Fig. 11.1
(a, b) Change in enamel on permanent upper incisors following two microabrasion treatments with ongoing use of CPP-ACP with fluoride
Bleaching
A bleaching agent (e.g., 10 % carbamide peroxide) can be applied to the surfaces of teeth with the aim being to lighten color. The exact mechanism of bleaching is unknown, but the release of hydrogen peroxide anions, reactive oxygen molecules, and free radicals is thought to be involved in lightening the stained mineral and protein in the enamel. Discoloration can reoccur because of a combination of chemical reduction of the previously formed oxidation products, marginal leakage of restorations allowing ingress of bacterial and chemical by-products, salivary or tissue fluid contamination, or food color contamination via the permeable tooth structure.
Indications
-
Hypomineralized enamel defects
-
Mild tetracycline staining
-
Mild fluorosis
Contraindications
-
Hypoplastic enamel defects
Techniques
-
Vital bleaching can occur chairside/in the office or at home using custom-designed bleaching trays (vacuum formed).
-
The in-office technique involves application of carbamide peroxide to the surfaces of the teeth with activation of the process by a heat source. This consumes chair time, adding to the expense. It is useful for treatment of mild enamel defects where strict isolation of a single tooth is required.
-
The home bleaching technique utilizes a custom bleaching tray constructed for the maxillary and/or the mandibular teeth. The patient applies the carbamide peroxide (gel) to the teeth via the tray on a daily basis until the desired color change is achieved. There are many proprietary products available, and the principal differences lie in the concentration of carbamide peroxide employed and the amount of hydrogen peroxide released. Current recommendations indicate that a 10 % solution is both safe and successful in modifying tooth color.
-
The concurrent use of a calcium-based product such as that with casein phosphopeptide–amorphous calcium phosphate will control any tooth sensitivity.
-
Review 2–6 weeks later. An 80 % color change should have occurred.
-
Take postoperative photographs including the pre- and posttreatment shade tab for long-term records.
Outcome
Minor ulceration or irritation may occur during the initial treatment which may relate to tray overextension. There may be transient pulpal sensitivity because carbamide peroxide gel (10 %) breaks down in the mouth into 3 % hydrogen peroxide and 7 % urea. Both have low molecular weights that allow them to diffuse through enamel and dentine and cause pulp irritation [24]. If sensitivity occurs, exposure time can be decreased, or it may be necessary to discontinue treatment. To date, there is no evidence that bleaching solutions with a low pH (below the critical pH of 5.2–5.8) causes enamel demineralization [25], possibly because urea, followed by ammonia and carbon dioxide, is released on degradation of the carbamide peroxide elevating the pH. Bond strength of composite resin to bleached enamel decreases initially and has been attributed to the residual oxygen in the bleached tooth surface inhibiting polymerization of the composite resin, but this returns to normal within 7 days [26]. Vital-bleaching systems do not modify the color of restorative materials and any perceived effect is probably due to superficial cleansing. Regular retreatment may be necessary to maintain effective lightening [27]. When considering the use of bleaching products, the clinicians should be mindful of local regulations and seek advice with respect to contemporary legislation.
Direct Restoration with Composite Resin
Composite resin bonded to etched enamel and/or pretreated dentine can be used to restore tooth defects or improve esthetics by replacing or masking areas of discolored or defective enamel.
Indications
-
Demarcated enamel opacities
-
Hypoplastic enamel defects
Contraindications
-
Diffuse enamel opacities
Technique
-
Apply dental dam and contoured matrix strips if required.
-
Selective removal of demarcated lesion with a round diamond bur may be required to optimize esthetics and bonding; however, bonding can also be improved by selective use of GIC, or polyacid-modified composite.
-
The enamel margins can be chamfered with a diamond fissure bur to increase the surface area for retention and blend the composite margin with the enamel.
-
Etch the area, wash and dry, and apply the primer, bonding agent, and the chosen shade of composite. A brush lubricated with bonding agent can be used to smooth and shape before light curing.
-
Remove the matrix strip/dam, polish with graded polishing discs and diamond finishing burs, and characterize the surface if required.
-
Take postoperative photographs for records.
Outcomes
Restoration of localized hypomineralized or hypoplastic defects using composite resin is not usually associated with sensitivity and may not need local anesthesia unless there is caries with extension into dentine. These very conservative resin-bonded restorations are particularly suited to newly erupted incisors (Fig. 11.2a, b). However, when it is not possible or desirable to remove the entire opacity, problems with marginal staining, color matching, and suboptimal esthetics can arise.
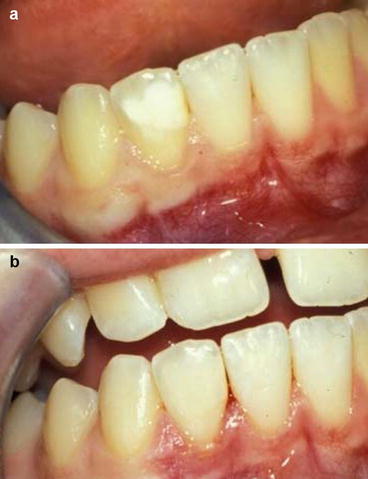
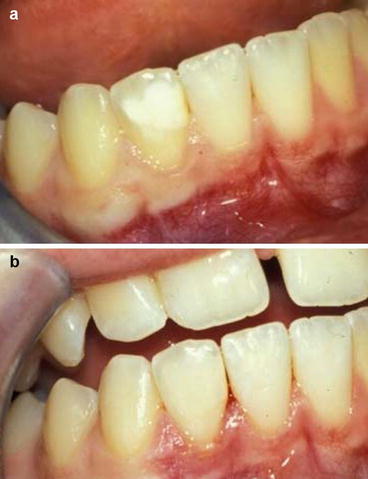
Fig. 11.2
(a, b) Lesion on the lower right lateral incisor masked with composite resin
Composite Resin Veneers
Composite resin can be used as a veneer to cover the entire labial aspect of the tooth and improve color and contour. These veneers can also protect against further breakdown of severely hypoplastic enamel as shown in Fig. 11.3a, b. Composite veneers may be directly placed at the chairside or indirectly fabricated in the laboratory. Composite veneering is conservative, cost-effective, and repairable in the mouth and may offer a satisfactory long-term alternative to full-coverage restoration in mild enamel defects even in adults. They are useful in the young dentition, in immature teeth with large pulp horns, large pulp chambers, immature gingival contour, and short crown height on teeth that are still erupting.
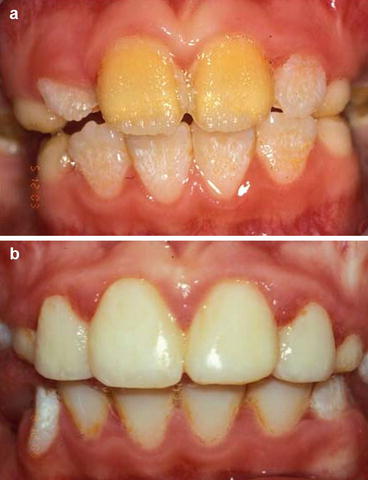
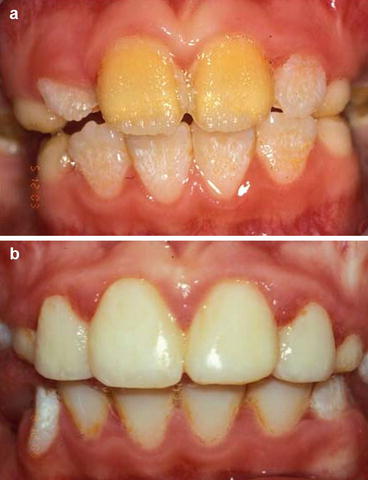
Fig. 11.3
(a, b) Resin veneers for upper incisors in the early mixed dentition period
Before proceeding with any veneering technique, it is necessary to decide whether to reduce the thickness of labial enamel. Increased labio-palatal bulk without tooth preparation makes it harder to maintain good oral hygiene. However, increase in the labial contour may enhance appearance of in-standing or rotated teeth. Bond strengths to enamel are increased when 200–300 μm of the surface enamel is removed, and the restoration will maintain the tooth contour. Some reduction and/or use of an opaquing agent may be required to mask intense stain in a discolored tooth. Hybrid composite resins finished to a higher surface luster can replace relatively large amounts of missing tooth tissue or may be used in thin sections. Layering of dentine and enamel shades can be used to simulate natural color gradations and hues.
Indications
-
Large demarcated enamel opacities
-
Widespread hypoplastic enamel defects
Contraindications
-
Very darkly discolored teeth
-
Minimal enamel defects
-
Insufficient tooth tissue available for bonding
-
Oral habits, e.g., woodwind musicians where embrasure may be critical
-
Heavy occlusal load/parafunction
Technique: Direct Composite Veneers
-
Use a tapered diamond or sharp tungsten carbide bur to reduce labial enamel by 0.3–0.5 mm if required. Identify a finish line at the gingival margin and extend mesially and distally just labial to the contact points.
-
Clean with a slurry of pumice in water, wash, and dry to remove plaque and debris.
-
Isolate the tooth with dam and a contoured matrix strip if needed.
-
Etch enamel, wash, and dry. Apply a thin layer of primer and bond with a brush and use an opaquing agent at this stage if discoloration is intense.
-
Apply composite resin and shape. Light cure according to manufacturer’s instructions at the gingival margin and the mesio-incisal, disto-incisal, and palatal aspects if incisal coverage has been used. Different shades can be combined to achieve matches with adjacent teeth and transition from a relatively darker gingival area to a lighter more translucent incisal region.
-
Finish the margins with diamond finishing burs and interproximal strips and the labial surface with graded finishing discs.
-
Take postoperative photographs for records.
Outcome
Good esthetics can be maintained for many years with regular reviews and repolishing as needed [28]. Indirect composite veneers can be fabricated from elastomeric impressions of the teeth, direct scanning of the prepared tooth or indirect scanning of a stone working cast. Laboratory-fabricated composite veneers can provide many of the characteristics of a ceramic veneer as described below. Color reproduction and surface wear are improving. However, in a situation with high esthetic demand, porcelain would still be the material of choice for restoration longevity and stability.
Porcelain Veneers
Porcelain has superior esthetic properties to composite resin, improved resistance to abrasion, and is well tolerated by gingival tissues. However, porcelain requires tooth preparation to maximize fit and maintain tooth contour and to allow replication of color. Disadvantages are that it is not repairable in the mouth and the laboratory stages add to cost when compared to directly placed restorations. Best outcomes are obtained after teeth have erupted completely, and therefore these restorations should generally be delayed until late adolescence (ideally after 20 years of age). Further information about preparation and design are covered in prosthodontic textbooks.
Restorative Management of Enamel Defects in Posterior Teeth
Clinicians face challenges when attempting to cover posterior teeth that are partially erupted, have significant sensitivity, suffer post-eruptive breakdown, or are difficult to anesthetize. Recommendations for managing sensitivity are included in Chap. 9. Where it is not appropriate to seal enamel because of the degree of hypomineralization, longer-term solutions are required.
Planning and Trialing the Occlusal Scheme
Patients with isolated teeth affected by enamel defects may have stable intra- (tooth to tooth) and inter-arch (maxilla to mandible) contacts, and acceptable arch alignment and length that provide a functional occlusion. Restorative management can be undertaken while conforming to the existing occlusal scheme. Where there is significant hypoplasia of the occlusal surfaces of molars and premolars, the teeth may not erupt into contact or the occlusal contacts that are formed may be on unstable inclined planes that predispose to tooth movement and tooth chipping. Specific malocclusions are associated with some types of AI including anterior open bite, delayed eruption, and/or missing teeth [29
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


