As societies become increasingly litigious, there is a considerable likelihood that a surgeon treating patients who have sustained facial injuries will become a participant in the litigation process. The prominent visibility of the face and its importance to each individual ensures that its physical characteristics and emotional perspective are both highly valued and guarded.
Most likely, this participation will involve a civil suit in which the patient is taking action against the driver of a car, an employer, or the owner of a dog. From this perspective, the physician is providing information on the extent of the wounds, the care provided and that potentially needed, and any permanent injury (e.g., scars, dysfunction). As medical insurers become increasingly vigilant and more financially restrictive, the physician who participates in the care of the facial wound may also assist the patient’s legal representative in obtaining the maximal medical benefits that are due under the guidelines of the health policy. Lastly, the specter of being a named defendant in a medical liability suit is an ever-present consideration, albeit the most unpleasant one.
When treating an individual with a facial injury, the surgeon must be aware that, as the medical record is being created, a legal record is simultaneously being formed. The recording of patient information through emergency department records, hospital charts, office notes, or operative reports establishes unchangeable evidence of what occurred and how the patient was medically treated. Being as meticulous in clinical record keeping as in the treatment of the patient will always serve the physician well.
Several aspects of the legal system are worth reviewing so that the treating physician may have some perspective on the medicolegal process. This information is useful because it relates to how these issues may directly affect the care delivered and how such events may be interpreted in the future. The first part of the chapter is written primarily from the perspective of the legal system in the United States and the second part for the United Kingdom; it is acknowledged that many countries have different medicolegal laws that are variably enforced.
Tort Law
Tort law is the branch of the law through which an aggrieved individual seeks compensation to right a wrong that was done to him (or her) in a civil context, usually the wrongful act of another person. However, failure to act when there is a legal duty to do so may also subject the wrongdoer to liability for his omissions. Some wrongful acts may be criminal in nature (e.g., battery) as well as being a civil tort. If the wrongdoer is prosecuted criminally, he (or she) may also be subject to civil liability without double jeopardy.
The most common tort for which a facial reconstructive surgeon may become involved in litigation is negligence. Although the surgeon treating facial injuries need not be overly concerned with the legal definition of negligence, its proof requires four separate elements: (1) the existence of a duty, (2) breach of the duty, (3) causation (between the breach of duty and harm suffered), and (4) damages.
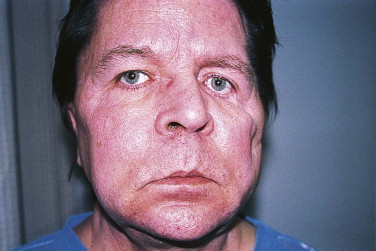
Negligent operation of a motor vehicle may be the most common type of tort resulting in a facial injury. This usually occurs when an individual suffers injuries from being hit by a car operated by another driver. More rarely, an action may originate from an injured passenger against the driver of the motor vehicle in which the person was riding. Animal bites, particularly in children, are an especially obvious injurious circumstance in which litigation rates are high relative to the occurrence of injury ( Figs. 2-1 through 2-3 ). Unsafe maintenance of premises, manufacture of defective products, and intentional torts such as battery are also commonly encountered in clinical practice.


The Treating Physician and Litigation
When a physician encounters a patient with a facial injury and there is some suspicion that tort litigation may result, he should be thinking of his potential role in any lawsuit.
Documentation is of the utmost importance. This means that records should be complete, accurate, and without editorial comment. The events that resulted in the facial injury should be noted in the patient’s medical record. The presence of underlying medical conditions, such as acute drug or alcohol intoxication, is a very important part of the initial medical record. However, if the physician is going to document the use of illicit drugs or alcohol, he must not speculate, and there should be confirmatory medical test results to support these comments.
Documentation of a facial injury should go beyond a written chart note or dictated operative report. Exact measurement of all lacerations should be taken and recorded, either in the emergency department note or as part of the operative report. Such wound measurements are often taken anyway, because the billing of wound closures (CPT codes) is based on the length and depth of the wound. Diagrams may be helpful, but preoperative and postoperative photographs are invaluable and should be taken whenever possible. Digital photography is the standard. Today’s cell phones have such good-quality cameras that there is little reason why photographs cannot easily be taken and transferred to the patient’s medical record ( Fig. 2-4 ).
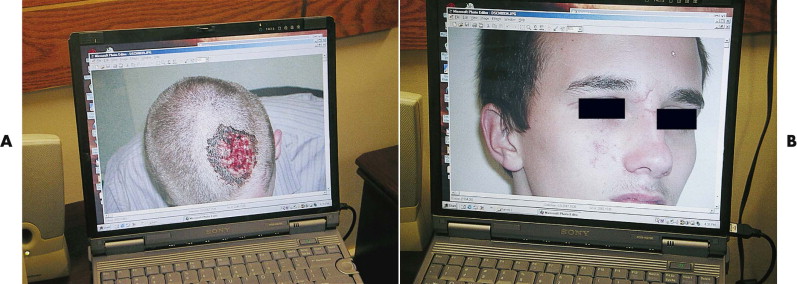
There is no aspect of medical care in which photographs are more widely helpful than the treatment of facial injuries. The establishment of visual documentation in the medical record has numerous merits in the present and potential future care of the patient. Thorough documentation of facial injuries creates a record for the patient to review in the future. This serves to educate the patient about the severity of the initial injuries. This is very useful, because many facially injured patients will need reconstructive surgeries or scar revisions. An appreciation of the original problem may help the patient understand why such procedures are necessary. Furthermore, if a physician is going to become involved in any litigation, either willingly or reluctantly, good photographic documentation of the facial wounds will help both parties to understand the nature and severity of the injuries and may increase the likelihood of a settlement before trial or sometimes before a suit is filed.
The more ambiguous the nature and extent of the injuries appear in the medical record, the more room the attorneys will have for arguing a position that is favorable to their client, leaving the treating physician in the middle of a legal tug-of-war in which he is not likely to be an enthusiastic participant.
The Treating Physician and Litigation
When a physician encounters a patient with a facial injury and there is some suspicion that tort litigation may result, he should be thinking of his potential role in any lawsuit.
Documentation is of the utmost importance. This means that records should be complete, accurate, and without editorial comment. The events that resulted in the facial injury should be noted in the patient’s medical record. The presence of underlying medical conditions, such as acute drug or alcohol intoxication, is a very important part of the initial medical record. However, if the physician is going to document the use of illicit drugs or alcohol, he must not speculate, and there should be confirmatory medical test results to support these comments.
Documentation of a facial injury should go beyond a written chart note or dictated operative report. Exact measurement of all lacerations should be taken and recorded, either in the emergency department note or as part of the operative report. Such wound measurements are often taken anyway, because the billing of wound closures (CPT codes) is based on the length and depth of the wound. Diagrams may be helpful, but preoperative and postoperative photographs are invaluable and should be taken whenever possible. Digital photography is the standard. Today’s cell phones have such good-quality cameras that there is little reason why photographs cannot easily be taken and transferred to the patient’s medical record ( Fig. 2-4 ).
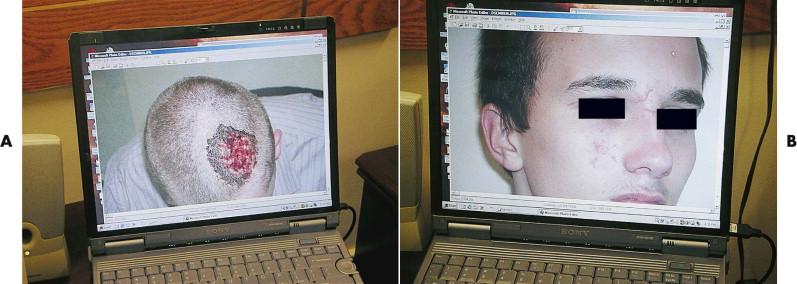
There is no aspect of medical care in which photographs are more widely helpful than the treatment of facial injuries. The establishment of visual documentation in the medical record has numerous merits in the present and potential future care of the patient. Thorough documentation of facial injuries creates a record for the patient to review in the future. This serves to educate the patient about the severity of the initial injuries. This is very useful, because many facially injured patients will need reconstructive surgeries or scar revisions. An appreciation of the original problem may help the patient understand why such procedures are necessary. Furthermore, if a physician is going to become involved in any litigation, either willingly or reluctantly, good photographic documentation of the facial wounds will help both parties to understand the nature and severity of the injuries and may increase the likelihood of a settlement before trial or sometimes before a suit is filed.
The more ambiguous the nature and extent of the injuries appear in the medical record, the more room the attorneys will have for arguing a position that is favorable to their client, leaving the treating physician in the middle of a legal tug-of-war in which he is not likely to be an enthusiastic participant.
The Litigation Process
The treating physician may expect litigation if the patient has suffered severe, extensive, or disfiguring injuries in a setting of potential negligence. The first concrete indication of a lawsuit is a request for medical records made by the plaintiff’s attorney. Each state has its own statutes governing the handling of medical records requests, and it would be prudent for the physician to become familiar with the laws in the state in which he practices. Under no circumstances should original records be provided; copies should be sent, with the original records kept in the physician’s office at least as long as required by state laws. If litigation is ongoing, a patient’s medical records should not be purged from the files simply because the statutory time for maintenance of medical records has expired. Additionally, a patient’s confidential medical record should never be duplicated and forwarded in the absence of a properly executed release form signed by the patient or the patient’s guardian.
Usually, the provision of medical records does not end the physician’s involvement in the underlying legal matter. The pace of personal injury litigation is most often driven by the plaintiff’s attorney; therefore, the physician’s first contact is likely to be the attorney who is representing the patient. Depending on the attorney’s style and practice habits, the physician may be asked to participate in an informal conference. Frequently, the plaintiff’s attorney asks for a narrative statement to record in writing the content of the conference with the attorney. Typically, the physician is asked to respond to very specific questions regarding the cause of the plaintiff’s injuries, history and physical examination findings, treatment, and prognosis. Some plaintiffs’ attorneys choose to forego the conference, especially if there is not sufficient funding for the case, and simply ask for a narrative report.
Many physicians do not like to become involved in litigation, even if they are not a party to it. However, physicians can always be subpoenaed to testify at a deposition or trial, so this task cannot be completely avoided. In general, cases are far more likely to be settled in advance of trial if both sides have reasonable expectations and as much information as possible about liability and damages. If the response to a request for a narrative report is both clear and complete, the prospects for early settlement are better. However, there may be matters and issues beyond the physician’s control, and this can cause some cases to proceed toward trial despite full cooperation in providing the medical information that is available.
Deposition and Trial Testimony
There are two types of depositions in the litigation process: discovery (or evidentiary) depositions and trial depositions.
Discovery Depositions
The purpose of a discovery deposition is to learn what the deponent’s testimony is likely to be at trial. Discovery depositions are usually taken by defense counsel. Because all depositions are given under oath, and under the penalties for perjury, defense counsel will seek to build a record that may be used at trial to impeach the deponent’s credibility if there are inconsistencies or inaccuracies.
The attorney conducting the deposition will ask a series of questions, usually beginning by asking the deponent-physician about his medical education and training. After the preliminary questions have been asked and answered, the substance of the legal case will be explored. Unlike examination at trial, leading questions are permissible on direct examination. Objections may be made by the plaintiff’s attorney, but the custom in most jurisdictions is for the deponent to go ahead and answer once the objection has been stated, unless advised otherwise. The admissibility of the objections to questions and answers at trial will be decided by the trial judge at a later date. If the plaintiff’s attorney and the defense attorney disagree as to whether a particular question should be answered, they may seek to contact the trial judge for an impromptu ruling, or they may skip the question for the time being and have the deponent answer it at a later date, if that is in accordance with the trial judge’s ruling.
In most jurisdictions, deposition testimony in one matter is admissible in another. If there is a significant chance of a subsequent medical malpractice action arising from the care rendered to the plaintiff, the physician would be wise to seek counsel before attending any deposition. Although medical negligence laws vary from state to state, a showing of negligent care usually must be present if the plaintiff is to prevail in a medical malpractice suit. A mere unsatisfactory medical outcome in the absence of negligence will not typically suffice. However, the requirements for filing a medical malpractice action are not as burdensome as those for sustaining the charges of negligence, so a physician may become a medical malpractice defendant even if the suit is largely without merit.
Trial Depositions
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


