Experience with arthroscopy of the temporomandibular joint (TMJ) and with endoscopic sinus and skull base surgery equips the oral and maxillofacial surgeon for the endoscopic-assisted treatment of maxillofacial trauma. Endoscopic-assisted management of maxillofacial trauma has been described for treatment of fractures of the mandibular condyle, the zygomatic complex, the orbit, and the frontal sinus. The reduction and fixation strategy of open fracture treatment with osteosynthesis has not changed. However, with the use of endoscopic-assisted techniques, extraoral incisions can be limited or avoided in favor of intraoral approaches. Intraoperative fixation after fracture reduction in areas of limited exposure and visibility can be obtained with these techniques. However, the choice to use endoscopic techniques has no influence on the indication for surgical treatment. It is a relatively new surgical field, which continues to expand, yet its long-term benefit in many scenarios, still awaits confirmation.
State-of-the-Art Management
Mandible
Mandibular Condyle Fractures
Fractures of the mandibular condyle are common and account for 9% to 45% of all mandibular fractures. Closed reduction is the method most widely employed for the treatment of displaced condylar fractures. Anatomical reduction is rarely achieved, and rehabilitation and TMJ function depend on adaptation of the altered condylar morphology or formation of a new joint. With precise fracture reduction by preauricular, retromandibular/transparotid, or submandibular approaches, damage to the facial nerve and the creation of visible scars have been described. Because of these possible complications, the indications for open reduction versus closed treatment are still in debate.
The risks of facial nerve damage and extensive visible scars can be minimized by minimally invasive endoscopic techniques using a transoral approach. However, in cases of severely displaced or comminuted fractures, the extraoral approach seems to be advantageous over endoscopic-assisted reduction of mandibular condyle fractures.
Other Mandibular Fractures
For mandibular fractures in other locations, such as the mandibular angle and the ramus, the transoral approach is less time-consuming and is preferable to avoid visible scars and possible facial nerve damage. The transoral approach is indicated if there is no comminution. However, with a transoral approach, the inferior and posterior aspects of the fracture and possible lingual gaps cannot be visualized. Endoscopic examination of the fracture site after transoral reduction and fixation of fractures provides further information about the accuracy of the fracture reduction. The alignment of the posterior and inferior aspects of angle fractures and the presence of a lingual gap in ramus fractures can be detected endoscopically and corrected intraoperatively if necessary.
Midfacial and Frontal Sinus Fractures
Endoscopic-assisted techniques for treatment of fractures of the zygoma, the midface, and the orbit have been reported. In patients with fractures of the zygomatic complex, the orbital floor and infraorbital rim are often inspected by transconjunctival or mid–lower eyelid incisions. Nondisplaced fractures of the orbital floor that do not need to be treated yet are often noted. Inadequate results after repositioning may occur due to rotation of the fragment if the repositioning at the sphenozygomatic buttress is not fixed.
Inspection of the lateral orbital wall in cases of displaced fractures of the zygomatic complex can be performed endoscopically by means of a limited blepharoplasty incision. In zygoma fractures, the orbital floor can be endoscopically inspected transorally via the maxillary sinus. The result after fracture reduction can also be evaluated at the infraorbital rim and the lateral orbital wall. Additional transconjunctival or infraorbital incisions can be avoided if there is no displaced fracture of the orbital floor and no displacement of the fragments at the infraorbital rim after repositioning. When indicated, osteosynthesis of the infraorbital rim can be performed endoscopically by the transoral approach.
The endoscopic treatment of comminuted fractures of the zygomatic arch is reported to avoid open reduction via coronal incisions, in the rare cases when an open approach is needed.
Frontal sinus fractures of the anterior wall may be reduced with the use of minimally invasive techniques. At least two incisions posterior to the hairline are needed for insertion of the endoscope and instruments for repositioning of fractures. Stab incisions may be needed for direct manipulation and fixation of the fragments. The indications for minimally invasive endoscopic surgery of the frontal sinus may be limited to single-fragment fractures of the anterior table of the frontal sinus.
Surgical Technique
Endoscopic Equipment
The results of our experience are presented below, as this is rapidly developing field of surgery, clear clinical outcomes are not yet available for many procedures.
Initially, a prototype of an endoscopic plate application device (Synthes, Paoli, Penn) with a 30-degree angle, 4-mm diameter endoscope (Karl Storz, Tuttlingen, Germany) was used via an extraoral approach, because of the limited vision with this angulation during plate insertion using the plate application device there was a need for transbuccal incisions.The device was successfully only used in selected cases if the submandibular approach was performed.
In selected cases, 45- and 70-degree angle endoscopes, when used by experienced endoscopic surgeons, can be successful. These endoscopes are more difficult to employ, because there is limited forward vision when inserting the endoscope. A suction and irrigation device allows irrigation of the endoscope tip in limited optical cavities if vision through the lens is blurred by blood.
The monitor and the endoscopic equipment should be placed in the operating room facing the surgeon and assistant. Intraoperatively, it is important to watch the endoscopic picture on the monitor while sitting in a comfortable position. The light source and the camera should be close to the patient’s head to avoid limiting the movement of the endoscope. A second suction device is recommended, even if an endoscope equipped with a suction and irrigation instrument is used.
Mandibular Condyle Fractures
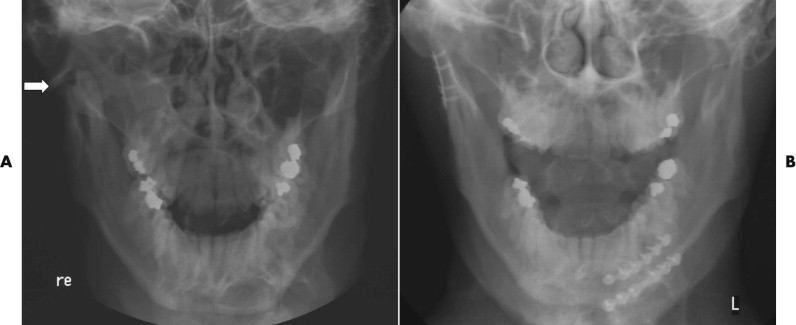
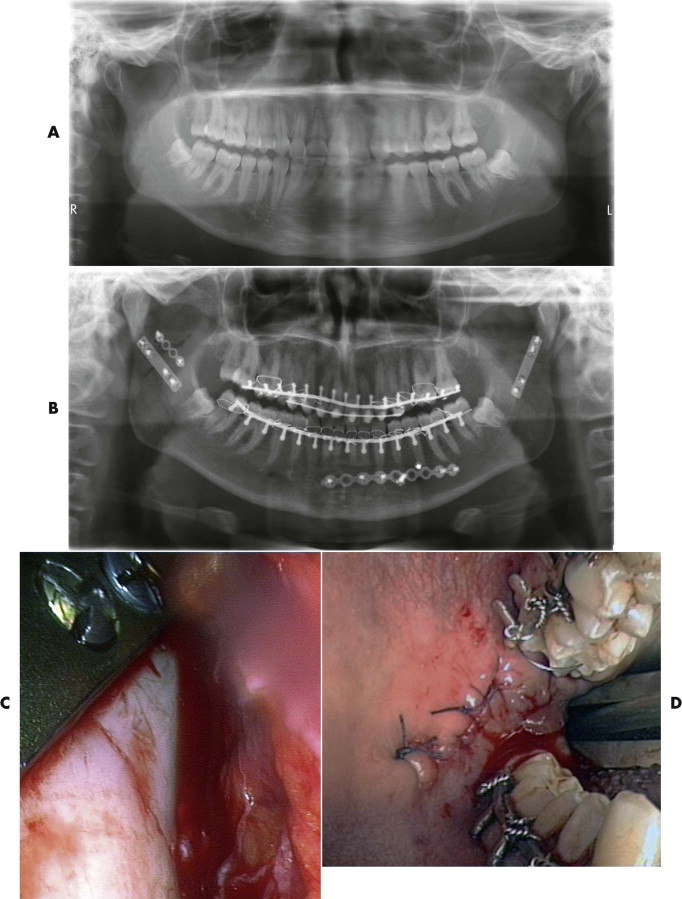
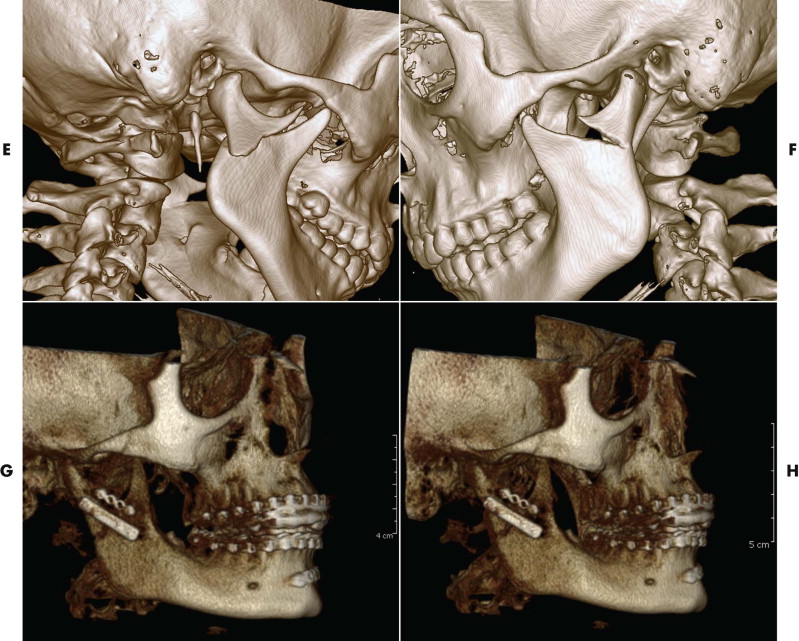
The type of fracture, degree of displacement, and result of reduction were evaluated intraoperatively using the endoscope. Of course, conventional preoperatively and postoperatively Towne’s and panoramic radiographs or computed tomographic (CT) and conebeam computed tomographic (CBCT) scanning are required ( Figs. 31-1 to 31-3 ).
Transoral Approach
The transoral incision is similar to the surgical approach for sagittal split osteotomies of the mandible in orthognathic surgery. Local anesthetic is injected 8 to 10 minutes before incision to control bleeding. To create the optical cavity, the periosteal tissue on the ascending mandibular ramus is elevated, freeing the posterior aspect of the ascending ramus and the mandibular angle. The inferior inserting fibers of the temporalis muscle are stripped from the lower aspect of the muscular process. The endoscope is inserted subperiosteally and advanced cranially toward the fracture without dissection of the masseter muscle to avoid bleeding and damage to the facial nerve (see Fig. 31-7 ).
Repositioning and Fixation
Distraction of the TMJ region by pressure on the mandibular molars via the transoral approach is performed to facilitate repositioning of the condylar fragment. The periosteum and the soft tissues in the vicinity of the proximal fragment are removed carefully to allow the miniplates to be placed without detaching the lateral pterygoid muscle or impairing the blood supply to the condylar head.
Special instruments are inserted for the reduction of the condylar fragment. Stab incisions in the condylar region are made for transbuccal insertion of the screws. Transbuccal incisions are avoided when angulated drills and screw drivers are used endoscopically via a transoral approach (see Fig. 31-2 ).
After insertion of the first screw in the condylar fragment, the fracture reduction is facilitated by pulling the miniplate with modified nerve hooks. The second screw is then inserted next to the fracture in the mandibular fragment. Osteosynthesis is performed with a 2.0-mm miniplate with at least two screws on each side of the fracture. After fracture reduction and fixation using two screws, the alignment at the posterior border of the ascending ramus is controlled endoscopically before osteosynthesis is completed (see Figs. 31-3 and 31-8 ).
Mandibular Fractures in Other Locations
In patients with mandibular fractures, endoscopic-assisted control after transoral fracture reduction is performed in areas of limited vision such as the inferior and posterior aspects of the ascending ramus in mandibular angle fractures ( Table 31-1 ). The result after fracture reduction was controlled endoscopically in areas of limited visibility during the transoral approach to avoid displacement at the inferior and posterior aspect of the fracture and prevent lingual gaps before osteosynthesis is completed.
| Indication | No. of Patients |
|---|---|
| Condylar fractures | 45 |
| Investigation and treatment of midface fractures with additional orbital injury (e.g., orbital floor) | 49 |
| Decompression of optic nerve | 3 |
| Fixation of distraction devices in the mandible | 2 |
| Treatment of mandibular fractures or plate removals | 21 |
| Revisions of frontal sinus | 7 |
| Other (e.g., exploration of skull base; treatment of lesions in combination with conventional surgical procedures) | 14 |
Midfacial and Frontal Sinus Fractures
In patients with fractures of the zygomatic complex and the orbit, endoscopic-assisted treatment can be undertaken. Limited incisions were performed, and because of the superior visibility with endoscopic techniques, further incisions (e.g., a transconjunctival approach) could be avoided in selected cases. However, the advantage of endoscopic-assisted techniques in the treatment of midfacial trauma remains controversial.
Zygomatic Fractures
Because of possible rotation of the zygomatic bone, the result after repositioning can be evaluated intraoperatively before osteosynthesis is performed. The repositioning cannot be determined precisely from the lateral orbital wall with an intraoral approach. An additional extraoral approach for exploration of the orbital floor and the infraorbital rim is recommended if displaced zygoma fractures are suspected. Using these additional incisions, one can often identify nondisplaced fractures that do not need treatment at the orbital floor and infraorbital rim.
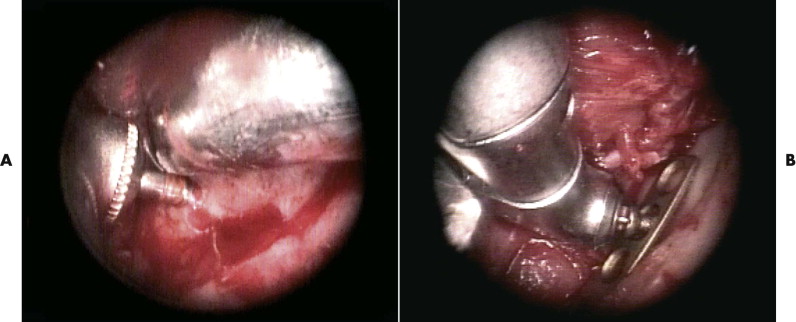
In case of zygoma fractures, the endoscope is inserted via a limited blepharoplasty incision to control the fracture-dislocation at the sphenozygomatic buttress at the lateral orbital wall ( Figs. 31-4 and 31-5 ). In displaced zygoma fractures, defects of the outer wall of the maxillary sinus often exist and can be used to insert the endoscope for transoral inspection of the orbital floor ( Fig. 31-6
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


