The eyelids protect the eyes. Spontaneous blinking sweeps away microscopic debris and moistens the eyes with tears. A dust fragment or bright light stimulates reflex blinking, and during sleep, the eyes are protected by continuous eyelid closure. Without adequate eyelids, the combined effects of desiccation and repeated minor trauma would soon lead to painful blindness. Neglected eyelid trauma can have the same disastrous result.
The distress that inevitably accompanies facial trauma can be reduced considerably by a cosmetic and functional outcome that restores normality as far as possible, especially to the midface. This is achieved by careful assessment in the hours after trauma and appropriate early management with later adjustment if necessary. A multidisciplinary approach is appropriate for all but the most superficial injuries. Photographs add to the written record, aid in planning late adjustments, and provide an accurate graphical record for medicolegal purposes.
Anatomy
Thorough knowledge of the anatomy of the periorbital region is essential for an accurate assessment and repair of eyelid and canthal trauma.
Surface Anatomy
The upper and lower lids enclose the palpebral aperture, and they join at the medial and lateral canthi ( Fig. 18-1 ). The average size of the palpebral aperture in an adult is 30 mm horizontally and 10 mm vertically between the centers of the lids. In the upper lid, the delicate preseptal skin (inferior to the brow) and the pretarsal skin (superior to the lashes) meet at the upper lid skin crease, 6 to 10 mm from the lash line in an adult and lower in a child. The skin crease in the upper lid is formed by the insertion of the levator aponeurosis into the orbicularis muscle at this level. There is often redundant skin superior to the skin crease in the upper lid so that a skin fold is created that covers the skin crease when the eye is open. Superior to the skin crease, the fullness in the upper lid is caused by orbital fat. A less obvious skin crease may be visible in the lower lid 4 to 5 mm from the lash line. Fullness in the lower lid also is caused by orbital fat. The lateral canthus lies at a slightly higher position than the medial canthus, and it rises further in upgaze.

Eyelid Structure
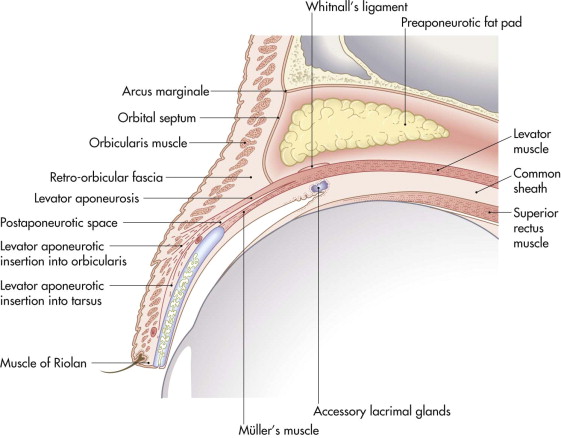
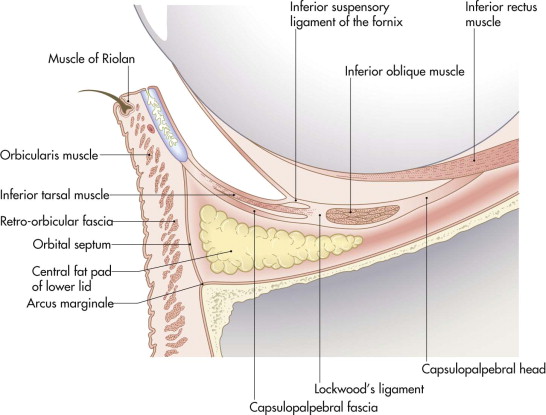
An eyelid is conveniently divided into two anatomical lamellae ( Figs. 18-2 and 18-3 ). The anterior lamella includes the skin and the orbicularis muscle. The posterior lamella is formed by the tarsal plate and the conjunctiva. Any reconstruction of the eyelid must restore the anterior covering lamella (skin) and the posterior lining lamella (mucosa) for the lid to function normally.
The skin of the eyelids is the thinnest in the body. It is attached loosely to the orbicularis muscle and more firmly attached in the region of the canthal tendons.
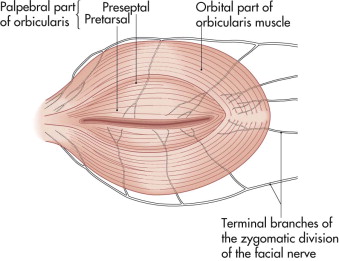
The orbicularis oculi muscle is the main protractor of the eyelids ( Fig. 18-4 ). It is a flat sheet of concentric fibers encircling the palpebral aperture and spreading out beyond the orbital rims. It is divided into concentric zones: palpebral and orbital. The palpebral part overlies the eyelids. It is subdivided into a pretarsal part overlying the tarsal plates and a preseptal part anterior to the orbital septum in the upper and lower lids. The orbital part of the orbicularis muscle lies peripheral to the palpebral part. Because the orbicularis muscle is supplied by the facial nerve, lacerations that damage the nerve may compromise eyelid closure.
The anatomy of the lymphatic drainage of the lids is important in facial trauma. Lacerations or surgical incisions that cut the lymphatic drainage may result in prolonged edema of the eyelid tissues. The lateral two thirds of the upper lid and the lateral one third of the lower lid drain to the preauricular and parotid lymph nodes. The medial one third of the upper lid and the medial two thirds of the lower lid drain to the submandibular nodes.
Lateral Canthal Tendon
The pretarsal muscles join laterally and insert by a common tendon into Whitnall’s tubercle, a bony prominence in the lateral orbital wall 5 mm posterior to the lateral orbital rim. The preseptal muscles join laterally to form a lateral raphe, which is connected to the underlying tendon. Deep to the muscle insertions, a Y -shaped fibrous thickening in the orbital septum joins the lateral ends of the tarsal plates to Whitnall’s tubercle. These structures together form the lateral canthal tendon.
Medial Canthal Tendon
The medial canthal tendon is complex anatomically, and some controversy surrounds the details of the anatomy. It has a fibrous and a muscular component. The muscular component is the insertions of the preseptal and pretarsal muscles ( Fig. 18-5 ). The fibrous component is attached laterally to the medial ends of the tarsal plates as two limbs of a Y . The stem of the Y inserts medially, and it has an anterior and posterior component. The anterior component inserts on the frontal process of the maxilla just anterior to the anterior lacrimal crest level with the upper part of the lacrimal sac. The posterior part leaves the deep surface of the anterior part just lateral to the anterior lacrimal crest. It passes medially and posteriorly, lateral to the lacrimal sac, and inserts on the posterior lacrimal crest. The muscle insertions are divided into superficial and deep heads, which also insert into the anterior and posterior lacrimal crests. Contraction of the preseptal orbicularis muscle during blinking activates the lacrimal pump mechanism, which facilitates the passage of tears from the palpebral aperture through the canaliculi into the lacrimal sac.
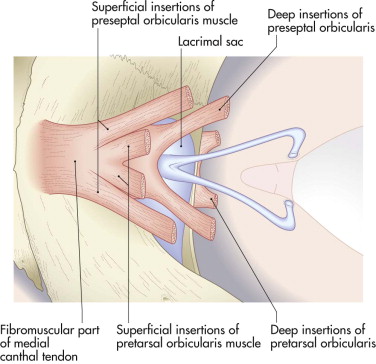
In practice, the detailed anatomy of the medial canthal tendon is not evident at surgery. The fibrous part is clearly visible, especially the anterior component. The posterior components of the medial canthal tendon are the main anchor for the medial ends of the lids. It is important to reconstruct the posterior component by reattaching the canthal tissues to the posterior lacrimal crest if it has been divided by medial canthal trauma.
Upper and Lower Lid Retractors
The levator palpebrae and Müller’s muscles working together maintain the normal position of the upper lid when the eye is open (see Fig. 18-2 ). The levator muscle arises from the roof of the orbit immediately anterior to the optic foramen. It passes forward above the superior rectus muscle to end just posterior to the orbital septum as an aponeurosis. The aponeurosis passes forward into the lid and is inserted into the orbicularis muscle at the level of the upper lid skin crease and into the lower one third of the anterior surface of the tarsal plate. The orbital septum inserts into the anterior surface of the aponeurosis soon after its origin from the levator muscle. The aponeurosis expands medially and laterally to insert into the region of the medial and lateral canthal tendons as the medial and lateral horns of the aponeurosis ( Fig. 18-6 ).
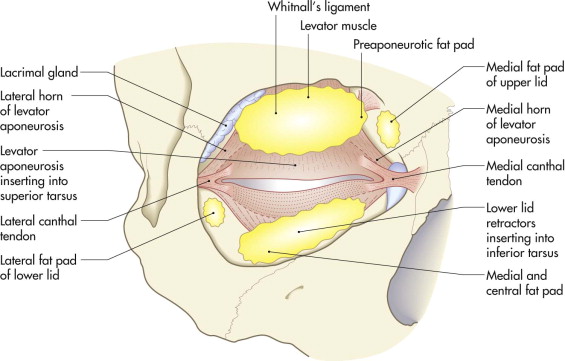
Müller’s muscle lies deep to the levator aponeurosis, between it and the conjunctiva. It arises from the deep surface of the levator muscle at the point of origin of the levator aponeurosis. It descends to insert into the superior border of the tarsal plate. The preaponeurotic fat pad lies posterior to the septum and superior to the levator muscle. This fat gives the upper lid its fullness, and it is an important surgical landmark.
The structure of the lower lid is similar. The lower lid retractors are vestigial but important in maintaining lower lid position. The central fat pad in the lower lid is similar anatomically to the preaponeurotic fat in the upper lid.
The Lacrimal System
Tears are produced by the lacrimal gland, which lies between the globe and the superior temporal quadrant of the anterior orbit, just within the orbital rim ( Fig. 18-7 ). As it becomes the lateral horn, the lateral edge of the levator aponeurosis creates a deep cleft in the lacrimal gland, dividing it into two lobes, a larger orbital lobe above the lateral horn and a smaller palpebral lobe below the lateral horn. The palpebral lobe is just visible in the lateral end of the superior conjunctival fornix if the lateral end of the upper lid is lifted. Fine secretory ductules pass from the palpebral lobe to penetrate the conjunctiva of the superior fornix laterally.
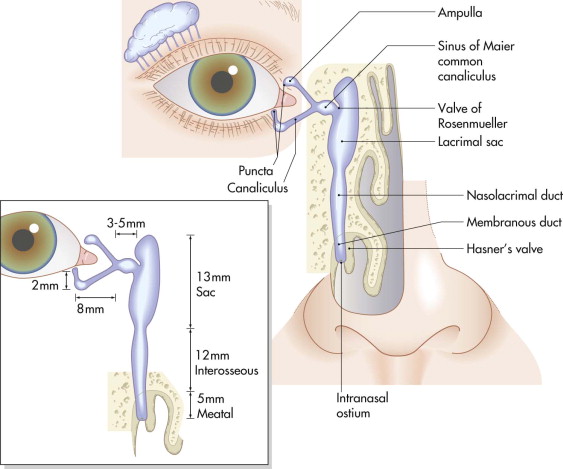
Blinking spreads tears across the cornea, and they usually move in a medial direction toward the lacrimal puncta in the upper and lower lids approximately 6 mm from the medial canthus. The puncta normally lie within the tear film, and eversion of the puncta hinders the collection of tears. Canaliculi pass from the puncta medially to the lacrimal sac. The initial 2 mm of each canaliculus passes vertically into the lid before turning medially. At the medial canthal angle, the canaliculi pass posterior to the anterior limb of the medial canthal tendon and usually join to form a common canaliculus 3 to 5 mm lateral to the lacrimal sac. The common canaliculus opens into the sac 2 to 3 mm behind the anterior limb of the medial canthal tendon. The lacrimal sac is situated within the fossa and is bounded by the anterior and posterior lacrimal crests. The sac empties inferiorly into the nasolacrimal duct that passes down through the bony nasolacrimal canal, which is about 12 mm long, to open into the lateral wall of the nose under the inferior turbinate, which is approximately 15 mm from its tip and 30 to 35 mm from the external nares.
Assessment
History
An accurate account of the cause of the trauma allows a preliminary estimate of the depth and extent of the injury. Blunt trauma frequently leads to diffuse contusion with irregular wound edges, whereas sharp objects cause wounds with smoother edges that are often deeper.
Examination
Tissue swelling or a reduced level of consciousness may prevent a full assessment. A stepwise approach to the examination of the periocular soft tissues is helpful.
Gross Pathology
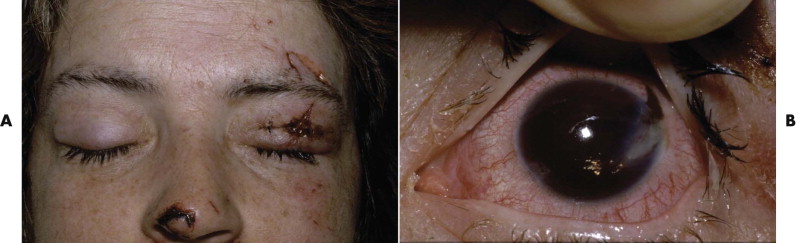
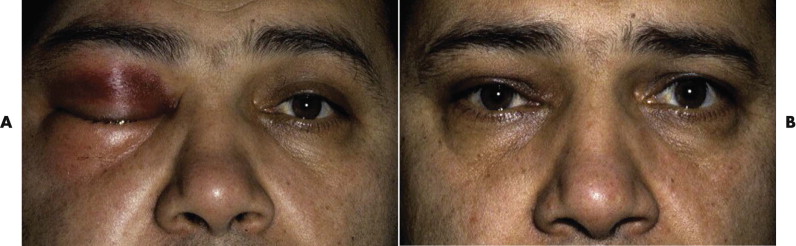
The examination assesses edema, ecchymosis, crepitus, and hematoma. It is important to differentiate an orbital hematoma from preseptal hemorrhage. An orbital hematoma has a sharply limited edge ( Fig. 18-8 ). The globe may be proptosed and eye movements reduced. In contrast, preseptal hemorrhage ( Fig. 18-9 ) may be extensive, causing considerable local swelling but without proptosis of the globe or limitation of eye movements. A subconjunctival hemorrhage arising from an orbital hemorrhage ( Fig. 18-10 ) has no posterior edge but disappears posteriorly around the equator of the globe. Subconjunctival hemorrhages due to direct trauma ( Fig. 18-11 ) may be localized with the whole edge visible, although the posterior edge is often well posterior and may not be visible.




Record entry wounds, estimate the depth of wounds, and document any possible loss of tissue. Record whether the lid margins are involved in any laceration. Notice lacerations involving the medial canthus, the presence of telecanthus, and aponeurosis or lacerations in the upper lid that may have damaged the levator muscle.
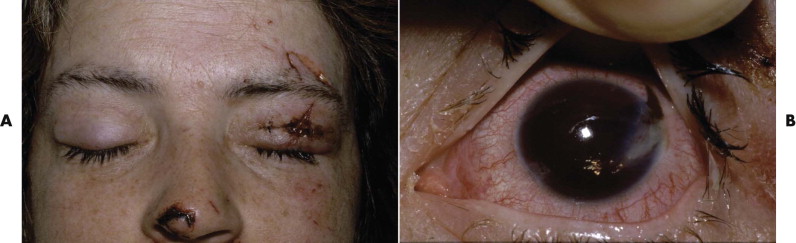
Exclude blunt or penetrating trauma to the eye, particularly penetrating injury of the globes if the eyelids are lacerated ( Fig. 18-12 ). Check the visual acuity. Examine the pupils for their size at rest and their reaction to light.
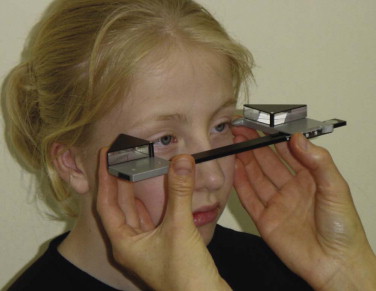
The swinging flashlight test ( Fig. 18-13 ) is valuable for identifying optic nerve trauma. To perform this test, dim the lights in the examination room, and if the patient is able to cooperate, indicate a distant target to look at. With a bright light, illuminate first one eye for 2 seconds and then the other for 2 seconds. Swing the light backward and forward in this fashion, and observe the pupil reactions. In the absence of optic nerve trauma (or disease) or widespread retinal trauma, the pupils remain small in both eyes, apart from momentary dilatation during the transit of the light from one eye to the other. In the presence of unilateral trauma to the optic nerve or with widespread retinal trauma, the pupil on that side dilates instead of remaining constricted as the light is moved from the normal eye to illuminate that eye. If the patient is mobile, a slit-lamp examination with measurement of the intraocular pressures is important at this stage.

Eyelid Position
The examination evaluates the vertical position of the eyelids and the shape and position of the canthi. Although the vertical distance between the center of the upper and lower lids varies, the palpebral aperture is commonly used as a measure of the position of the lids. It has the disadvantage that the lower lid is used as the reference point for the position of the upper lid. In trauma and often in lid disease, the lower lids are not level ( Fig. 18-14 ), and a false impression of the lid positions is given. A better measure is the margin reflex distance (MRD). The patient is asked to look at a flashlight ( Fig. 18-15 ). The distance from the corneal light reflex to each upper lid and each lower lid is recorded. This gives an accurate record of the position of all four lids. It remains reasonably accurate even if one eye is displaced by hemorrhage, swelling, or an underlying squint. The MRD is recorded in the following manner:
3 1 MRD 5 5


In this case, the right upper lid is 3 mm and the left upper lid 1 mm above the corneal light reflexes. Both lower lids measure 5 mm from the light reflexes.
The distance between the medial canthi should be approximately one half of the distance between the centers of the pupils with the eyes in the primary position. Telecanthus and any displacement of the lateral canthi should be documented. Disruption of the canthal tendons frequently leads to rounding of the angle of the canthi.
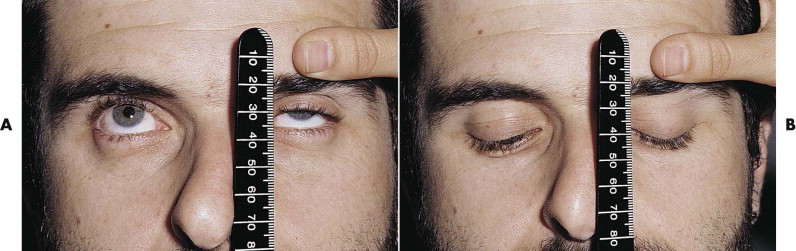
Eyelid Movement
To estimate the function of the levator muscle of each upper lid, stabilize the brow with a thumb, and hold a ruler directly in front of the eyelids. Ask the patient to look up and down, and measure the excursion of the upper lid in millimeters ( Fig. 18-16 ). The normal upper lid moves 12 to 15 mm from upgaze to downgaze. If there is no measurable levator function because of swelling or hemorrhage, look for any evidence of muscle action. The levator may cause only the slightest movement of the lid or dimpling of the upper lid skin. Bruising alone without transection of the levator can lead to a marked decrease in levator function ( Fig. 18-17 ). Surgical emphysema causes a mechanical ptosis that resolves over several days as the emphysema disappears ( Fig. 18-18 ).

Eye Position
Measure the position of each globe in all three planes. A ruler is used to measure the vertical and horizontal position of the globes ( Fig. 18-19 ). The center of the pupil and the medial limbus are useful reference points. A Hertel exophthalmometer is used to measure anteroposterior position ( Fig. 18-20 ). Because the Hertel exophthalmometer rests on the lateral orbital rims, it is not accurate in the presence of displacement of the zygoma. In this case, a rough estimate of anteroposterior displacement of the eyes can be made by looking over the patient’s forehead from behind ( Fig. 18-21 ). The relative positions of the eyes can be assessed easily.


Eye Movement
Check that the eyes move together in horizontal and vertical directions. Record the presence of diplopia and the direction of gaze in which the images are most widely separated.
Lacrimal System
Inspect the medial canthal areas and the nose. A fine probe (size 00) may be passed into the lacrimal puncta and along the canaliculi to assess continuity. Alternatively, saline stained with fluorescein may be gently syringed through the canaliculi ( Fig. 18-22 ). As a result of nasoethmoidal fractures that have damaged the walls of the nasolacrimal duct or sac, the fluid may leak through a defect into the tissues and give the false impression of a patient’s nasolacrimal system. Patency of the lacrimal system is confirmed if fluid can be seen beneath the inferior turbinate. Fluid stained with fluorescein fluoresces green with a cobalt blue light.

Special Studies
It is important to exclude retained foreign bodies within the periocular tissues or globes. They are easily visible with plain radiography or computed tomography.
A photographic record of the extent of the injuries at presentation is useful for medicolegal purposes and for planning future treatment. The photographic department may not be available, and it is helpful to have access to an alternative camera in the department. The most useful magnifications are for one eye (1 : 1), both eyes (1 : 3, 1 : 4), and full face (1 : 10). A suitable standard film (nondigital) camera should have a lens with an approximately 100-mm focal length, a suitable flash, and 100 ISO film speed. A digital camera should be capable of the same range of magnifications and a resolving power in excess of 3 megapixels.
Assessment
History
An accurate account of the cause of the trauma allows a preliminary estimate of the depth and extent of the injury. Blunt trauma frequently leads to diffuse contusion with irregular wound edges, whereas sharp objects cause wounds with smoother edges that are often deeper.
Examination
Tissue swelling or a reduced level of consciousness may prevent a full assessment. A stepwise approach to the examination of the periocular soft tissues is helpful.
Gross Pathology
The examination assesses edema, ecchymosis, crepitus, and hematoma. It is important to differentiate an orbital hematoma from preseptal hemorrhage. An orbital hematoma has a sharply limited edge ( Fig. 18-8 ). The globe may be proptosed and eye movements reduced. In contrast, preseptal hemorrhage ( Fig. 18-9 ) may be extensive, causing considerable local swelling but without proptosis of the globe or limitation of eye movements. A subconjunctival hemorrhage arising from an orbital hemorrhage ( Fig. 18-10 ) has no posterior edge but disappears posteriorly around the equator of the globe. Subconjunctival hemorrhages due to direct trauma ( Fig. 18-11 ) may be localized with the whole edge visible, although the posterior edge is often well posterior and may not be visible.




Record entry wounds, estimate the depth of wounds, and document any possible loss of tissue. Record whether the lid margins are involved in any laceration. Notice lacerations involving the medial canthus, the presence of telecanthus, and aponeurosis or lacerations in the upper lid that may have damaged the levator muscle.
Exclude blunt or penetrating trauma to the eye, particularly penetrating injury of the globes if the eyelids are lacerated ( Fig. 18-12 ). Check the visual acuity. Examine the pupils for their size at rest and their reaction to light.
The swinging flashlight test ( Fig. 18-13 ) is valuable for identifying optic nerve trauma. To perform this test, dim the lights in the examination room, and if the patient is able to cooperate, indicate a distant target to look at. With a bright light, illuminate first one eye for 2 seconds and then the other for 2 seconds. Swing the light backward and forward in this fashion, and observe the pupil reactions. In the absence of optic nerve trauma (or disease) or widespread retinal trauma, the pupils remain small in both eyes, apart from momentary dilatation during the transit of the light from one eye to the other. In the presence of unilateral trauma to the optic nerve or with widespread retinal trauma, the pupil on that side dilates instead of remaining constricted as the light is moved from the normal eye to illuminate that eye. If the patient is mobile, a slit-lamp examination with measurement of the intraocular pressures is important at this stage.

Eyelid Position
The examination evaluates the vertical position of the eyelids and the shape and position of the canthi. Although the vertical distance between the center of the upper and lower lids varies, the palpebral aperture is commonly used as a measure of the position of the lids. It has the disadvantage that the lower lid is used as the reference point for the position of the upper lid. In trauma and often in lid disease, the lower lids are not level ( Fig. 18-14 ), and a false impression of the lid positions is given. A better measure is the margin reflex distance (MRD). The patient is asked to look at a flashlight ( Fig. 18-15 ). The distance from the corneal light reflex to each upper lid and each lower lid is recorded. This gives an accurate record of the position of all four lids. It remains reasonably accurate even if one eye is displaced by hemorrhage, swelling, or an underlying squint. The MRD is recorded in the following manner:
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


