Implant Maintenance and Review
Kyle D. Hogg
Principles
Dental implants can be an aesthetic and predictable method of replacing missing teeth. While dental implants are not subject to caries or endodontic pathology like natural teeth, they can develop peri-mucositis and peri-implantitis, similar to the natural dentition exhibiting gingivitis and periodontitis. Long-term studies show that both biological and technical complications can arise for both implants and implant-supported restorations.1 Despite very high survival rates over long periods of time, the need does exist for maintenance and revision procedures related to dental implants and their restorations. This can result in significant amounts of time and financial resources allocated to keep the implants healthy and functioning appropriately. The need for continual maintenance, a defined individualised maintenance plan consisting of both at-home and professional care, as well as the cost of ownership of the implant rehabilitation should be discussed and documented as part of the process of achieving informed consent prior to treatment. Furthermore, surgical and prosthetic planning should be conducted in such a way as to minimise avoidable biological and technical complications.
The most common biological complications that occur with dental implant treatment are peri-mucositis and peri-implantitis. Peri-mucositis is the plaque-induced reversible inflammatory response of the marginal peri-implant soft tissues (Figure 11.7.1). It does not present with appreciable bone loss. While it is also plaque induced, peri-implantitis features progressive marginal bone loss and clinical signs of infection of the peri-implant soft tissues. Central to the disease process of both conditions is the accumulation or presence of bacterial plaque. A causative relationship has been shown between plaque accumulation and inflammatory changes in the peri-implant soft tissues.2 It is generally thought that untreated peri-mucositis can progress into peri-implantitis, which can lead to implant failure. This is of importance because the incidence of peri-mucositis is fairly common and is likely to be under-diagnosed.
Different maintenance regimens as well as surgical and non-surgical interventions have been proposed for treatment of peri-mucositis and peri-implantitis (Table 11.7.1). Prevention strategies should be aimed at eliminating the accumulation of bacterial plaque on restorations, abutments and any susceptible surface of the implant itself via patient education on home care and hygiene instruction, professional in-office supportive therapy on a recall that matches the individual’s risk assessment, and provision of restorations that facilitate cleaning. At this time there is no definitive regimen or intervention that has been shown to be the most effective in management of peri-mucositis or peri-implantitis.3 When the diagnosis of peri-implant pathology has been made, an interventive treatment should be initiated promptly to avoid disease progression. As peri-mucositis and peri-implantitis have high rates of recurrence, repeated interventions and close monitoring of patients with a past history of the conditions should be considered.
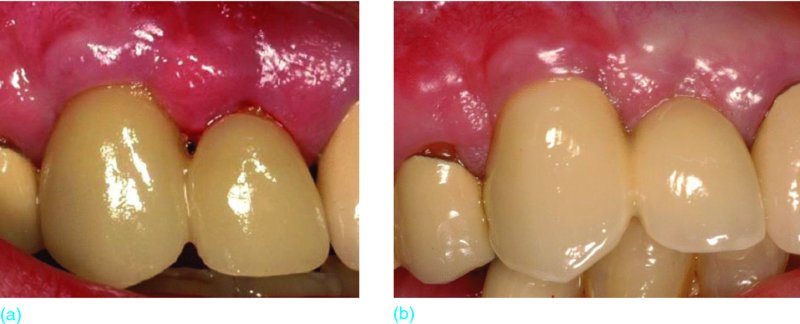
Figure 11.7.1 Comparison of peri-mucositis and healthy peri-implant. Gingival inflammation,
soft-tissue swelling and tissue that bleeds easily on gentle probing (a). The patient was reluctant to perform basic hygiene around the cantilevered provisional fixed partial denture (FPD) UR 2–3 on the implant in the UR 3 position. Healthy peri-implant environment on the same individual around the final cantilevered FPD UR 2–3 after non-surgical supportive therapy and patient education (b). Note the lack of swelling, inflammation and bleeding
Table 11.7.1 Treatment strategies for maintaining or re-establishing peri-implant tissue health
|
Maintaining soft-tissue health |
Treatment of peri-mucositis |
Treatment of peri-implantitis |
|
|
|
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


