Mandible fractures are among the commonest fractures of the face, and much has been published about their management. Yet despite this wealth of clinical research, debate continues over what is considered to be best practice in some types of fracture. Management has evolved considerably over the past 3 decades, with advances occurring not only in the techniques used to repair fractures but also in our understanding of fracture healing, and the importance of the soft tissues in this process. These developments have resulted in improved outcomes and fewer complications, notably infection and malunion. Consequently patients are now much more likely to be restored to their pre-injury function and occlusion. Transoral, semirigid fixation is commonly undertaken for most “routine” mandibular fractures, thereby avoiding the need for external incisions with their attendant shortcomings. Wire intermaxillary fixation (IMF, also known as maxillomandibular fixation—MMF) is now rarely indicated as definitive treatment, although elastic IMF may still be used to “fine tune” the bite and provide additional fracture support with some semirigid techniques. External approaches and rigid fixation are now usually reserved for more complex cases (such as those that involve extensive comminution, infected fractures, continuity defects, or when immediate bone grafting is required).
However, current indications for semirigid and rigid fixation are not absolute and a degree of overlap still exists between the two, the final decision often being based on personal experience and that gained from reported clinical outcomes and prospective studies. Many aspects of management are still controversial and the literature is replete with publications arguing the case for or against various strategies. Surgical access, biomaterials, plate size and design, and specific fracture groups (such as edentulous, comminuted, or pathological fractures) are just a few areas where controversy continues. For the novice this may sometimes be confusing. This lack of consensus suggests that additional confounding factors may play a role in final outcomes. Patient compliance and their biological variation, aftercare and our individual technical skills, to name a few, no doubt contribute variably to our final results. Nevertheless, these developments have resulted in a faster, safer and a more comfortable return to function. Some of these developments and controversies are discussed.
A Brief Historical Overview
Very early descriptions of mandibular fractures came from the Egyptians in 1650 b . c . and also from Hippocrates who described the treatment of a fractured mandible using circumferential wiring. Later references to fractures and their management include the the Edwin Smith Surgical Papyrus, Salicetti in 1275 and Gilmer in 1887.
For much of the 20th century, initial attempts at managing mandibular fractures were limited mostly to maxillomandibular fixation (described later), or Gunning-type splints. Direct fixation through an open approach was generally avoided in this preantibiotic era, due to high infection rates. Only on occasion was this was used in selected cases, or in some edentulous patients. Fracture fixation using “bone plates” was later reintroduced, initially into the German-speaking literature by Luhr and Spiessl in 1968 and 1972. Further work has since helped to develop many of the principles now advocated by the Arbeitsgemeinschaft für Osteosynthesefragen (Association for Osteosynthesis/Association for the Study of Internal Fixation [AO/ASIF]).
Initial attempts at fracture fixation were based on the orthopedic principles of the time, in which callus formation was believed to indicate a failure of the healing process, due to movement at the fracture site. This resulted in the development of rigid, but bulky “compression” plates, which by necessity were placed through large skin incisions in an attempt to provide absolutely rigid fixation. However it later became recognized that satisfactory reduction and healing was also possible without requiring this degree of rigidity, using much weaker fixation (i.e., IMF). But some considered it to be potentially dangerous and was certainly unpleasant for the patient. Each of these two approaches (rigid fixation and IMF) had advantages and disadvantages over the other. IMF in some countries required the patient to remain in hospital for the 6 weeks or so of fixation and posed an obvious threat to the airway. On the other hand compression plating had high morbidity, such as unsightly scarring, risks of nerve injury (facial and inferior alveolar), plate infection, and the need for a second procedure to remove the plates. It was also a very unforgiving technique, which could not be used to repair the thinner bones of the upper facial skeleton.
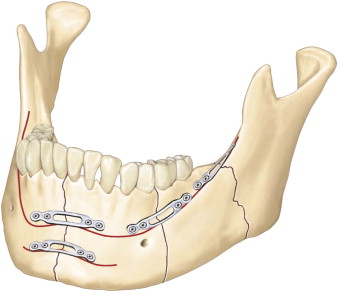
In the 1970s, Michelet introduced a new technique for mandible fixation using smaller “miniplates” which could be placed through the mouth. These “monocortical” plates could be secured using much smaller screws which only needed to engage the outer cortical bone. This advance was subsequently modified by Champy and colleagues, whose biomechanical studies resulted in the concept of “ideal lines of osteosynthesis” ( Fig. 15-1 ). This concept was analogous to the principle of the suspension bridge. By defining lines of tension across a load-bearing fracture, smaller and thinner plates (and sometimes wires) could provide adequate fixation to enable bone healing. The key development here was that the fracture support, provided by these smaller plates, was considered adequate and did not need to be rigid—hence the term semirigid . Consequently the use of monocortical screws allowed greater flexibility in plate positioning over these lines of tension. This use of smaller miniplates was subsequently extended into the rest of the facial skeleton, being miniaturized further for periorbital and cranial non–load-bearing areas and are now in common use today.
Most recently, bone-plating systems made from resorbable polymer have been developed. Material-related complications (such as migration of titanium, thermal paresthesia and the need to remove plates) have all been reported and this has led to the search for more biocompatible materials. These polymers are generally degraded by hydrolysis into water and carbon dioxide and have been reported in some cases to reach mechanical rigidities similar to that of titanium. Resorbable materials were initially designed for use in craniofacial surgery, due to the minimal loading requirements. However as they became stronger, their use was later extended to the treatment of midfacial fractures and then orthognathic surgery. Within the past decade increasing reports have been published of their use in mandibular fractures, although it is still unclear whether or not all systems are comparable to the commonly used miniplates. Biodegradable materials have a number of disadvantages (costs, brittleness, difficult handling, inflammation and swelling during degradation). These need to be balanced against those of titanium (cost, infection, possible long-term toxicity and need for removal).
Even more recently the use of adhesives to fix bone fragments has received interest in both orthopedic and maxillofacial surgery. The idea itself is not new —the notion of bonding bone using biological materials was proposed by Gluck more than a century ago. Adhesives have several advantages over plating. They can secure small fragments and may therefore be useful in comminuted fractures. It has been suggested that by providing more diffuse fixation, adhesives result in a more uniform distribution of loads across the fracture site, compared to the irregular loading that occurs at screw sites. This may reduce the risk of overloading the plate and subsequent failure. It has also been reported that some adhesives act as “subchondral spacers”, smoothing out joint surface irregularities in articular fractures. However, compared to those adhesives used in soft tissue trauma, the biocompatible requirements for bone adhesives need to be stricter, if they are to be safe, easy to use, and effective in load-bearing fractures. Cyanoacrylates, methacrylates, aldehyde-based, and fibrin systems have all been evaluated at some point and research is still ongoing. Adhesives related to polymethylmethacrylate (PMMA), used extensively in dentistry and in hip surgery, show some promise, but this is still a relatively new field of research.
Epidemiology
Much has been published on the causes of mandible fractures, which vary from culture to culture, but include assault, motor vehicle collisions, work-related injury, falls, sport-related injury, pathologic fractures, and projectile missiles. A number of large reviews have been published over the years with differences in etiology, varying between different clinical settings. In urban populations, the most frequent cause of mandibular fractures is often interpersonal violence, while in more rural areas motor vehicle collisions are a more common cause. Young men are almost universally more commonly injured than women and in many countries alcohol is often a significant contributing factor—hence the (paraphrased) expression “Testosterone and alcohol are a potentially dangerous mix”!
Epidemiology
Much has been published on the causes of mandible fractures, which vary from culture to culture, but include assault, motor vehicle collisions, work-related injury, falls, sport-related injury, pathologic fractures, and projectile missiles. A number of large reviews have been published over the years with differences in etiology, varying between different clinical settings. In urban populations, the most frequent cause of mandibular fractures is often interpersonal violence, while in more rural areas motor vehicle collisions are a more common cause. Young men are almost universally more commonly injured than women and in many countries alcohol is often a significant contributing factor—hence the (paraphrased) expression “Testosterone and alcohol are a potentially dangerous mix”!
Initial Assessment
“If you leave the patient facing towards heaven, it won’t be long before they get there” (paraphrased, original source unknown), underlines the importance of good initial care and assessment.
The immediate care of the traumatized patient is covered elsewhere, but is especially important when complex mandibular fractures exist. The American college “ATLS” system of care in the multiply injured patient is commonly regarded as the gold standard and is now taught in over 40 countries worldwide. However its “blind,” unthinking, application to patients with coexisting facial injuries can result in a number of complications (notably airway), especially in those patients with associated head injuries, a full stomach, and high blood alcohol. Such patients need close observation and should never be left unattended while immobilized on a spine board.
Crudely speaking, patients can be placed into one of two groups:
- 1
High-velocity or deceleration injuries, where coexisting torso injuries exist and ATLS principles are required
- 2
The “walking wounded,” where other injuries have been ruled out
In both scenarios assessment always starts with the airway, while simultaneously protecting the cervical spine until injury can be excluded. “Clearing” the neck by clinical examination can usually be done in alert, cooperative patients and many guidelines exist. Where concerns exist about cervical spine injury, imaging is necessary, although how this is best done is more controversial. The best approach is to follow local evidence-based protocols, which usually exist in most trauma units.
With regard to initial assessment (during the primary survey), establishing the presence of those mandibular fractures placing the airway at risk, is a crucial early step. Although an appropriate verbal response is encouraging, direct inspection of the oropharynx must always be undertaken to rule out oral bleeding, mobile and unstable fractures, loose teeth, and foreign bodies, all of which place the airway at risk in supine patients. Correctly fitting rigid collars restrict mouth opening, making assessment difficult ( Fig. 15-2 ), but in all cases of significant facial trauma should be loosened enough to enable thorough examination. During this time manual in-line immobilization of the neck provides continued protection. Precise sizing and placement of collars is important—poorly fitting ones can displace mandibular fractures and aggravate ongoing swelling. Swallowing may be painful and ineffective in mandibular fractures and vomiting is an ever-present risk in all patients, unless the airway has been secured. The use of opiates (recreational or for pain relief) can also compromise the airway in these patients. Airway adjuncts such as the jaw thrust and chin lift can be difficult with comminuted fractures and if unable to sit up, patients who are at high risk of vomiting may require intubation to protect the airway. However not all patients vomit and the difficulty therefore lays in deciding who should have their airway secured as a precaution. This decision is even more critical if inter-hospital transfer or imaging (notably CT) outside the relative safety of the resuscitation room is necessary. For these reasons senior staff with skills in airway management should be involved at an early stage in such cases.

Clinical Features
With all trauma patients, knowledge of the mechanism of injury can give clues to the possibility of unrecognized injuries. For instance, a blow to the forehead can result in blindness, even if there are no fractures present and deceleration injuries to the torso can result in mediastinal bleeding (“bell clanger” effect). Such injuries can easily be overlooked and bear relevance to us if transfers to maxillofacial units are being considered. These, and many others, need to be actively considered and excluded. Similarly, with regard to the mandible, certain mechanisms may also suggest particular injury patterns. The classic “guardsman’s fracture” (midline/parasymphyseal fracture associated with bilateral fractures of the condyles, following a faint or fall onto the chin), is an example where both condyles need to be carefully assessed.
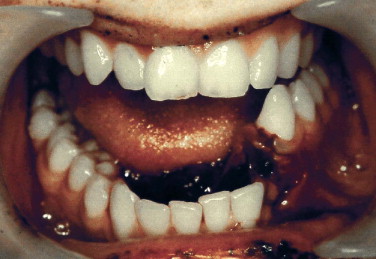
The hallmark of a mandible fracture is a change in the patient’s occlusion ( Fig. 15-3 ). However a normal occlusion does not rule out a mandible fracture. Clinical features are listed in Box 15-1 . If a fracture is felt not to be present, “springing” the mandible by manually compressing the angles (much akin to springing the pelvis), should elicit no pain and is a useful test to avoid unnecessary imaging. Change in the occlusion is one of the commonest physical findings, but can be easily overlooked or misinterpreted in patients with preexisting abnormal dental or skeletal relationships, hence change in the occlusion. However, occlusal changes may also arise as a result of an effusion in the TMJ, or following fractures of the alveolus, teeth, or the maxilla. Occasionally a displaced fracture of the zygoma can “flex” the ipsilateral maxilla resulting in premature contact with the mandible on the same side and diagnostic confusion. Numbness of the lower lip is also a useful sign. This may signify stretching of the inferior alveolar nerve during fracture displacement at the moment of impact, but it can also occur in the absence of a fracture. Documentation of numbness is important as its persistence is often a source of patient dissatisfaction and litigation. Sublingual hematoma is highly suggestive of a fracture involving the lingual plate of the mandible. It should be watched closely in those patients taking anticoagulant medication, notably warfarin, because continued bleeding can result in airway compromise.
- •
Pain, especially on talking and swallowing
- •
Swelling, bruising
- •
Bleeding from the periodontium
- •
Sublingual hematoma
- •
Drooling
- •
Altered bite, with palpable step in the dental arch
- •
Mobility of fractured segment, with palpable crepitus
- •
Numbness of the lower lip
- •
Trismus and difficulty in moving the jaw
- •
Loosened teeth
- •
With medial displacement of the condyle, injury to the trigeminal nerve can result in ipsilateral facial numbness (rare)
- •
The facial nerve may be damaged by a direct blow over the ramus, resulting in ipsilateral facial weakness (rare)
Imaging
Radiographic studies (usually plain films) are not always necessary to exclude fractures of the mandible, so long as a thorough clinical examination has failed to elicit signs of one. In an alert and cooperative patient, springing the mandible and asking them to forcefully open the mouth against resistance at the symphysis are two useful tests. If neither elicit pain the bone is at least clinically intact. However, when a fracture or fractures are evident or suspected, imaging is required, usually as plain films in the first instance, although in some cases with computed tomography (CT).
The principle with plain radiography is to obtain at least two films taken at right angles to each other. Often this is thought to be achieved by obtaining an orthopantomogram (OPT or OPG) and a posteroanterior (PA) view of the mandible, to help visualize the condyles. In reality the direction of view at the symphysis is similar in both films and certainly not at ninety degrees, but this practice has become historical in many units and together with clinical examination seems to be reliable. If doubt exists in the symphyseal region a true lower occlusal view is a useful additional view. This is particularly useful in visualizing the lingual plate and the presence of any avulsion fractures. Panoramic films (OPT) ( Fig. 15-4 ) provide a good overview of all regions of the mandible and are also useful in examining the existing dentition, buried teeth, and location of the inferior alveolar canal. Depending on patient positioning, OPTs may also incidentally view the maxilla, zygomatic arch, hyoid bone, and upper cervical spine, although diagnostic accuracy is limited. However, in order to obtain an OPT the patient must be able to stand, a requirement which may not be possible in the multiply injured scenario (and in some alcohol-related ones too). If this is not possible oblique views can often be obtained to view any regions of interest. This is more labor intensive and costly and subjects the patient to a higher dose of radiation, but at least is possible in the supine patient. Alternatively, imaging can be withheld until the patient is in a better condition. This may be possible in those fractures and patients in whom immediate intervention is not required.

Additional periapical or occlusal radiographs are often helpful in viewing specific areas of concern, especially when dental, alveolar, or oblique fractures are suspected. Selective tomograms or transcranial views of the TMJ are occasionally useful if CT facilities are not available, but are now mostly of historical interest only.
Computed tomography (CT) currently offers the most detailed and comprehensive view of the facial skeleton, but is more expensive and time-consuming. Two-mm cuts usually provide enough detail when imaging the entire facial skeleton. CT may be undertaken in clinical situations where the patient is not able to undergo routine radiographic techniques, such as may occur in the presence of torso, cervical spine, or brain injury. With the newer high-speed machines, the extra time required to image the face is now considerably reduced, and the previous arguments against wasting valuable time to image the face no longer apply. Images can now be viewed in any plane (in addition to the standard axial, coronal, and sagittal views), with three-dimensional reconstruction. If necessary (which is rarely required in mandibular fractures), accurate models of the facial skeleton can now be fabricated and used to create custom-made implants or prostheses. More recently the use of cone-beam computed tomography (CBCT) in dentistry has been extensively reported. It is now regarded by some as an accurate and reliable alternative to conventional CT, providing good quality images with less radiation. Both CT and CBCT are usually reserved for complex fractures, to help in the planning of fractures of the condyle, or when concomitant midfacial or orbital injuries are present. However, for most “walking wounded” fractures plain films are enough.
Other imaging studies can be helpful in very specific circumstances, but are rarely required. Magnetic resonance imaging (MRI) is of very limited value in evaluating bony injuries, but may be helpful to delineate injuries to the intracapsular disc of the TMJ or associated soft tissues. Ultrasound has occasionally been used to determine condylar position after fractures. Supraselective angiography and embolization can be used when significant bleeding is associated with facial fractures.
Classification of Mandibular Fractures
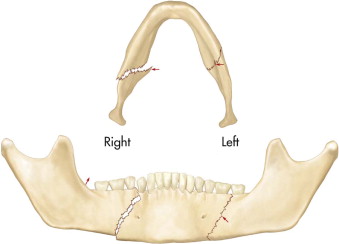
A number of classifications for mandibular fractures now exist, some of which are based on orthopedic experiences. Despite obvious similarities between the long bones and the mandible, some important differences exist. These include differences in development, presence of the dentition, complex muscle attachments, and synergistic bilateral articulations. Fractures of the mandible are often classified and described based on the relationship of the fractured segments, anatomic region, associated muscular anatomy and the involvement of the dentition. Unfortunately these are of limited usefulness when it comes to the “nuts and bolts” of planning treatment. However the influence of the pterygomasseteric muscle sling and its role in displacing angle fractures (favorable and unfavorable fractures) is important when closed management is being considered. The terms favorable and unfavorable refer to the orientation of the fracture (as viewed in the horizontal or vertical plane) and the likelihood of subsequent impaction or displacement of the bone fragments ( Fig. 15-5 ).
Basic Principles of Fracture Management
Whatever type of treatment is undertaken, the main aims in management are as follows:
- •
adequate (or anatomical) reduction of the fractures
- •
adequate stability to allow healing
- •
restoration of pre-injury occlusion
- •
restoration of mandibular function
- •
avoidance of complications (notably infection, malunion, nonunion, and nerve injury)
Regarding the first two points, what is considered as “adequate” is still not clearly defined in the literature and opinions vary, hence the many alternative treatments which have been successfully used. For example, perfectly acceptable functional outcomes can be achieved in patients without anatomical reduction of the fracture. Furthermore, intermaxillary fixation (IMF), semirigid fixation, and rigid fixation are all well know to result in healing, yet the degree of stability each produces across fracture sites varies between them. These points are discussed later.
In orthopedic surgery it is often taught that the success of fracture management depends not only on the condition of the bones and how well they are repaired, but also (and mostly) on the condition of the overlying soft tissues. Consider for example two identical fractures, one of which is closed and covered by healthy, well-vascularized soft tissues, the other being exposed through a mucky (infected), open wound following a crush injury. Whether the fracture is in the leg, arm, or mandible, intuitively outcomes would seem to be better with the first fracture than with the second. This is not the whole story, but does highlight the importance of the soft tissues and in particular the blood supply in the healing process. In this regard the mechanism of injury gives useful clues as to the likelihood of injury to the soft tissues. Comminution in a fracture implies high energy transfer—more energy is also transferred to the soft tissues in the process of sustaining the fracture. Compare, for instance, fractures following a single punch, being kicked by a horse, blast injury, and being shot. Each mechanism carries with it increasing amounts of kinetic energy, potentially compromising the vascularity of the tissues. The worse the blood supply, the greater the chances of infection, non-healing, and /or sequestration.
Excessive movement across the fracture also has an adverse effect in healing by preventing vascularization of the fragments. The judgment here is what do we mean by “excessive”—micromovement has been shown to stimulate bony union.
Closed Versus Open Treatments
In general, treatment is usually composed of the following elements:
- 1
Reduction (such as closed manipulation or open reduction)
- 2
Stabilization (for example with IMF, transosseous wires)
- 3
Fixation (internal or external)
- 4
Rehabilitation
By and large, these components can be achieved by either “closed” or “open” treatments. In many fractures, closed treatment (i.e., the fracture is not exposed) involves analgesia, judicious use of antibiotics if the fracture is contaminated (often via the periodontium), and a soft diet until a firm callus has formed (usually around 4-6 weeks). This may also be termed conservative treatment. In some fractures, IMF may be used to provide additional support and/or pain relief. This approach works well in fractures where the mandible appears undisplaced, stable, with no change in occlusion, and the fracture pattern is “favorable”, that is, unlikely to displace spontaneously (from muscle activity). Outcomes are usually good in compliant and motivated patients. Some clinicians may prescribe antibiotics if the fracture involves a periodontal socket (making it technically compound, or open). Patients must be kept under regular review for approximately 1 month after which the fracture should have healed sufficiently to allow them to return to a normal diet. However, closed treatment does not reduce fractures anatomically —it is wrong to assume that just because the teeth meet, the fractures are in the anatomically correct position.
If the occlusion is deranged or other signs of fracture displacement or mobility are present, then either closed treatment or open reduction can be undertaken. As a temporary first-aid measure, pain relief may be achieved by infiltration of local anesthesia around the fracture site, or if possible by an inferior alveolar nerve block. If the neck is cleared, a soft collar can be used to support the mandible. If the fracture can be reduced manually, a “bridle wire” can be passed around the teeth either side of the fracture and tightened to help reduce it, provide support, and prevent movement ( Fig. 15-6 ). In effect this is the maxillofacial equivalent of an orthopedic backslab used to support limb fractures. By itself, or in conjunction with intermaxillary fixation (IMF), this should be considered when significant delays in repair (i.e., surgery the next day) are anticipated. Any loose dentoalveolar fractures can also be splinted with this technique.

With displaced or mobile fractures a number of treatment options are available. These include:
- 1
Intermaxillary fixation with wire or elastics (closed techniques)
- 2
Open reduction and internal fixation via a transoral approach
- 3
Open reduction and internal fixation via a transcutaneous approach
- 4
External fixation
Each of these has its own specific set of advantages and disadvantages. The choice of fixation depends on the site and type of fracture, condition of the overlying soft tissues, the patient’s general condition and preferences, as well as the personal preference and technical skills of the surgeon. Open treatments tend to be used when closed treatment is inappropriate or has failed. With open treatment, surgical exposure of the fracture site and (hopefully) anatomical reduction and fixation is carried out.
Currently there are two schools of thought when undertaking fixation of mandibular fractures.
- 1
Mandibular fractures need rigid fixation. This can be achieved using dynamic compression osteosynthesis. However, this requires an external approach (with a resulting scar and risks to the mandibular branch of the facial nerve), bicortical screw fixation (with risks of injury to the dental roots and inferior alveolar nerve), and a second procedure to remove the bulky plate once the fracture has healed. The natural curvature of the mandible also makes this a technically demanding procedure, as the plate must fit precisely to avoid distortion of the bone. The thick plates are very difficult to contour, even in experienced hands. Nevertheless, this is a reliable treatment, with a good “track record” and patients can return to normal function quickly. Lag screws also provide rigid fixation and can be placed intraorally (see later). However these are also technically demanding and are only suitable for certain fracture configurations.
- 2
Mandibular fractures do not need rigid fixation. Following fracture, the initial phase of healing is characterized by an inflammatory response within the surrounding hematoma. This is followed by fibrovascular ingrowth and soft callus formation by osteogenic cells. For these processes to occur successfully, the fracture must be adequately stabilized. However, rigid fixation is not essential. Consider for example other land mammals. These may sustain fractures in the wild, which go onto soundly unite, albeit nonanatomically, without any form of artificial stabilization. Furthermore, studies have shown that micromovement, which can occur following semirigid fixation, encourages callus formation and healing. Callus is no longer regarded as a failure of healing. It is just an indication that there is movement across the fracture. Excessive palpable callus is clearly undesirable but, by and large, bone remodeling reduces this over time.
To achieve semirigid fixation large reconstruction plates are not needed. Instead, smaller miniplates, placed along Champy’s lines or zones of tension, produce compression across the fracture. For this to work the periosteum needs to be mostly intact, with good abutment of the fracture ends. Finite element model analysis supports this approach. If necessary, fine tuning of the bite is possible with elastic IMF. Routine removal of the miniplates is not necessary. However, compared to rigid fixation, miniplates are reported to be more likely to get infected and patients still require a soft diet for the same period of time as if treated by IMF.
Within the United Kingdom both techniques are used. However the use of miniplates to apply semirigid fixation is usually the first choice for most mandibular fractures. Nevertheless the rigid approach still has a role to play, particularly in comminuted and in some infected fractures, or where bone grafting is required. If semirigid fixation is not going to be successful, rigid fixation or IMF may then be undertaken. The role of fixation in the edentulous mandible is discussed later.
Timing of Surgical Repair
Ideally all fractures should be repaired as soon as possible, but this does not always happen. For all open fractures (i.e., those associated with an overlying laceration, or involvement of the periodontium), it is generally assumed that the longer the delay in repair, the more likely infection will occur. However what is not clear from the literature is how long a delay is possible without significantly increasing the risks of complications or the likelihood of poor outcomes. Although some clinicians may feel that a delay of more than a few days may put patients at risk, several studies have failed to demonstrate a direct relationship between delays in repair and any increase in complication rates. Excessive fracture mobility, poor oral hygiene, and smoking are probably more likely to result in poor outcomes, and if these can be minimized safe delays may be possible. By and large, it appears that in the absence of airway problems, active bleeding, and excessively mobile (and painful) fragments, most patients can be safely deferred until the next day, or even longer. General anesthesia can be risky and is best avoided late at night. When prolonged delay is anticipated, temporary support using a collar, bridle wire, and/or temporary IMF may be useful interim measures.
Specific Treatments
Closed Techniques
IMF is commonly used in minimally displaced fractures and in fractures of the condyle (a controversial topic in itself, which is discussed elsewhere). Arch bars (wired or bonded to the teeth), hooks, or eyelets (many types exist) are applied to the upper and lower dentition using circumdental wires or adhesives. These are then used to hold the teeth into occlusion. This approach is based on the (erroneous) assumption that if the bite is restored, the bones will be anatomically reduced. This is not always the case, although adequate reduction usually occurs, enough to restore a functional occlusion. Many products now exist and the choice between them is often a matter of personal preference. Whatever fixation device is used, it is important to place it carefully so as not to damage the gingiva or periodontal pocket. Plastic circumdental ligatures (rather like bag-ties or the plastic wrist restainers used by some law enforcers), with cleats, are claimed to speed up the process of applying IMF ( Fig. 15-7 ). Arch bar systems which are bonded to the teeth can sometimes be unreliable, since a dry field during bonding may be difficult to achieve.

All these techniques rely heavily on the presence of an intact dentition and are therefore limited in usefulness in the partially dentate/edentulous patient, or when dentoalveolar injuries coexist. Alternatively the use of bicortical bone screws (IMF screws), which allow the passage of wire ligatures, avoids the need for dental anchorage, but care is required in screw placement if teeth exist nearby ( Fig. 15-8 ). An adequate number of opposing teeth is still required in order for the occlusion to be stable while held in IMF.

One potential complication of IMF is that the condyles can be inadvertently distracted out of the glenoid fossae if the fixation is too tight (notably with wires). The fracture then heals in the incorrect position, only to be noticed once the IMF is released. This is particularly important in condylar fractures. For this reason elastics are often used rather than wires, to provide a degree of “give” and allow the condyles to settle in their correct positions (remember that fracture immobilization only has to be adequate and not necessarily rigid).
Specific Treatments: Open Reduction and Internal Fixation
It is now widely accepted that most displaced craniofacial fractures are best treated by direct exposure, anatomical reduction and internal fixation using miniplates (or microplates), with monocortical screws. This is termed open reduction and internal fixation,
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


