Indications
Failure of conventional endodontic therapy
If conventional root canal treatment, retreatment and surgical treatments have failed and are deemed impossible to perform
Anatomical limitations
Proximity of the intended tooth to nerves (mandibular or mental) or anatomical structures (maxillary sinus) are at risk of damage from the procedure
Surgical access
Surgical access of mandibular molars may be difficult due to dense buccal bone (external oblique ridge) or lingually displaced roots
Tooth factors
Root canal obstructions and restorative or perforation root defects that may be present and are inaccessible to non-surgical or surgical approaches
Contraindications
Root anatomy
Long curved or divergent roots are more prone to fracture during the extraction procedure
Periodontal disease
Teeth with poor periodontal support and tooth mobility are not good candidates for intentional replantation
Vertical root fracture
Teeth where a crack or vertical root fracture has been confirmed following extraction are not good candidates for replantation
It is well documented that avulsed teeth recover optimal function under ideal conditions following replantation. Periodontal ligament cells can be damaged mechanically during extraction/replantation or biologically/chemically during the extra-oral period. Studies have shown that periodontal ligament cells can easily be damaged under stressful conditions such as variable pH, osmotic pressure and dehydration [7–10]. Favourable healing of the periodontal ligament is dependent on how many viable cells are preserved on the root surface [7, 8]. Where the periodontal ligament is damaged, then the potential for surface resorption, inflammatory resorption and replacement resorption (ankylosis) is increased. This type of resorption is a well-known complication of replanted teeth, which adversely affects the long-term outcome [9, 10].
It can be extrapolated from avulsed teeth that optimal periodontal healing is seen when a tooth is immediately replaced in its socket. This ensures minimal damage to periodontal ligament cells reducing adverse effects during the healing period [11–14].
Success rates of intentionally replanted teeth are reported to range from 52 to 95 % [6, 8, 15, 16].
A key to a successful outcome is based on a safe extraction method without causing cracks or root fractures. This is also one of the prerequisites for successful intentional replantation [5]. Orthodontic extrusion and the use of an atraumatic extraction technique have been proposed to ensure a fracture-free safe extraction [17].
14.2 Technique
The objectives of extraction with replantation are to remove the tooth intentionally from its socket, carry out normal surgical root-end procedures extra-orally and replant the tooth. This indication is relevant when non-surgical root canal treatment is not possible or has not been successful and when surgical endodontics is not advisable.
The treatment procedure (Fig. 14.1) should, ideally, be carried out by two operators.
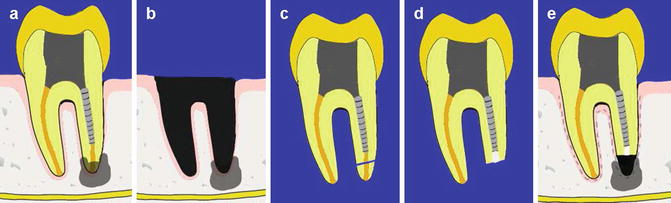
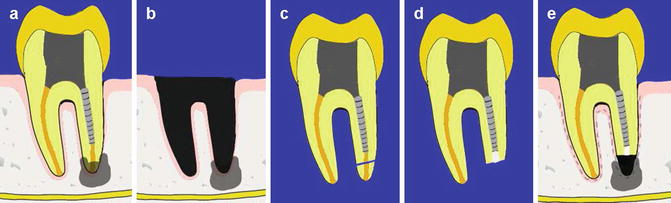
Fig. 14.1
Diagrams representing (a) preoperative view showing the tooth with periradicular lesion close to inferior dental nerve (contraindication to conventional surgery) and fractured post preventing conventional endodontic re-treatments. (b) Post extraction of the apical portion of the socket can be curetted ensuring minimal trauma to the remaining socket walls, (c) root resection, (d) retrograde filling placement, and (e) repositioning
- 1.
The extraction procedure is carried out with minimal trauma. During the extraction scraping or denudation of the periodontal ligament (PDL), the cementum should be avoided. Damage to either can increase the chances of root resorption ensuing postoperatively and inadvertently reducing the prognosis for success. Only the apical part of the socket can be aspirated or curetted with care (Fig. 14.1).
- 2.
Minimal pressure is exerted during the extraction. Care is taken to ensure that the beaks of the forceps are placed on the crown at all times and do not reach beyond the cement-enamel junction. The author has found that placing a rubber band around the handle of the forceps after extraction helps to apply a constant pressure on the crown thereby preventing slippage of the forceps or damaging the tooth. Also the handling of the tooth during the extra-oral period is markedly easier for both root resection and replantation purposes (Fig. 14.2).
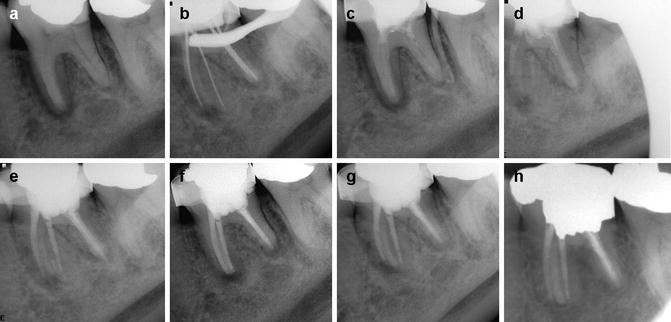
 Fig. 14.2Clinical photographs and radiographs demonstrating (a–c) extraction with minimal trauma, (d, e) root resection, (f–h) reimplantation, and (i) postoperative radiograph demonstrating repositioned tooth
Fig. 14.2Clinical photographs and radiographs demonstrating (a–c) extraction with minimal trauma, (d, e) root resection, (f–h) reimplantation, and (i) postoperative radiograph demonstrating repositioned tooth - 3.
Throughout the extra-oral dry period, when the tooth is resected, prepared for retrograde filling, retrograde filling placement and reimplantation, care is taken to avoid desiccation of the periodontal ligament. Extra-oral time should be as brief as possible. Efficient cutting of the root end and ultrasonic preparation are carried out with effective coolant spray. The periodontal ligament is also kept moist using physiological saline throughout the procedure.
- 4.
Root resection is carried out with a high-speed turbine using copious amounts of water. Resection is carried out with a 0° bevel. Retrograde preparation is carried out with ultrasonics using conventional tips. A retrograde root filling of mineral trioxide aggregate (MTA) is placed (3 mm depth) (Fig. 14.3).
 Fig. 14.3Clinical photographs and radiographs demonstrating (a) preoperative radiograph and (b) clinical photograph of tooth 31 with post crown restoration in place. Note failed endodontic treatment, (c, d) atraumatic extraction, (e–g) root resection, retrograde preparation and MTA filling, (h–i) replantation and suturing, and (j) postoperative radiograph
Fig. 14.3Clinical photographs and radiographs demonstrating (a) preoperative radiograph and (b) clinical photograph of tooth 31 with post crown restoration in place. Note failed endodontic treatment, (c, d) atraumatic extraction, (e–g) root resection, retrograde preparation and MTA filling, (h–i) replantation and suturing, and (j) postoperative radiograph - 5.
The tooth is then repositioned in the socket with minimal trauma. Following repositioning the clinician should press gently on the buccal and lingual plates. The patient can bite on cotton wool roll to help stabilize the tooth and aid in repositioning. Splinting is not usually advocated although temporary splinting using sutures in a figure of 8 can be used. Prolonged splinting (semi-rigid or rigid) is contraindicated since this does not allow for physiological mobility increasing the risk of replacement resorption and ankylosis of the root (Fig. 14.2).
14.3 Outcome
The main reason for failure in replanted teeth is root resorption, specifically surface resorption, ankylosis or replacement resorption (Fig. 14.4). Based on the literature, when the periodontal ligament cells have not been damaged during extraction and replacement of the tooth, if the tooth has been out of the mouth a minimal amount of time and the periodontal ligament has been kept moist, the prognosis is excellent. On the other hand, where damage to the periodontal ligament cells has been considerable, either because of trauma or dehydration, resorption of the root of the tooth will more likely occur.
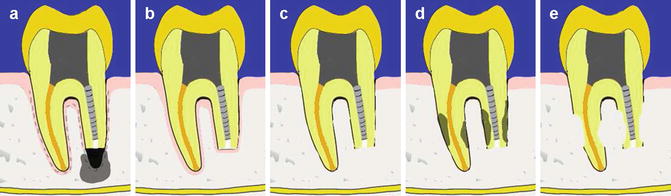
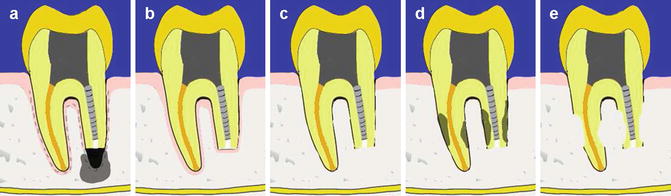
Fig. 14.4
Clinical diagrams showing outcome of intentional reimplantation. (a) Persistent periradicular disease, (b) normal periodontal ligament space (healed case), (c) surface resorption, (d) extensive root resorption, and (e) replacement resorption
14.4 Clinical Cases
Case 1
Failed non-surgical root canal treatment of tooth 46 due to additional untreated canal
A 24-year-old public servant was seen in specialist practice with a fluctuant swelling in the right mandibular area. Clinical examination revealed the first lower right molar was mobile and tender to touch. The radiograph revealed an extensive radiolucency associated with the mesial root. Conventional root canal treatment was undertaken. Access preparation was completed and four canals located. Canal preparation was completed using 1 % NaOCl solution. An intra-canal dressing of calcium hydroxide was placed for a period of 4 weeks. A buccal sinus had developed. A decision was made to carry out further intra-canal irrigation with adjunctive solutions including chlorhexidine and sonic irrigation. Access cavity was reassessed for any missed anatomy with particular reference to the distal root. Canal sizes were increased further. An intra-canal dressing was left in the tooth for a further 6 weeks. At the review appointment, the buccal sinus had failed to resolve. Treatment options were discussed with the patient, and surgical apicectomy was not considered due to anatomical constraints and patient preference. The tooth was subsequently obturated using a warm vertical compaction technique using gutta-percha and AH plus cement. A decision was made to extract the tooth, check for root fractures and replant it after performing an extra-oral root resection and retrograde filling (Figs. 14.5 and 14.6). Following extraction an additional apical foramen was confirmed in the distal root, which had been untreated (Fig. 14.6). The patient was reviewed 1 month, 3 months, 6 months, 12 months, 24 months and 48 months later. The periapical radiograph at 48 months demonstrates good healing with no peri-radicular rarefactions (Fig. 14.7). The tooth remains asymptomatic.