth structure exits.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


