Injuries to the face, head, and neck are relatively common, but in the overall trauma literature, the etiology of maxillofacial injuries has received relatively little attention. Almost all injuries result from some form of trauma, which may be defined as a physical force resulting in injury. Injuries may also be the result of chemical, thermal, or even radiation trauma, but these occur far less commonly than physical trauma.
Despite the high incidence of facial injuries, there has been relatively little research until recently into their etiology, treatment, and prognosis. Nevertheless, such injuries are clinically important for several reasons:
- •
The soft tissues and bones of the face give anterior protection to the cranium.
- •
Facial appearance is a major factor, if not the most significant factor, in appearance and perception of self.
- •
The whole anatomic region is associated with several important functions of daily life, including sight, smell, eating, breathing, and talking. Significant impairment in any of these functions has potentially serious effects on the patient’s lifestyle and quality of life.
Trauma has traditionally been classified according to anatomic site. Although this is a logical approach on which to base treatment, in terms of developing strategies to prevent injury it is more informative to consider the etiology and the applied forces that produce injuries of differing types. Patterns of injury can be described that relate to certain types of accidents, and it is important to understand these patterns in relation to forensic evidence. In addition, strategies to reduce the incidence of maxillofacial injuries need to be developed, because the cost of treatment of these injuries can be high.
The reaction of the body to trauma depends on the nature of the assault and the response of the victim. The applied force and the extent of injury after trauma are affected by several factors. The kinetic energy (or potential to inflict damage) is calculated as one half of the mass of the object striking the face or head multiplied by the velocity squared; this is usually represented by the formula, K = ![]() MV 2 . Sometimes the situation is the opposite, and the momentum is generated by movement of the head striking a static object (e.g., in a fall). In all cases, it is the velocity rather than the mass of an object that has the greater proportional effect because of the kinetic energy generated. This is clearly demonstrable in road traffic accidents (RTAs): The severity of injuries associated with collisions at speeds greater than 20 mph (32 kph) is disproportionately increased compared with injuries sustained at lower speeds, and the risk of serious or fatal injury is much greater. The same principle applies to ballistic injuries: Although rifle or gunshot injuries may appear to be more damaging, they are seldom as severe as injuries caused by high-velocity bullets.
MV 2 . Sometimes the situation is the opposite, and the momentum is generated by movement of the head striking a static object (e.g., in a fall). In all cases, it is the velocity rather than the mass of an object that has the greater proportional effect because of the kinetic energy generated. This is clearly demonstrable in road traffic accidents (RTAs): The severity of injuries associated with collisions at speeds greater than 20 mph (32 kph) is disproportionately increased compared with injuries sustained at lower speeds, and the risk of serious or fatal injury is much greater. The same principle applies to ballistic injuries: Although rifle or gunshot injuries may appear to be more damaging, they are seldom as severe as injuries caused by high-velocity bullets.
In most cases, the applied force is predetermined, but there are four other variables that affect the type and severity of injury sustained:
- •
The position of impact—the anatomic region to which the force is applied
- •
The area of impact—the wider the area, the greater the dissipation of force (given that pressure equals force per unit area)
- •
The resistance—whether there is any movement of the head or the soft tissues, or whether there is contact with bone; any restriction of movement potentially increases the severity of injury
- •
The angulation of the strike—a glancing blow causes a less serious injury
The strength of the soft tissues and underlying bone also plays a part in the extent of any injury, but there has been little work to assess susceptibility to injury in those terms.
Classification of Facial Trauma
The classification of maxillofacial trauma should be related to outcome (i.e., type of injury sustained) to be valuable in audit of outcomes. It can also be considered with respect to etiology under a variety of headings, including assaults, falls, industrial injuries, RTAs, animal bites, sports injuries, burns, and war injuries. Other categories could also be included, such as iatrogenic and self-inflicted injuries. In all published studies, industrial injuries have represented only a small percentage of the overall total, although such injuries may be underreported. Many of these injuries are the result of falls at work, but equipment breakages and malfunctions also account for a significant proportion.
Several difficulties exist in comparing published reports because of variations in data collection and classification of injuries. Soft tissue injuries, nasal bone fractures, dental injuries, and dentoalveolar fractures are presented in different ways by different centers, and in some studies, they are completely omitted. True comparison of published studies is also made difficult by the use of different selection criteria and the frequent reporting of retrospective, poorly collected data (which are commonly restricted to either causes or types of injury). Even so, the existing data have been useful in helping to promote changes in legislation and practice aimed at reducing the number and extent of maxillofacial injuries.
Attempts to standardize the recording of injury pattern and severity have been made. With respect to assessing the injury severity associated with maxillofacial trauma, a number of scales have been described. These have three important uses:
- •
They promote targeted care (e.g., the Glasgow Coma Scale ).
- •
They help to predict the likely outcome (e.g., the Abbreviated Injury Scale [AIS] and the Injury Severity Score [ISS] ).
- •
They encourage the accurate assessment and outcome of critically injured patients (e.g., Acute Physiology and Chronic Health Evaluation [APACHE II] Disease Classification System ).
It is well recognized that scoring systems are useful for determining the extent of maxillofacial trauma, but they do have a number of drawbacks. For example, whereas the International Classification of Diseases (ICD) describes diagnostic codes for most injuries, in practice the coding for patients with multiple craniofacial injuries may be complex, and data recovery almost certainly introduces bias in retrospective studies. There can be little doubt, therefore, that the prospective, systematic collection of data is always to be preferred in considering the etiology of facial injuries.
Assault
From a forensic viewpoint, assault can be defined as the perceived threat of an imminent attack. Any act of physical violence is legally referred to as battery. In medical parlance, the word assault has become synonymous with the act of violence itself.
The comparative study of the prevalence of maxillofacial trauma as a result of assault (battery) is not easy. This is again due to the fact that relatively few studies have considered consecutive, nonselective data in estimating the pattern of injuries sustained, the actual treatment delivered, or the resulting demand for services.
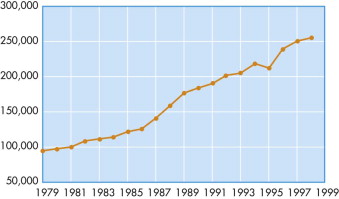
It is well accepted that there is an increasing incidence of maxillofacial trauma associated with the rise in interpersonal violence in much of Western society ( Fig. 1-1 ). In the developed world, there has been a pattern of increasing violence in urbanized settings since World War II, but in the developing nations, this pattern is less evident. With the increase in interpersonal violence in the developed world (coupled with improvements in road safety and car design), assaults are replacing RTAs as the most common etiologic factor in maxillofacial trauma ( Table 1-1 ); in the Third World, this is not yet the case. This trend has been observed in many countries, including the United States, United Kingdom, Scandinavia, Australia, and New Zealand. The pattern in many other societies is different, with RTAs often remaining the most common cause of maxillofacial trauma. In the Netherlands, RTAs still predominate because of the number of bicycle accidents that occur.
| Australia | New Zealand | Japan | Norway | United Kingdom | USA | India | Nigeria | Tanzania | |
|---|---|---|---|---|---|---|---|---|---|
| Assaults | 52 | 32 | 15.5 | 49 | 52 | 49 | 25 | 43 | 14.5 |
| RTAs | 19 | 30 | 38.5 | 14 | 16 | 43 | 40 | 27 | 81 |
| Sports | 16 | 20 | 16.5 | 8 | 19 | 4 | 4 | 9 | <2 |
| Falls | 10 | 9 | 28.5 | 15 | 11 | 3.5 | 24 | 18 | <2 |
| Industrial | 1.5 | — | 0.3 | 9 | 2 | 0.5 | 1.3 | 3 | 1 |
| Other | 1.5 | 9 | 0.7 | 4 | — | — | 1.2 | — | — |
When considering interpersonal violence, the frequency with which the face is involved in assaults was shown in one study to approach 50% of all reported cases. Approximately 40% of individuals who presented at emergency departments because of assault had facial injuries, and almost 30% of assault victims had fractures, 83% of which affected the facial skeleton. The rise in interpersonal violence has directly increased the trauma workload, particularly for oral and maxillofacial surgeons, and especially with regard to the more serious facial injuries.
With the exception of the sex of the assailant, which is usually male, the single most important etiologic factor in assault cases appears to be alcohol consumption (by both the assailant and the victim). Almost 50% of assault victims are found to have an increased blood alcohol concentration (>100 mg/dL), and alcohol abuse has been described as a contributing factor to assault in almost all independent studies. It is difficult to obtain accurate figures on the numbers of assailants who have consumed alcohol because so many escape. However, this information is widely reported, and the fact that so many assaults take place in or near locations where alcoholic beverages are supplied gives further confirmation to this hypothesis that alcohol consumption is an important factor in assault. In the British Association of Oral and Maxillofacial Surgeons’ survey of facial injuries (an intensive multicenter study), 55% of assaults were related to alcohol consumption, and 24% of the facial injuries recorded were caused by assaults. However, this study is still incomplete, and formal testing of all those involved was not possible.
The victims of trauma from assaults are most frequently young adult men in the 18- to 25-year-old age group, and they are most commonly assaulted by an unknown assailant. Those affected tend to be employed in manual labor, suggesting a possible causal link between social deprivation and aggression, but this has not been confirmed in other studies. Assaults leading to facial injuries typically occur in a bar or a public place near a bar and frequently late at night ; the effects of cumulative alcohol consumption compounded by tiredness have not been independently studied but may offer a simple explanation for this fact. The relationship between alcohol and assault was even clearer in a U.K. study which showed that, among those older than 15 years of age, alcohol consumption was associated with 90% of facial injuries occurring in bars, 45% of those occurring in the street, and 25% of those occurring in the home situation. Almost one quarter of all facial injuries in all age groups were related to consumption of alcohol within 4 hours of the injury.
Studies in large cities have shown that assaults often occur within a relatively limited geographic area and that they tend to be focused in areas adjacent to licensed premises. Assaults make up a slightly larger proportion of facial injuries seen in emergency departments in cities (26%) than in county towns (21%).
Whereas males are more commonly assaulted by unknown assailants, the converse is true of female victims. Typically, women are assaulted by a partner or ex-partner, and the assault occurs in or around the home. Moreover, a greater percentage of women are assaulted at home in county towns (52%) compared with cities (38%), and fewer females are assaulted in public bars in all environments.
The number of injuries caused by female assailants is small, but there is some evidence that it is growing. Again, alcohol appears to be the main factor in the etiology of such attacks.
The pattern of injury sustained depends largely on the implement used. Whereas studies of maxillofacial trauma have often considered bony injury in isolation, soft tissue lacerations are the most common maxillofacial injuries sustained. Despite their frequency, soft tissue injuries are often overlooked in trauma epidemiology. More than two thirds of the injuries sustained in assaults are lacerations; almost 40% of all assault victims and 95% of victims of domestic violence have facial lacerations. Soft tissue injuries are most frequently inflicted by direct, blunt trauma. Stab injuries to the face are uncommon, but the use of broken glass or blades was responsible for 11% of facial injuries in one study.
A number of studies have considered hard tissue injuries in isolation. Assault-related fractures most frequently involve (in order of descending frequency) the nasal bones, the mandible, the zygoma, and the midface. This contrasts with the pattern observed in RTAs, which cause injury principally to the midface (see later discussion).
The pattern of injury is affected greatly by the weapon selected. In the past, fists, feet, blunt instruments, and broken glass were commonly used. More recently, baseball bats and automatic and semiautomatic weapons have been more frequently used in premeditated assaults, principally in the United States, and this has had a considerable impact on the extent and pattern of injuries in some studies. Despite attempts to reduce the incidence of injuries due to assault (including education about alcohol consumption, introduction of drinking glasses made of toughened safety glass in licensed premises, increased policing, and improved street lighting), the available data suggest that maxillofacial trauma due to assaults and interpersonal violence will continue to increase for some time yet.
Medicolegal Description of Injuries
Bruises or Contusions
A bruise is the result of subcutaneous bleeding that occurs after an impact from a blunt object. Bruises may be seen adjacent to lacerations or abrasions, but they also frequently occur without rupture of the skin. The extent of any bruising is related to the severity of the impact, the laxity of the tissues, the individual’s propensity to bruising, and age (older people and children being most susceptible). Particular care needs to be taken in trying to correlate the severity of a blow with the extent of bruising, particularly in older patients and in those taking anticoagulants, who may have disproportionately excessive bruising.
Abrasions
An abrasion is a superficial wound that does not fully penetrate the dermis. The point at which an abrasion may be termed a laceration is not always easy to determine, because deeper abrasions frequently bleed (sometimes excessively) and therefore must have penetrated the dermis. This is especially apparent after an RTA in which the victim’s head skidded over a gravel surface.
Careful examination of abrasions often reveals a “heaping” of skin at the distal end of the impact area. This raised skin or small skin tags can indicate the direction of impact and therefore can be useful in helping to establish possible causes. Deeper wounds are often accompanied by foreign bodies—wood splinters, road dirt, paint specks, and the like—all of which can be used to provide forensic evidence. It is clearly good medical practice to clean wounds before repair or dressing, but few practitioners collect any debris removed from a wound, although this practice could be of considerable legal benefit.
Lacerations
A laceration is a full-thickness wound of the skin that is caused by compression of the skin against the bone with a blunt object. A blunt weapon such as a fist or a bat may have been used, or the head or other body part may have struck a blunt object (e.g., in a fall). There is no way of distinguishing the cause with certainty unless the wound contains foreign matter.
On occasion, it can be difficult to distinguish a laceration from an incision, although the former usually shows mild inversion of the wound edges on close examination—a feature not seen in wounds caused by sharp objects. Lacerations may bleed profusely, but they frequently do not because of retraction of the blood vessels that were compressed during the creation of the injury.
Incisions
An incision is a full-thickness skin wound that is caused by a sharp instrument. If the length of the wound exceeds its depth, it is referred to as a slash wound ; if the converse is true, it is a stab wound .
The clinical appearance of a slash wound is affected by the muscular pull and the crease lines of the skin. Such wounds may bleed profusely, and it is not always easy to identify and occlude vessels that have been cut. From a forensic point of view, it is not easy to glean much information from a slash wound, although the deeper end of the incision tends to be the origin. Ragged edges may suggest a blunter implement, but the actual type of implement used cannot be categorized with any certainty.
Although stab wounds to the face are less common than stab wounds to other sites, they yield more forensic information, and good close-up photographs of such wounds should be taken before suturing. Multiple stab wounds in the region of the neck should lead the clinician to consider a possible diagnosis of attempted suicide, although stabbing of other areas of the body (e.g., chest, wrists) is more common in such cases. The unpredictable direction of the stab may cause unpredictable severity to the wound.
Medicolegal Description of Injuries
Bruises or Contusions
A bruise is the result of subcutaneous bleeding that occurs after an impact from a blunt object. Bruises may be seen adjacent to lacerations or abrasions, but they also frequently occur without rupture of the skin. The extent of any bruising is related to the severity of the impact, the laxity of the tissues, the individual’s propensity to bruising, and age (older people and children being most susceptible). Particular care needs to be taken in trying to correlate the severity of a blow with the extent of bruising, particularly in older patients and in those taking anticoagulants, who may have disproportionately excessive bruising.
Abrasions
An abrasion is a superficial wound that does not fully penetrate the dermis. The point at which an abrasion may be termed a laceration is not always easy to determine, because deeper abrasions frequently bleed (sometimes excessively) and therefore must have penetrated the dermis. This is especially apparent after an RTA in which the victim’s head skidded over a gravel surface.
Careful examination of abrasions often reveals a “heaping” of skin at the distal end of the impact area. This raised skin or small skin tags can indicate the direction of impact and therefore can be useful in helping to establish possible causes. Deeper wounds are often accompanied by foreign bodies—wood splinters, road dirt, paint specks, and the like—all of which can be used to provide forensic evidence. It is clearly good medical practice to clean wounds before repair or dressing, but few practitioners collect any debris removed from a wound, although this practice could be of considerable legal benefit.
Lacerations
A laceration is a full-thickness wound of the skin that is caused by compression of the skin against the bone with a blunt object. A blunt weapon such as a fist or a bat may have been used, or the head or other body part may have struck a blunt object (e.g., in a fall). There is no way of distinguishing the cause with certainty unless the wound contains foreign matter.
On occasion, it can be difficult to distinguish a laceration from an incision, although the former usually shows mild inversion of the wound edges on close examination—a feature not seen in wounds caused by sharp objects. Lacerations may bleed profusely, but they frequently do not because of retraction of the blood vessels that were compressed during the creation of the injury.
Incisions
An incision is a full-thickness skin wound that is caused by a sharp instrument. If the length of the wound exceeds its depth, it is referred to as a slash wound ; if the converse is true, it is a stab wound .
The clinical appearance of a slash wound is affected by the muscular pull and the crease lines of the skin. Such wounds may bleed profusely, and it is not always easy to identify and occlude vessels that have been cut. From a forensic point of view, it is not easy to glean much information from a slash wound, although the deeper end of the incision tends to be the origin. Ragged edges may suggest a blunter implement, but the actual type of implement used cannot be categorized with any certainty.
Although stab wounds to the face are less common than stab wounds to other sites, they yield more forensic information, and good close-up photographs of such wounds should be taken before suturing. Multiple stab wounds in the region of the neck should lead the clinician to consider a possible diagnosis of attempted suicide, although stabbing of other areas of the body (e.g., chest, wrists) is more common in such cases. The unpredictable direction of the stab may cause unpredictable severity to the wound.
Road Traffic Accidents
Motor Vehicle Accidents
RTAs are a major health problem. In the United States alone, they account for an estimated 50,000 deaths and more than 3 million injuries annually. Although RTAs are frequently associated with severe maxillofacial injuries, most of these injuries are facial lacerations. In Western countries, the highest rate of maxillofacial trauma in many studies occurred during the 15 years following World War II (see Table 1-1 ). In the developing world, RTAs still account for the majority of maxillofacial trauma, but the introduction of seat-belt and drunk-driving legislation and improvements in car design (discussed later) have greatly decreased the incidence of fatalities and RTA-associated maxillofacial trauma. This serves to illustrate not only the progress of car design but also the benefits of the detailed study of facial trauma. The most important factor in determining the extent of injuries sustained in RTAs is the direction of the collision; for example, drivers involved in head-on collisions are 18% more likely to survive.
In the past 30 years, modern car designers have developed an impressive array of safety features to reduce the risk of serious injury in RTAs ( Fig. 1-2 ). Some of these are principally improvements in the design features of the car, such as crumple zones, collapsing steering wheels, and side-impact bars. Others have involved the development of new technologies (often adopted from the aviation industry), including improved seat restraints, laminated windshields, air bags, computerized warning systems, and antilock and assisted braking systems. Improvements have also been made to the environment, such as enhanced road design, better signposting and lighting, rumble strips, and bright “cats’ eyes.” Recent innovations have included car designs that minimize injuries to pedestrians or cyclists struck by vehicles.

External Support Devices
Supportive and protective devices play a major role in preventing facial injuries and significantly reducing the magnitude of the facial damage. They can be divided into protective devices that are installed as part of a vehicle or sporting equipment and those devices that are carried or worn by the individual.
The decrease in maxillofacial trauma associated with RTAs has been dramatic. In the United Kingdom, car ownership has increased rapidly in the past 20 years, but the total incidence of facial fractures associated with RTAs has decreased by one third. Most encouragingly, the percentage of all facial fractures associated with RTAs has decreased from 46.8% in 1948 to 18.6% over the same period. The severity of injuries has also decreased: 54% of RTA-associated midfacial injuries were at Le Fort II or III levels in 1948-1955, compared with 8.6% in 1987-1993. These dramatic improvements occurred after the introduction of drunk-driving legislation in the 1970s and compulsory seat-belt wearing in 1983: The incidence of facial injuries in patients involved in RTAs was reduced from 21% to 6% in less than 2 years.
Similar findings have been noted in several other countries. However, Tanaka and colleages reported that seat-belt legislation in Japan did not make a great difference in the pattern of facial injuries, whereas Imai and co-workers concluded that the number of midfacial fractures was significantly reduced. It is difficult to postulate why these findings differed and whether the perceived lack of improvement may have been related to poor compliance or to an already low incidence of such injuries.
Compliance with seat-belt legislation is another area in which there is considerable national variation. Despite the proven benefits of seat belts, almost 70% of individuals involved in RTAs were not using any form of restraint. Particularly alarming was a study of pediatric RTA-related facial trauma in the United States, which demonstrated that only 138 of 412 children with facial trauma were restrained at the time of impact.
Seat Belts and Lap Belts
Seat belts work in three different ways. Perhaps most obvious is the restraint of the person within the vehicle, which prevents their expulsion through the windshield. Seat belts also spread the area over which the energy of impact is dissipated. Finally, seat belts are made of a fabric that has a slight degree of elasticity; this increases the time during which the energy of impact is dissipated.
The current three-point combination lap and diagonal belt positioned across the pelvis and the rib cage was developed by a Swedish aircraft engineer and was introduced in 1959. It provides a strong three-point harness with a simple pendulum and ratchet mechanism that locks the belt in sudden-stop situations. The lap belt spreads crash forces across the strong pelvic bone and keeps the passenger from being tossed around inside the car, whereas the shoulder harness spreads forces across the rib cage and prevents the upper body from jack-knifing forward. In the United States, this three-point system has been mandatory in automobiles since 1974 and saves thousands of lives each year.
It is universally accepted that the use of seat belts and lap belts is associated with a lower risk of serious injury, particularly to the head and face ( Fig. 1-3 ). The difference in injury rate is so significant that the use of these devices is mandated by law in all parts of the United States and the United Kingdom, and violations are punishable by monetary fines. Despite these recognized safety facts, seat belts and lap belts frequently are not used (e.g., by up to 33% of front seat occupants), and the results are manifested in trauma registry records.

For children, the rate of restraint use is better (78%), according to the latest National Pediatric Trauma Registry information from 92 centers reporting throughout the United States. This probably reflects the effects of pediatric education campaigns and the legal requirement for use of restraints in children up to the age of 4 years or 40 lb in weight ( Fig. 1-4 ).

Despite the craniofacial protection provided by seat belts and lap belts, severe systemic injuries still do occur in belted individuals. Certain specific injuries occur with belt use, including cervical, lumbar, and intra-abdominal injuries; this has been referred to as seat-belt syndrome . However, critical analysis suggests that, with the exception of sternal fractures, injuries previously associated with seat-belt syndrome occur in similar proportions in belted and unbelted patients.
Air Bags
Like seat belts and lap belts, the air bag has proved to be effective in reducing injuries and fatalities in motor vehicle accidents. They work best for belted drivers, reducing fatalities by more than 50%. With unbelted drivers, fatalities are reduced by up to one third, and facial injuries are decreased due to the prevention of direct facial impact onto the steering wheel, dashboard, or seat ( Fig. 1-5 ). Of all automotive safety devices, air bags probably provide the single best protection for the driver, preventing lacerations and facial fractures. Among passengers, air bags have been reported to reduce the incidence of facial lacerations but not that of fractures.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



