Type of defect
Extent of defects
Diffuse opacities
Demarcated opacities
Normal
Less than one third
Diffuse lines
White cream
Diffuse opacity
Between one and two thirds
Diffuse patchy
Yellow brown
Demarcated opacity
At least two thirds
Diffuse confluent
Hypoplasia
Staining
Hypoplasia pits
Pits
Hypoplasia grooves
Loss of enamel
Hypoplasia, missing enamel, discoloration
Any other
Clinical History
As many opacities and hypoplastic defects appear to have no obvious cause, a careful and accurate history can pinpoint the timing in relation to possible associated medical events when the defects may have occurred. There will often be a history of repeated attempts to restore teeth with DDE or of a child who is often described as uncooperative. This suggests that because of the sensitivity of affected teeth, children have been more anxious, and local anesthesia has not been successful [1]. In older children, first molars in molar incisor hypomineralization (MIH) may have already been extracted. Table 8.2 summarizes the information that is useful in the clinical history.
Table 8.2
Information from the clinical history
|
Information
|
Relevance
|
|---|---|
|
Family history
|
May suggest a genetic cause (Chap. 5)
|
|
Birth history
|
|
|
Pregnancy history
|
Pregnancy history and mother’s health
|
|
Childhood systemic illnesses
|
Timing of childhood illnesses (Chap. 4)
|
|
Drug and medication history
|
|
|
Allergies
|
Enamel defects in with conditions such as celiac disease (Chap. 4)
|
|
Hypocalcemia
|
|
|
Nutritional problems
|
|
|
Caries history
|
From the primary dentition. If only second primary molars restored – suggestive these teeth may have had DDE
|
The problems, signs, and symptoms given by the child should be recorded. It can sometimes be difficult to elicit concerns or a pain history from younger children but suitable questions often help identify the issues, as suggested in Table 8.3 and described in Chap. 7.
Table 8.3
Children’s history indicating teeth problems
|
Question/comment
|
Explanation
|
|---|---|
|
It hurts to brush my teeth
|
Teeth are too sensitive
|
|
My teacher says I don’t clean my teeth properly
|
Many people think opacities and other DDE are due to a lack of brushing
|
|
Mother describes child never smiling
|
Suggests that children do not like their appearance
|
|
My friends make fun of me
|
Demonstrates a social problem for the child
|
|
My teeth have sharp edges
|
An issue for children with hypoplastic or fractured enamel
|
|
Can’t eat ice cream
|
Indicates a significant sensitivity problem
|
|
Parents say child eats slowly or refuses some foods
|
Suggests sensitive teeth and food trapping
|
Clinical Examination
The clinical examination should note the sites, size, and appearance of DDE on individual primary and/or permanent teeth. This can help to differentiate between isolated insults during development or a genetic- or systemic-related problem that has affected all the teeth. DDE in selected primary teeth can indicate a potential problem in permanent teeth. Developmental defects of the primary second molar alone are suggestive of hypomineralized second primary molars (HSPM) which are predictive of MIH as discussed in Chap. 3. Developmental defects that affect all the primary teeth may indicate a more generalized impact in the permanent dentition (Chaps. 4 and 5). The texture and color of the enamel indicate the presence of hypoplasia and/or hypomineralization. The darker the color, particularly in MIH, the higher the enamel protein content, indicating increased risk of cohesive failure of bonded restorations [2]. Texture can be determined by gently running a probe across the surface. Enamel that is opaque may have a relatively smooth texture reflecting the fact that the surface enamel has mineralized further after eruption. However it is important to remember that from the bonding perspective, the subsurface is still hypomineralized. Color and texture will partly determine the restorative approaches. In hypomineralized enamel without hypoplasia or breakdown, attempts can be made to improve the appearance using microabrasion with and without bleaching or possibly resin infiltration. This is discussed further in Chap. 11. Areas of posteruptive breakdown or hypoplasia should be noted as well as the position of normal enamel that can be utilized to optimize bonding and achieve a sound marginal seal for restorations. In most MIH-affected first permanent molars, there is a band of relatively normal enamel at or below the gingival margin as shown in Fig. 8.1. This allows for good permanent crown margins in late adolescence once pulps have matured and teeth have erupted to provide an acceptable crown height. The challenge in a young child is how to achieve protection of the crowns and pulps of affected teeth until late adolescence (Chaps. 9 and 11 discuss management options).


Fig. 8.1
View of extracted lower first molar crown showing “normal” enamel at or below the gingival margin (Courtesy of Dr. Rami Farah)
Care should be taken when diagnosing caries. What appears to be caries visually may be found to be sound dentine with posteruptive enamel breakdown after the surface has been cleaned and dried. This is important as non-carious dentine should be preserved when restoring hypomineralized teeth and so consideration needs to be given to dentine, as well as enamel bonding in the restorative technique. This is discussed further in Chap. 11.
Radiographic Examination
Panoramic radiography is essential to establish the presence or absence of all permanent teeth and to assess the stage of development of the dentition. This is very important if extractions are being considered as part of the management plan. Calcification of the second premolar crowns will be evident in the early mixed dentition. However, calcification of the third molar crowns does not begin until 7–10 years of age, and this should be taken into account when taking radiographs and planning treatment (Fig. 8.2). The developmental stages of each tooth and anomalies in shape and size as well as in eruption paths should be recorded to consider the possibility of other associated conditions. Bitewing radiographs can help determine if caries is occurring alongside hypomineralization when the shapes of radiolucent lesions are compared and the dentine is examined (Fig. 8.3).
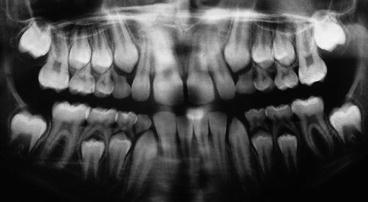

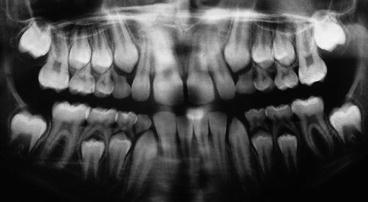
Fig. 8.2
Panoramic radiograph of a 9-year-old boy with severe hypomineralization of the upper first molars. Third molars are not evident

Fig. 8.3
Right posterior bitewing radiograph of an 11-year-old girl with gold overlays on the upper and lower right first molars. Note the hypomineralized enamel on the mesial and distal surfaces and suspected enamel caries on the mesial of the lower first molar
Histological Examination
When a systemic or genetic cause for the DDE is suspected, it is recommended that any available teeth be examined histologically. The histological appearance will help to determine a more accurate diagnosis and provide the clinician with a better understanding of the condition and likely behavior of the tissues when planning restorative care. Histology can be carried out on exfoliated primary teeth or ideally on permanent teeth if they become available.
Medical Examination
Teeth with DDE may be associated with a systemic condition or a syndrome. Occasionally a problem has not been diagnosed, and where this is suspected, children should be referred to a pediatrician with the relevant orofacial history and concerns. It is useful to include copies of radiographs or histology reports which can be added to the general medical record. Where a genetic cause is determined, advice may be sought from a geneticist to determine the genes involved or to give the child and parents more information about the inheritance pattern.
Assessment of Growth and Development
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


