Trauma is the leading cause of death from birth to age 44 years. It is third only to cancer and atherosclerosis in all age groups. It is a leading global public health problem, affecting 135 million people a year, and it is estimated that more than 5 million people died from trauma in the year 2004. Of these, more than 1 million (20%) died from Road Traffic Accidents (RTAs) ( Fig. 3-1 ). Other major causes of trauma are sports-related injuries, interpersonal violence, occupational injuries, and falls. In the United Kingdom, falls represent the biggest single group.

Worldwide, approximately 50 million people are severely or moderately disabled as a result of trauma and more than 180 million disability-adjusted life years are lost each year. In the United Kingdom, across all age groups combined, trauma is a leading cause of death, and kills more than 16,000 people per year in England and Wales. Trauma is one of the few disease categories in which mortality is increasing.
The burden of trauma constitutes 12% of the world’s total disease load. It is estimated that the global financial cost of trauma exceeds U.S.$500 billion annually. Apart from the emotional distress, a significant number of trauma victims are injured seriously enough that they are never able to work again. This converts them from productive, employed members of society, paying taxes and contributing to the state’s finances, to net receivers of state aid, dependent on the welfare system for financial support, potentially for many years. This figure is further compounded when it is considered that trauma is largely a disease of younger people.
Since the full financial cost, as well as the physical and emotional suffering, major reviews of the field of trauma management have been carried out with the aim of improving the quality of service and reducing the mortality and morbidity. These reviews have focused both on improving the whole quality of care, from the time of trauma to eventual discharge, with full rehabilitation, and on prevention of the trauma in the first place.
The cost of trauma is escalating in all countries. In developed countries, the proportion of deaths from “preventable” trauma, such as RTAs, is declining but the proportion from other causes, such as falls and interpersonal violence, is increasing. The decrease in preventable deaths results from the twin approaches of prevention and better care. In these countries, society is moving forward from “managing illness” to “promoting wellness” and “preventing illness.” This policy should eventually result in reduced health care costs. However, both prevention and improved trauma management are very expensive to implement and may not be feasible in less developed countries. Consequently, more than 90% of RTA deaths worldwide now occur in the less developed countries.
Improved quality of care reduces both mortality and morbidity. A greater proportion of patients survive, and a greater proportion of survivors make a full recovery. This requires both national strategic planning and development of local provision of care. Experience from management of trauma on the battlefield is translated into more rapid evolution of improvements in civilian care as lessons continue to be learned from conflicts around the globe.
The earlier resuscitation can be initiated after injury and the quicker the victim can be transported to an appropriate care facility, the better. In war zones, this fact has led to immediate support by frontline medics and rapid helicopter evacuation, initially to a field hospital and then to a higher-level center. In the civilian world, it has led to significant investment in prehospital care and in the emergency facilities that are provided at receiving hospitals.
The ideal hospital is a Level 1 Trauma Center where all medical specialties, with full back-up infrastructure, are on site 24 hours a day ( Box 3-1 ). Because these facilities are extremely expensive to provide and maintain, it is more cost-effective to have centralized major trauma units. These need to be located in urban areas of high population, facilitating rapid access and high-quality care for the greatest number of people. Although this has been accomplished in the United States, trauma services in the United Kingdom are still largely designed around the district general hospital (DGH), which serves a population of 250,000 to 400,000. Although the services in these hospitals have been significantly improved, only one patient with major, life-threatening trauma (Injury Severity Score [ISS] >15) may be received in these hospitals on a weekly basis and additionally, the patient will still need to be transferred to a specialized unit if they have sustained cardiothoracic, neurosurgical, or burn injuries.
- •
Identification of major trauma patients at the scene of the incident
- •
Immediate intervention to allow safe transport
- •
Rapid transfer to appropriate trauma center for surgical management and critical care
- •
Coordinated specialist reconstruction
- •
Targeted comprehensive rehabilitation
Work is now progressing to develop regional trauma systems in the United Kingdom. Major trauma cases would be taken directly to a Trauma Center, which would serve a population of 2 to 3 million. These units would expect to receive in excess of 400 major cases per year, leading to better outcomes. Longer prehospital transfer times have been found to make little difference in mortality and morbidity if the destination is a fully staffed trauma center. At present in the United Kingdom, the mortality rate for severely injured trauma patients who are alive on arrival at hospital is 40% greater than in the United States, where there is an established regional trauma system.
The original paper showing that, in the absence of a trauma system, 30% of in-hospital trauma deaths are preventable was published more than 2 decades ago, in 1988. However, the apparent downgrading of a local DGH Accident Center remains a politically very sensitive issue, and effective strategic communications will be required to help the local population understand the rationale behind reconfiguration of major trauma services.
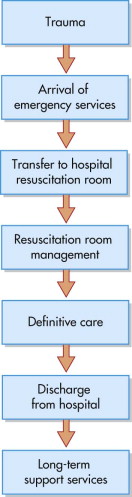
The whole ethos of patient care, from the arrival of the first emergency personnel at the scene through complete rehabilitation and discharge, must be to “ Do no further harm,” and therefore appropriately trained personnel must provide the care ( Fig. 3-2 ).
Prehospital Care
The definition of an integrated trauma system incorporates prehospital care and the need to identify and deliver patients to a place of definitive care safely and quickly. It is essential that trauma services be thoroughly planned and funded to ensure provision of the most efficient and effective services to meet the predictable needs of the population within the capital budget available, because considerable numbers of trauma incidents occur at a significant distance from such facilities.
In the United Kingdom, this has resulted in significant investment in the ambulance services, upgrading their role essentially from first-aid hospital taxi services to first-line care providers. The vehicles themselves are outfitted with essential equipment necessary to provide immediate resuscitation. In addition, most regions have air ambulance facilities to expedite transfer of the victim from the scene of the accident to the hospital. The best environment for resuscitation is a safe, warm, dry, well-lit, fully staffed and equipped area with complete back-up resources—laboratory, imaging facilities, operating rooms, intensive care units, and so on—immediately available.
All emergency services personnel, including police and firefighters in addition to ambulance crews, are trained in basic life support techniques. The initial aim on arrival at the scene is to assess the situation in relation to the safety of both the victims and the service providers. Ambulance crews attending trauma scenes are now specifically trained paramedics; in addition to providing basic life support, they are able to assess the patient and carry out more advanced supportive techniques, concentrating on airway maintenance, respiratory support, immobilization of the patient, and control of external bleeding and shock during any delay that may occur in extricating and transporting the patient to the nearest appropriate facility.
Paramedic crews assess the victims and communicate with the planned receiving hospital, giving them advance warning of the number of patients, the severity of their injuries, and the estimated time of arrival. The crew also routinely carry digital cameras and take photographs at the scene to transport with the patient; these can help clarify the situation and assist in determining the “index of suspicion” of injuries incurred ( Fig. 3-3 ).

Triage
Triage is the sorting of patients based on their need for treatment and the available resources to provide the treatment. This sorting may be carried out by the paramedic team at the accident scene, who decide what level of care is required and therefore to which hospital the patient needs to be transferred. Triage also may be done at the receiving hospital, if it is a small unit (e.g., a U.S. community hospital) with limited facilities and personnel. Triage in this situation may be based on which patients need immediate, life-saving intervention, which can wait, and which are, in fact, beyond saving.
There are two types of triage. Multiple casualties is the term used when the number of patients and the severity of their injuries do not exceed the ability of the facility to provide care. Patients with life-threatening problems and those who have sustained multiple-system injuries are treated first. Mass casualties is the term used to describe the situation in which the number of patients and the severity of their injuries exceed the capability of the facility and the staff. Those patients who have the greatest chance of survival with the least expenditure of time, supplies, equipment, and personnel are managed first.
Preparation at the Receiving Hospital
Each hospital is capable of managing only a limited number of patients. If the number of trauma vicims exceeds the ability of the hospital to handle them, a major incident is called, and a pre-prepared and practiced action plan is implemented whereby neighboring hospitals are alerted and warned that they will also be receiving patients. Natural incidents such as floods, hurricanes, and tidal waves still account for most of the deaths worldwide, but manmade incidents resulting from technological or other human interactions are more common, especially in the urban setting. Terrorist actions in densely populated areas, such as in New York on 9/11/2001 and in London on 7/7/2005, test the best equipped and organized services.
However, under most circumstances, the receiving hospital should be capable of receiving the victims. The hospital must have a fully equipped and staffed resuscitation room with comprehensive back-up of all the necessary support teams, such as radiology, blood bank, and ICU.
A formally constituted trauma team , ideally comprising specialist anesthetic, surgical, and orthopedic components in addition to the emergency department staff, should be immediately available ( Fig. 3-4 ), with the ability to summon extra specialist assistance (e.g., an obstetrician for a pregnant patient) if necessary. All members should have appropriate training, such as the Advanced Trauma Life Support (ATLS) course, which has become the gold standard and common language of trauma management.

The involvement of maxillofacial surgeons in trauma teams has significant benefits in terms of training and in the early identification and optimal management of craniofacial trauma. As a member of the trauma team, the maxillofacial surgeon must be skilled in trauma life support techniques and capable of dealing with both specialty-specific problems and other life-threatening conditions. In addition, expertise concerning midface injuries and any potential threat to eyesight from trauma and hemorrhage is invaluable.
The team should assemble in the resuscitation room and put on protective clothing. The absolute minimum gear includes rubber latex gloves, plastic aprons, and eye protection, because all blood and body fluids should be considered to be infected with the human immunodeficiency virus (HIV) and hepatitis viruses. In addition, all members of the team should be immunized against tetanus and hepatitis B. Staff who undress the patients should initially wear more robust gloves, because trauma patients often have glass and other debris in their clothing, and ordinary surgical gloves do not provide enough protection.
The team leader should brief the team and assign specific duties, so that each member knows the task for which he or she is responsible (e.g., airway, circulation). To avoid chaos, no more than six people should be touching the patient at any one time. A final check of the equipment by the appropriate team members can then be made. Only minimal preparation of the resuscitation room should be necessary, because it should be kept fully stocked and ready for use at all times.
Once the patient arrives in the resuscitation room, a stop clock is started so that accurate times can be recorded. The patient should be transferred from the stretcher to the trolley in a coordinated fashion to avoid injury to the spinal column or exacerbation of preexisting injuries. The lines and leads should be checked so that they do not become tangled or disconnected.
Initial Assessment of the Patient
Deaths from trauma follow a trimodal distribution ( Fig. 3-5 ). The first peak, constituting 40% to 50% of trauma deaths, occurs immediately or within minutes of the accident, at the scene. The causes are usually related to lacerations of the brain, brainstem, high spinal cord, heart, aorta, or other large blood vessels. Due to the severity of their injuries, very few of these patients survive. Only prevention—safer roads, speed restriction, air bags, and other measures—can significantly reduce this peak of trauma-related deaths, although the speedy arrival of trained personnel who are able to begin immediate resuscitation may save some victims.
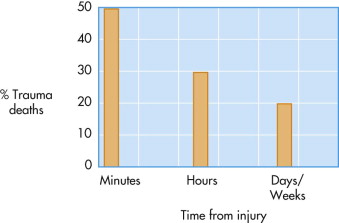
The second peak, representing approximately 30% of trauma-related deaths, consists of those patients who arrive alive in the hospital resuscitation room but succumb to their injuries over the next minutes or hours. This period is referred to as the golden hour . These patients die largely from hypoxia and hypovolemic shock as a result of severe chest injuries with hemothorax or cardiac tamponade, abdominal trauma with ruptured spleen or liver, or orthopedic injuries such as fractured pelvis or long bones associated with significant blood loss.
The third peak is made up of patients who succumb days or even weeks after the traumatic incident from causes such as multiple organ failure, sepsis, or respiratory distress ( Box 3-2 ).
- •
Deaths at the scene : brainstem injury, airway obstruction, heart or major vessel injury
- •
Early deaths: airway obstruction, uncontrolled blood loss, extradural or subdural hematoma
- •
Late deaths : multiple organ failure, respiratory distress, sepsis
The immediate assessment and early management of the trauma patient is comprehensively covered by the ATLS course. ATLS focuses on the second peak, because appropriate and timely intervention in the resuscitation room will both save lives and minimize morbidity, thereby also reducing the third peak in the subsequent definitive care period lasting days or weeks.
Initial Assessment of the Patient
Deaths from trauma follow a trimodal distribution ( Fig. 3-5 ). The first peak, constituting 40% to 50% of trauma deaths, occurs immediately or within minutes of the accident, at the scene. The causes are usually related to lacerations of the brain, brainstem, high spinal cord, heart, aorta, or other large blood vessels. Due to the severity of their injuries, very few of these patients survive. Only prevention—safer roads, speed restriction, air bags, and other measures—can significantly reduce this peak of trauma-related deaths, although the speedy arrival of trained personnel who are able to begin immediate resuscitation may save some victims.
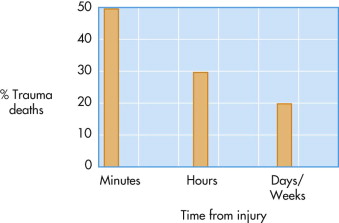
The second peak, representing approximately 30% of trauma-related deaths, consists of those patients who arrive alive in the hospital resuscitation room but succumb to their injuries over the next minutes or hours. This period is referred to as the golden hour . These patients die largely from hypoxia and hypovolemic shock as a result of severe chest injuries with hemothorax or cardiac tamponade, abdominal trauma with ruptured spleen or liver, or orthopedic injuries such as fractured pelvis or long bones associated with significant blood loss.
The third peak is made up of patients who succumb days or even weeks after the traumatic incident from causes such as multiple organ failure, sepsis, or respiratory distress ( Box 3-2 ).
- •
Deaths at the scene : brainstem injury, airway obstruction, heart or major vessel injury
- •
Early deaths: airway obstruction, uncontrolled blood loss, extradural or subdural hematoma
- •
Late deaths : multiple organ failure, respiratory distress, sepsis
The immediate assessment and early management of the trauma patient is comprehensively covered by the ATLS course. ATLS focuses on the second peak, because appropriate and timely intervention in the resuscitation room will both save lives and minimize morbidity, thereby also reducing the third peak in the subsequent definitive care period lasting days or weeks.
Primary Survey and Resuscitation
The patient is transferred to the emergency (resuscitation) room where a rapid primary survey is carried out ( Fig. 3-6 ). Care must follow the safest pathway, diagnosing and simultaneously treating life-threatening injuries in the order in which they would otherwise kill the patient. As each most pressing killer injury is treated, more resuscitation time is created to deal with the next most pressing problem.
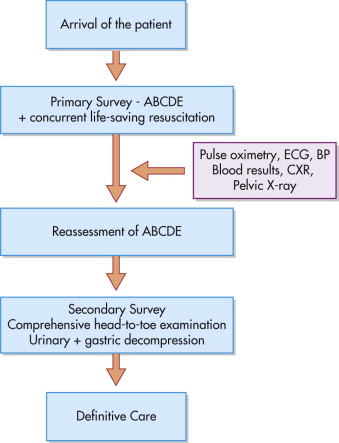
Each patient should be assessed in the same way, and the appropriate tasks should be performed automatically and simultaneously by the team. To facilitate this, the primary survey of the patient follows a strict, sequential “ABCDE” protocol:
-
Airway with Cervical Spine Control
-
Breathing and Ventilation
-
Circulation and Hemorrhage Control
-
Disability–(Neurological status
-
Exposure + environment − completely undress the patient, but prevent hypothermia
To these, another point may be added:
-
Frequent Reassessment must be made
It is essential to ensure that prehospital personnel provide a comprehensive account of the accident scene. In addition to patient details, important information such as the time of the accident, weather conditions, ambient temperature, and other factors such as fires, explosions, hazardous chemicals, and injuries sustained by other victims must all be gathered. Photographs taken at the scene also provide vital information, giving clues to understanding the mechanism of injury and, from that, what injuries might be anticipated (index of suspicion).
Maxillofacial injuries are addressed at this stage only if they have an impact on the airway, breathing, or circulation. Comprehensive assessment and definitive management of maxillofacial injuries occur later, away from the resuscitation room setting.
Priorities for care of the pediatric patient are the same as for adults, and priorities for care of the pregnant woman are similar to those for nonpregnant patients. Pregnancy should be identified early by palpation of the abdomen for a gravid uterus and by laboratory testing for human chorionic gonadotropin (HCG). Early fetal assessment is important for maternal and fetal survival.
Trauma is the fifth most common cause of death in the elderly. Comorbidities such as cardiac, respiratory, and metabolic diseases are more common, and, together with the aging process, they reduce the patient’s functional reserve and ability to respond to injury. The chronic use of medications may also alter the usual physiological response to injury. The narrow therapeutic window frequently leads to overresuscitation or underresuscitation in the elderly, and early invasive monitoring is valuable.
A:
Airway and Cervical Spine Control
There should be a high index of suspicion for cervical spine injury if the patient has maxillofacial injuries or multisystem trauma, if the level of consciousness is altered, or if there is a history of a high-speed impact. Approximately 15% of patients with supraclavicular injuries also have a cervical spine injury, and 5% of head-injured patients have some form of associated cervical, thoracic, lumbar, or sacral spinal injury. Although spinal injuries most commonly occur in the cervical region, other parts of the spine are affected in 45% of cases, and in 10% of cases, there is a second and completely separate spinal injury. Therefore, great care should be taken to prevent excessive movement of the cervical spine during assessment and management of a patient’s airway ( Fig. 3-7 ). Again, the overriding management principle should be, “Do no further harm” ( Box 3-3 ).

Assume that the cervical spine may be injuried, particularly if any of the following is present:
- •
Blunt trauma above the clavicles
- •
Head injury (any patient with altered level of consciousness)
- •
Hypoxia, trauma, alcohol, drugs
- •
Maxillofacial trauma
- •
Multiple trauma (injury above and below the clavicles)
Remember: SUSPECT, PROTECT, DETECT
An assessment must immediately be made as to whether the patient can maintain and protect his or her own airway. The team leader should talk to the patient while the neck is kept manually in a neutral position without longitudinal compression or distraction. This can be achieved simply and quickly by placing one hand on either side of the patient’s head and holding the head in a neutral position, taking care not to cover the ears. If the head is twisted to one side, it should be carefully straightened, ensuring that the neck is not extended or flexed in the process. In the motorcyclist, the neck should be supported from below while an assistant carefully expands the helmet laterally and removes it from above. Removal of the helmet using a cast cutter while stabilizing the head and neck minimizes cervical spine motion in a patient with a known cervical spine injury. The neck is then splinted with a rigid collar of appropriate size to grip the chin.
Much information can be gained very quickly by asking the patient a simple question such as “How are you?” or “What happened?”If the patient gives an appropriate and coherent response, it suggests that the airway ( A ) is clear, that breathing and ventilation ( B ) are sufficiently effective to deliver enough oxygen into the circulation ( C ), which is functioning sufficiently to transport the oxygen to the brain ( D ), which in turn is functioning sufficiently to allow the patient to comprehend and respond. In addition, information about the patient, the medical history, and the details of the accident may be gathered. However, there is a significant caveat: Although the patient’s ABCD factors may be functioning satisfactorily at the time of questioning, they may not be shortly, so that frequent re-examination is essential.
Basic Airway Maneuvers
Supplemental oxygen delivered through a well-fitted reservoir (rebreathing) mask, at a rate of 15 L/min to achieve maximum oxygenation of the tissues, should be given to every trauma patient.
If the patient fails to respond to questioning, formal airway assessment must be immediately instigated. As always, clinical assessment should follow the protocol, “Look, Listen, and Feel . ”
- •
Look to see if the patient is agitated or obtunded. Agitation suggests hypoxia, and obtundation suggests hypercarbia. Cyanosis indicates hypoxemia and can be seen in the lips and nailbeds. Look for the pattern of breathing and use of accessory muscles of ventilation.
- •
Look for facial burns; singed eyebrows, facial hair, or nasal vibrissae; and soot around the lips, in the mouth, or in the sputum (indicating burn injury, inhalational burns, and possibly impending airway obstruction).
- •
Listen for abnormal sounds. Noisy breathing is obstructed breathing. Snoring, gurgling, and crowing noises (stridor) may be associated with partial obstruction of the pharynx or larynx. Hoarseness implies functional laryngeal obstruction. The abusive or belligerent patient may be hypoxic and should not be presumed to be intoxicated.
- •
Feel for the location of the trachea and determine whether it is in the midline.
- •
The mouth should be opened and any foreign objects (e.g., fractured teeth, fillings, dentures) should be removed. The mouth is examined, and any fluid is sucked out. The nature and volume of the fluid (secretions, blood) and evidence of pooling in the oropharynx indicate loss of airway control by the patient.
In an unconscious patient who is lying supine on a gurney, the tongue may fall back and obstruct the airway; a simple chin lift or jaw thrust maneuver can be used to correct the tongue position and open the airway. Those patients with a gag reflex can maintain their own airway. The use of oropharyngeal (Guedel) airways in these patients can precipitate vomiting, neck movement, and a rise in intracranial pressure; therefore, a nasopharyngeal airway is preferred, provided there is no evidence to suggest a fracture of the base of the skull.
A jaw thrust is performed by grasping the angles of the mandible with one hand on each side and displacing the mandible forward. If the patient is breathing spontaneously, high-flow oxygen via the facemask and resevoir bag will provide good oxygenation and ventilation ( Fig. 3-8 ). If the patient is not breathing, a facemask with a bag-valve device (Ambu bag) connected to the oxygen supply and compressed by an assistant will work until formal management of the airway is achieved.

A chin lift should be performed without hyperextending the patient’s neck. The mandible is gently lifted upward using the fingers of one hand placed under the chin. The thumb of the same hand lightly depresses the lower lip to open the mouth ( Fig. 3-9 ).

The oropharyngeal airway must not be used in a conscious patient, because it may induce coughing, gagging, vomiting, and aspiration. During its insertion, care must be taken not to push the tongue backward and thereby block rather than clear the airway. The device is introduced upside-down so that its concavity is directed upward, until the soft palate is encountered. At that point, the device is rotated 180 degrees to direct the concavity caudad, and the airway is slipped into place over the tongue.
Alternatively, the oropharyngeal airway can be introduced directly by using a tongue spatula to depress the tongue, again ensuring that the tongue is not displaced backward as the tube is inserted. This method should be used in children to avoid knocking out loose primary teeth and, potentially, displacing them into the oropharynx.
If the patient vomits, the patient’s head should not be moved to one side unless cervical spine injury has been excluded clinically and radiologically. If the patient is secured on a spinal board, the whole board can be turned. In the absence of a spinal board, the whole gurney should be tipped so that the head is down and the vomit sucked away with a rigid sucking device.
In a conscious patient, a well-lubricated nasopharyngeal airway is inserted in the nostril that appears to be unobstructed and passed gently into the posterior oropharynx. If obstruction is encountered during introduction of the airway, the procedure is stopped and then retried on the other side.
The laryngeal mask airway (LMA) has an established role in routine surgery to provide a protected airway and also in patients with difficult airways, particularly if orotracheal intubation has failed or bag-mask ventilation is not maintaining sufficient oxygenation. However, it is not a definitive airway because there is no cuffed tube in the trachea. Also, some training is required to use it, and it can be displaced relatively easily. If a patient presents with an LMA already in place, conversion to a definitive airway must be planned.
A multilumen esophageal airway is a form of LMA that has two tubes, enabling occlusion of the esophagus to reduce the risk of aspiration. However, it does not have a cuffed tube in the trachea and therefore does not constitute a definitive airway. The laryngeal tube airway also does not allow definitive airway protection; as with the LMA and the multilumen esophageal airway, plans must be made for it to be replaced by a definitive airway.
Maxillofacial Injuries
Up to 5% of patients presenting to the emergency department have facial injuries, and some may have airway compromise. Maxillofacial trauma demands aggressive airway management, and it may be appropriate for the maxillofacial surgeon to assist the anesthetist in assessing and securing the airway. The following problems may be encountered:
- •
A conscious patient will fight to maintain his own airway. If maxillofacial injuries are present, there is likely to be bleeding from those fractures, probably into the mouth or nose. ATLS principles advocate that the patient should be laid on his or her back with cervical spine control; this maneuver leads to pooling of blood in the nasopharynx and oropharynx, resulting in coughing or, in a more obtunded patient, airway obstruction.
It may be wise to leave such a patient sitting up, protecting the airway until a decision on airway management is made ( Fig. 3-10 ). This decision must be made in the presence of a senior anesthetist and maxillofacial surgeon. The only alternative is formal intubation by means of an orotracheal tube, which in the emergency setting requires general anesthesia, or a surgical cricothyroidotomy.
- •
The midface consists of a series of bony struts passing upward from the upper teeth to the base of skull ( Fig. 3-11 ). These bone struts may fracture with severe impact, and the middle third of the face can be sheared off the cranial base and forced downward and backward along the inclined plane formed by the frontal and sphenoid bones. It should be disimpacted by exerting upward and forward traction on the maxilla using the index and middle fingers of one hand, which are placed inside the mouth behind and above the soft palate, with the palm of the other hand braced against the forehead and applying countertraction.

FIGURE 3-11 Skull showing the plane of the cranial base. With severe trauma to the midface, the facial bones shear off from the cranial base and are pushed down and backward. - •
Voluntary tongue control is lost only when the patient’s level of consciousness is depressed; it is only in such circumstances that the tongue constitutes a threat to the airway. In these patients, a deep traction suture (0 black silk) may be inserted through the dorsum of the tongue and taped to the side of the face. Alternatively, the tongue may be pulled forward with the use of a towel clip. However, both of these techniques can cause additional bleeding, and insertion of an oropharyngeal airway or a definitive airway (if necessary) is preferable.

It is often said that in patients with bilateral symphyseal or parasymphyseal anterior mandibular fractures, the tongue may lose its anterior insertion and then, under the influence of the genial muscles, drop back in the supine patient, blocking the oropharynx. In fact, this is not the case if the patient is conscious, because the tongue is still firmly attached to the hyoid bone, which remains connected to the mandible by the posterior parts of the mylohyoid muscle. In addition, the intrinsic muscles of the tongue continue to exert control.
In elderly patients, it is not unusual to see bilateral fractures of the body of the edentulous mandible, each occurring near the posterior attachment of the mylohyoid diaphragm. Under these circumstances, extreme downward and backward angulation of the anterior part of the mandible may occur under the influence of the digastric and mylohyoid muscles and can compromise the airway. This so-called bucket-handle displacement should be reduced manually to unblock the airway.
- •
Teeth, dentures, vomitus, hematoma, or other foreign bodies may block the airway at any point from the oral cavity to the bronchi, with the right main bronchus being particularly susceptible. Early in the primary survey, the oral cavity should be cleared using a finger sweep followed by aspiration using a rigid sucker. If any teeth, crowns, or bits of denture are mssing, this fact should be recorded and the chest radiograph should be checked to be sure they have not been aspirated.
- •
Soft tissue swelling and edema resulting from trauma to the oral cavity may compromise the airway.
Rarely, maxillofacial trauma is associated with injuries to the larynx and trachea. Any neck swelling, dyspnea, voice alteration, or frothy hemorrhage should be noted, and the neck should be palpated for surgical emphysema, tenderness, and laryngeal or tracheal crepitus at the fracture site. Penetrating trauma to the neck may result in vascular injury with significant hemorrhage, which can cause displacement or obstruction of the airway. Endotracheal intubation should be attempted; if this is not possible, an urgent surgical airway may be necessary. Blunt or penetrating injury to the neck can cause disruption of the larynx or trachea, resulting in airway obstruction or severe bleeding into the tracheobronchial tree. A definitive airway is again urgently required.
Laryngeal fractures—indicated by hoarseness, subcutaneous emphysema, and palpable fracture—are rare but can manifest with acute airway obstruction. If the patient’s airway is totally obstructed, an attempt at intubation is warranted. Flexible endoscopic intubation may be helpful, but only if it can be organized quickly. If intubation is unsuccessful, emergency tracheostomy is indicated, followed by operative repair. However, tracheostomy performed under these conditions can be difficult and time-consuming and may be associated with profuse bleeding. Under these circumstances, surgical cricothyroidotomy may be a life-saving option. If the injury is in the trachea below the potential tracheostomy site, the thoracic surgeons should be involved.
Advanced Airway Maneuvers: Definitive Airway
A definitive airway is defined as an inflated cuffed tube in the trachea. Definitive airways are of three types: the orotracheal tube, the nasotracheal tube, and the surgical airway (cricothyroidotomy or tracheostomy). A definitive airway should be considered if any of the following is present:
- •
Apnea
- •
Inability to maintain a patent airway by other means
- •
The need to protect the lower airway from blood or vomit
- •
Potential compromise of the airway (e.g., after burn injury, other inhalational injury, facial fractures, retropharyngeal hematoma, or sustained seizure activity)
- •
A closed-head injury requiring assisted ventilation (Glasgow Coma Scale [GCS] score of 8 or less)
- •
Inability to maintain adequate oxygenation by facemask oxygen supplementation
Patients who are without a gag reflex should be intubated with an appropriately sized endotracheal tube that has a low-pressure cuff, so that ventilation can be carried out safely. Attempts at ventilation with a bag and mask in these patients may lead to gastric distention with air and can precipitate vomiting. Orotracheal intubation with cervical in-line immobilization is recommended, rather than blind nasotracheal intubation, especially if a base-of-skull fracture is suspected. If this proves to be difficult, a surgical airway is then considered.
The most important determinant of whether to proceed with orotracheal or nasotracheal intubation is the experience of the doctor. Nasotracheal intubation should not be attempted in an apneic patient nor undertaken if a fracture of the base of the skull is suspected.
The route of choice for securing the airway depends on several factors. Between 5% and 10% of patients with blunt trauma of the head and neck have an associated fracture of the cervical spine. Laryngoscopy and orotracheal intubation are generally considered to be safe procedures and can be accomplished with minimal changes in the position of the neck when performed by a competent operator while an assistant immobilizes the patient’s head. Visualization of the cords may require aids such as the gum elastic bougie. Another skilled assistant must provide pressure on the cricoid to protect the patient from aspiration of gastric contents. The stomach may already have been emptied by the passage of a nasogastric tube.
A fiberoptic intubating bronchoscope may facilitate difficult orotracheal or nasotracheal intubation if the patient’s condition permits, but in the presence of distorted anatomy and hemorrhage, the procedure should be attempted only by an experienced anesthetist who is ready to abandon the procedure and proceed to establishment of a surgical airway if success is not achieved rapidly ( Box 3-4 ).
- 1
Altered level of consciousness
- •
Hypoxia
- •
Head injury
- •
Hypoglycemia
- •
Alcohol
- •
Drugs
- •
- 2
Maxillofacial injuries (patient in supine position)
- •
Profuse bleeding
- •
Displaced teeth, dentures, and so on
- •
Facial fractures
- •
- 3
Facial burns (inhalational injury): impending airway obstruction
- 4
Penetrating neck injury: potential compression of airway from closed hemorrhage
- 5
Direct laryngeal trauma
Rapid-sequence induction with anesthetic agents, neuromuscular blocking drugs, and esophageal occlusion by cricoid pressure is best carried out by the anesthetist, who is experienced in the use of these drugs. Before one embarks on intubation, the equipment must first be checked. Anesthetics with duplicate ampules should be ready in labeled syringes, and vasoactive drugs such as atropine should be at hand in case untoward bradycardia complicates extended laryngoscopy. A skilled assistant applies pressure to the cricoid while another assistant stabilizes the neck. Secure venous access and a pulse oximeter are essential.
Patients who have an intact gag reflex require induction of anesthesia and muscle paralysis for the airway to be secured by an oral or a nasotracheal tube. Preoxygenation is essential; while an assistant maintains pressure on the cricoid, neuromuscular blockade is produced with suxamethonium, and intubation proceeds with the onset of paralysis.
In deeply unconscious patients with a head injury, intubation should be preceded by the administration of a cerebral sedative and a muscle relaxant. This avoids dangerous increases in cerebral blood volume and intracranial pressure during laryngoscopy.
Orotracheal Intubation
In-line immobilization of the head must be maintained by an assistant to ensure that no extension of the cervical spine occurs. This is contrary to normal anesthetic practice in the non-trauma patient, where extension of the neck makes visualization of the vocal cords, and therefore intubation, easier.
The laryngoscope, held in the left hand, is inserted into the right side of the patient’s mouth and over the back of the tongue, displacing it to the left. The back of the tongue is observed while the curved blade of the laryngoscope is advanced until the epiglottis comes into view. With care taken not to move the neck, the whole lower jaw is moved anteriorly as the tip of the blade is moved anterior to the epiglottis. Under direct vision, the anesthetist then advances the endotracheal tube through the vocal cords. If a gum elastic bougie is used, an endotracheal tube of the appropriate size is “railroaded” into the trachea. A size 8 tube is usually suitable for women and a size 9 tube for men. The cuff is then inflated, producing an airtight seal. Care must be taken to avoid trauma to the upper front teeth from the laryngoscope.
Proper placement of the tube is suggested but not confirmed by hearing equal breath sounds bilaterally on auscultation in both axillae and detecting no breath sounds in the epigastrium. An end-tidal carbon dioxide monitor will rapidly confirm the presence of the endotracheal tube in the airway. Pressure on the cricoid can only then be released and the tube secured with tapes. Proper positioning of the tube is best confirmed by a chest radiograph once the possibility of esophageal intubation has been excluded.
End-tidal carbon dioxide (CO 2 ) detectors are colorimetric devices that use a chemically treated indicator strip to reflect the CO 2 level. The indicator changes color from purple at low levels of CO 2 (e.g., atmospheric air) to yellow at higher levels. A tan color indicates levels of CO 2 that are generally lower than those found in the exhaled tracheal gases. Patients with gastric distention may have elevated CO 2 levels in their esophagus, which clear rapidly after several breaths, so care should be taken to avoid assessing the results until after at least six breaths. If the colorimetric device still shows an intermediate range, six additional breaths should be taken or given.
After intubation, the patient is appropriately ventilated. Although capnography and pulse oximetry may provide immediate noninvasive assessment of oxygenation and the adequacy of ventilation, arterial blood gas tension should be analyzed at the first opportunity.
Nasotracheal Intubation
Blind nasotracheal intubation requires spontaneous breathing and is therefore contraindicated in the apneic patient. The deeper the patient breathes, the easier it is to follow the air into the larynx. Facial fractures, frontal sinus fractures, base-of-skull fractures, and cribriform plate fractures are relative contraindications and are suggested clinically by the presence of nasal fractures, “panda eyes” ( Fig. 3-12 ), Battle’s sign ( Fig. 3-13 ), and evidence of cerebrospinal fluid (CSF) leakage.


Endotracheal tubes can easily become displaced when patients are transported, so patients who arrive at the hospital with an endotracheal tube already in place must have the proper positioning of their tube confirmed.
Surgical Airway
Inability to intubate the trachea orally or nasally is a clear indication for creation of a surgical airway. If edema of the glottis, fracture of the larynx, or severe oropharyngeal hemorrhage obstructs the airway and an endotracheal tube cannot be placed through the cords, a surgical airway is performed. A surgical cricothyroidotomy is preferable to a tracheostomy for most patients. It is easier and requires less time to perform, and it is associated with less bleeding and fewer complications than an emergency tracheostomy.
Needle Cricothyroidotomy
Life-saving oxygenation can be provided through a large-bore (12- to 14-gauge) cannula (Venflon) that is connected to wall oxygen (at 15 L/min) and has a Y -connector or side hole in the tubing between the oxygen source and the cannula ( Fig. 3-14 ).

Intermittent insufflation (1 second on and 4 seconds off) can be achieved by occluding and then uncovering the open end of the Y -connector or the side hole of the oxygen tubing. Although needle cricothyroidotomy can provide a life-saving supply of oxygen, there are associated problems:
- •
Although oxygenation may be adequate with this technique, ventilation is not, and there is a gradual rise in the P co 2 . The patient can be ventilated by this technique for a maximum of 30 to 45 minutes. Jet insufflation must also be used with caution if obstruction by a foreign body in the glottic area is suspected. Although high pressure may expel the impacted material into the hypopharynx, from which it can be readily removed, significant barotrauma may occur, including pulmonary rupture with tension pneumothorax. Low flow rates (5-7 L/min) should be used if a persistent glottic obstruction is present. During the 4-second periods in which oxygen is not being delivered under pressure, some exhalation occurs. Because of the inadequate exhalation, carbon dioxide slowly accumulates. This limits the use of this technique, especially in head-injured patients.
- •
Patients in whom a surgical airway is required often have a head injury. A rise in P co 2 must be avoided, because it will result in cerebral vasodilatation, a rise in cerebral blood flow, and possibly increased intracranial pressure.
- •
Needle cricothyroidotomy does not protect the airway. In cases of severe maxillofacial trauma with disruption of the normal anatomy and profuse bleeding, orotracheal intubation may fail, and a surgical airway may be necessary ( Box 3-5 ).
Box 3-5Equipment for Needle Cricothyroidotomy- •
Source of oxygen (up to 15 L/min)
- •
Connecting tube with either a Y -connector or a hole in the side
- •
10-mL syringe
- •
12- to 14-gauge Venflon + spare
- •
Needle cricothyroidotomy should therefore be looked upon only as an immediate life-saving procedure. As soon as it has been completed and the P o 2 is improving, arrangements should commence to perform a surgical cricothyroidotomy to effect a definitive and secured airway. An experienced surgeon may elect to carry out a surgical cricothyroidotomy rather than first performing a needle cricothyroidotomy ( Box 3-6 ).
- 1
Establish Universal Precautions against cross-infection.
- 2
Prepare skin quickly with antiseptic.
- 3
Attach syringe to Venflon with 1 mL of air in syringe.
- 4
Identify cricothyroid membrane.
- 5
Immobilize trachea with finger and thumb.
- 6
Insert Venflon in midline, through skin and membrane, at a 45-degree angle, aiming caudad, away from the larynx.
- 7
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


