

Treatment of enamel lesions and management of color changes and discolorations
Discolored primary teeth can be yellowish, reddish, brown, grey, green, blue, or black. These discolorations may be due to intrinsic or extrinsic factors. Extrinsic staining can be commonly caused by many agents such as multivitamins, iron supplements, and many food items with high pigment content. Such staining is easily treated by coronal scaling and polishing the teeth with a medium grade prophylaxis paste that removes stubborn stains from tooth enamel in both primary and permanent dentition. In younger pre-cooperative children, such treatment can be achieved by a practitioner experienced in the knee to knee position.21
An intrinsically discolored primary incisor most often indicates that the tooth has sustained pulpal injury.22 Dark discoloration of the primary incisor may be an indication of the release of red blood cells from a ruptured pulpal blood vessel into the dentin. Such discoloration may resolve, persist, or worsen depending on the extent of the pulpal injury. The determination of the prognoses of these teeth is challenging. Clinical and radiographic evaluation at 4 weeks, 6 to 8 weeks, and 1 year from the time of initial occurrence and diagnosis is advised.23 An isolated yellow tooth may also be associated with a history of trauma that has resulted in dentinal calcific deposition within the dentin. This calcific degeneration or metamorphosis of the pulp can be confirmed radiographically by the presence of a calcified pulp chamber. Enamel and or dentin dysplasia explain the more generalized irregularities in the surface of the enamel and or underlying dentin causing discoloration in both primary and permanent dentition. These may be caused by a specific etiology such as ingestion of tetracycline during the development of the anterior teeth (generally up to 7 years of age), or they may be multifactorial, ranging from suboptimal or excessive fluoride exposure to other environmental, developmental, and genetic disorders24–27 Molar-incisor hypomineralization (MIH) is yet another developmental condition resulting in enamel defects in first permanent molars and permanent incisors, with no currently known etiologic mechanism.28
Most of the resulting esthetic defects from intrinsic factors and superficial staining resistant to scaling and polishing can be treated with a conservative composite resin veneer technique. Beyond these approaches, bleaching and acid application with mechanical abrasion (microabrasion) and resin infiltration therapy are three other modalities utilized for esthetic treatment of affected anterior teeth (see Chapter 12). These techniques along with a more detailed etiology of the associated lesions are described in Chapter 13. Although bleaching in primary and young permanent teeth may be an option and has been reported in the literature for both selected situations of extrinsic and intrinsic staining, such approaches await long-term studies in children.29–33 Currently there are no bleaching products in the marketplace that have the ADA’s Seal of Acceptance for use in children, and practitioners are encouraged to consider side effects when contemplating dental bleaching for child and adolescent patients.34, 35
Recently a new remineralizing agent based on Casein Phosphopeptide-Amorphous Calcium Phosphate (CPP-ACP) (MI Paste, GC America Inc.) has been developed. CPP-ACP stabilizes high concentrations of calcium and phosphate ions that bind to pellicle and plaque. When teeth are under acid challenge, this reservoir of ions maintains a supersaturated mineral environment, reduces demineralization, and enhances remineralization of enamel. According to in vitro studies, CPP-ACP supplementation has the potential to be effective in remineralization of the enamel affected by MIH and to result in an aesthetic improvement. This is a therapeutic agent that is particularly promising in the treatment of MIH in conjunction with treatments mentioned thus far and traditional restorative care. The use of CPP-ACP does require a long-term treatment plan that could last months or years, requiring optimal patient cooperation.36
Anterior composite resin restorations in primary teeth
Dentin/enamel adhesives allow bonding of resin-based composites and compomers to primary and permanent teeth. (See Chapters 3-5 for the treatment of permanent teeth with bonded restorations). Adhesives have been developed with reported dentin bond strengths exceeding that of enamel. In vitro studies have shown that enamel and dentin bond strength is similar for primary and permanent teeth. The clinical success of adhesives allows for more conservative preparation when using composite restorative materials. Adhesive systems currently follow either a “total-etch” or a “self-etch” technique. The total etch technique requires 3 steps. It involves use of an etchant to prepare the enamel while opening the dentinal tubules, removing the smear layer, and decalcifying the dentin. After rinsing the etchant, a primer is applied that penetrates the dentin, preparing it for the bonding agent. The enamel can be dried before placing the primer, but the dentin should remain moist. A bonding agent then is applied to the primed dentin. A simplified adhesive system that combines the primer and the adhesive is available. Because the adhesive systems require multiple steps, errors in any step can affect clinical success. Attention to proper technique for the specific adhesive system is critical to success.
Bisphenol A (BPA) is widely used in the manufacturing of many consumer plastic products and can become part of dental sealants and composites in three ways: as a direct ingredient, as a by-product of other ingredients in dental sealants and composites that may have degraded (e.g., bisphenol A glycidyl methacrylate [bis-GMA] and bisphenol A dimethacrylate [bisDMA]), and as a trace material left over from the manufacturing of other ingredients used in dental sealants and composites. The most significant window of potential exposure to BPA is immediately following the application of resin-based dental sealants and composites. Based on current evidence, the US Food and Drug Administration and the American Dental Association (ADA) do not believe there is a basis for health concerns relative to BPA exposure from any dental material and have concluded that any low-level of BPA exposure that may result from dental sealants and/or composites poses no known health threat.
Measures can be taken to reduce potential BPA exposure from dental materials. A precautionary application technique recommended is removal of residual monomer by rubbing the monomer layer with pumice on a cotton roll or having the patient gargle for 30 seconds and spit immediately after application of the dental sealant or composite. Because rinsing and spitting can be challenging for many children, thorough rinsing with an air-water syringe may be a suitable substitute. As with all dental operative procedures, use of a rubber dam to control the operative field would further limit potential exposures.37,38
Isolation technique
Composite resin is extremely technique sensitive and appropriate isolation technique must be used.39 Rubber dam isolation has been the traditionally used technique for ideal isolation. The use of ligature ties with dental floss to retract the gingival tissue has been shown to improve rubber dam effectiveness.40 Gingivectomy with electrosurgery is a less commonly used alternative. Isolite Systems (Fig. 19-2) is a fiber optic and evacuation device with age appropriate sized disposable mouthpieces that is easily administered with no need for anesthesia of the clamped tooth as is the case for rubber dam isolation. This device is well tolerated by most children and serves as bite block and cheek retractor and isolates the maxillary and mandibular arches well beyond the midline of the side of the mouth in which it is placed. It also provides continual evacuation of fluid and salivary flow, protection of adjacent soft tissues, and assistance in opening the mouth.

Composite resin veneer
Armamentarium
• Standard dental setup, basic composite resin restorative tray with nonstick composite resin placement instrument (e.g., Cosmedent, Inc.), high- and low-speed dental handpieces
• Acid-etch gel (see Chapter 3)
• Bonding agent of choice (see Chapter 3)
• Composite resin of choice (see Chapter 5)
• Isolation set up with Rubber dam (e.g., Hygenic Flexi Dam Rubber Dam Coltene/Whaledent. Inc) or other dental isolation system (e.g., Isolite Isolite Systems)
• Diamond flame bur—Medium (862) to Coarse (6862) (Peter Brasseler Series, Brasseler USA)
• Mylar clear strips and Cure-Through Wedge Wands (Garrison Dental Solutions)
• White Store Flame Finishing Bur & CompoSite Polishing Kit (Shofu Dental Corp.)
Clinical technique
1. Isolate the teeth using a rubber dam or Isolite.
2. Remove a 0.5-mm layer of enamel from the facial portion of the teeth, etch, rinse, dry, and apply bonding agent.
3. Apply a clear Mylar matrix to the teeth being treated and secure with a finger or a palatally placed wedge.
4. Apply a layer of composite resin (microfilled) and a buildup to cover the discolored tooth.
5. Light cure, finish, and polish to ideal esthetics.
6. Thoroughly rinse the restoration with an air-water syringe for 30 seconds.
Composite resin restorations (Class III, Class IV, Class V)
The age of a child will not only influence the ability to cooperate with procedures such as rubber dam application and local anesthesia, but the patient’s age will also dictate for how long a restoration is required to remain in the mouth. The morphology of the primary anterior dentition is unique in that the actual dimensions of the primary incisors offer little tooth structure for an effective long-term interproximal restoration (Table 19-2). Class III lesions in the primary dentition may best be treated with full coverage crowns, particularly when they are treatment planned in younger children who both are less likely to be fully cooperative and who require a longer period of service from the restoration. Restoration of primary incisors with interproximal caries requires an exacting technique. Prudent evaluation of both the tooth to be restored and the child’s ability to cooperate is imperative for successful treatment planning. The lesions should be small compared with the total tooth size. A lock may be placed with generous beveling of the facial or lingual portions of the preparation, rather than in the proximal internal walls where a danger of pulp exposure exists. The small size of the mandibular incisors makes it almost impossible to use this procedure without exposing the pulp, and full coverage composite resin strip crowns (see section on Resin-Bonded Composite Strip Crowns later) are often a more prudent esthetic treatment option. Stripping of interproximal enamel may be used occasionally for minimal caries in the anterior lower primary teeth. Opening of the contact points with a thin diamond bur allows saliva and fluoride to slow and possibly arrest the carious process, even when the caries involves the dentine. This is often, however, a less esthetic alternative that may be provided until the child is more cooperative and or until pharmacological behavior management options can be used.41
Table 19-2
Average Sizes of Primary Teeth
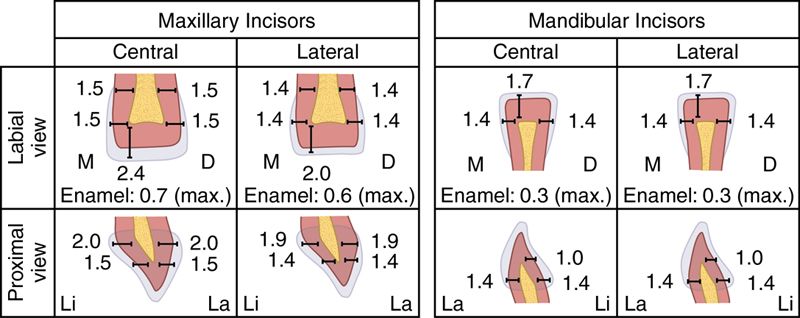
Modified from McBride WC: Juvenile dentistry, ed 4, Philadelphia, 1945, Lea & Febiger.
Armamentarium
Clinical technique
1. Apply topical and local anesthesia.
2. Place a rubber dam or Isolite.
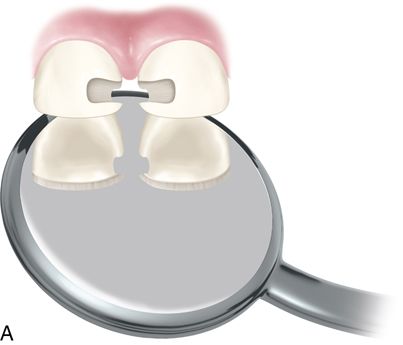
3. Remove interproximal caries with a pear-shaped bur #330 and round bur (Fig. 19-3 A). A bevel can be placed if desired.
4. Remove the incisal angle if it is thin and undermined. If both mesial and distal caries exist and/or a mechanical pulp exposure occurs, it is best to prepare the tooth for a full coverage strip crown. In the case of a mechanical pulp exposure, perform a vital pulpotomy. Direct pulp capping in primary teeth is generally contraindicated. (See the section on pulpotomy of vital primary teeth in this chapter.)
5. Place a liner of glass ionomer cement on the dentin. If a pulpotomy or pulpectomy is performed, place glass ionomer cement over the zinc oxide and eugenol, which was placed during the pulpotomy procedure.
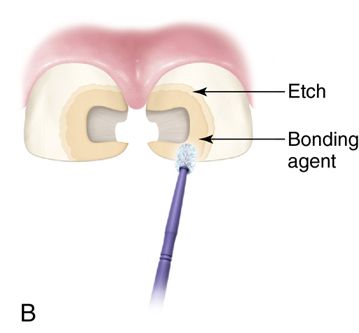
6. Acid etch the enamel for 30 to 45 seconds, rinse, and dry.
7. Apply bonding agent (Fig. 19-3 B).
8. Depending on the restorative situation
A. If the dental arch exhibits interdental space between the anterior teeth, place a bonded composite resin (Fig. 19-3 C).
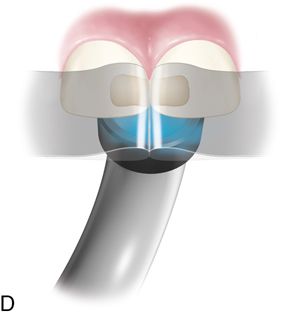
B. If no interdental space exists, place a wedge (if possible) and a mylar strip to aid in shaping the composite resin (Fig. 19-3 D).
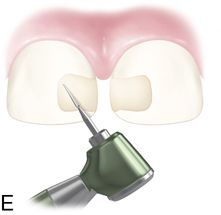
9. Light cure from the lingual (see Fig. 19-3 D) and facial direction. Then, finish and polish the restoration (Fig. 19-3 E).
10. Thoroughly rinse the restoration with an air-water syringe for 30 seconds.

Intracoronal esthetic restorations of posterior primary teeth
The demand for esthetic restorations in children is no longer limited to the anterior zone. Posterior esthetic options increasingly expected by patients and their parents. A 2009 study in the United States found that esthetics was the main parental concern about dental material.47, 48
Since the introduction of posterior esthetic options, the restoration of primary teeth with tooth colored materials has been increasing. Studies shows that composite resin is now the most frequently used restorative material for restoration of class I and class II restoration in some regions.47 The number of esthetic options is now wider than ever. Although amalgam continues to be deemed an acceptable and safe restorative material for children, glass ionomers, resin-modified glass ionomers, and composite resins have allowed for reliable esthetic treatment in the posterior region. Despite the scientific evidence, many areas in the world have experienced a decline in the use of amalgam in children, mostly because of more stringent environmental regulations and worries about mercury exposure.42, 43 In Scandinavia, Germany, and Japan amalgam is now seldom used in children.
When multisurface carious lesions are present, a full coverage restoration such as a stainless steel crown has been shown to have better long term survival rates44 and continues to be the most commonly used full coverage restoration for posterior primary teeth. However, these are an unesthetic option and parents often prefer a tooth-colored crown (see full coverage esthetic options in the preceding sections).
Posterior composite resins and compomer restorations (see Chapter 5) allow for almost perfect biomimesis in the posterior primary and permanent dentition for class I, small class II, class V and class VI carious lesions. However, in patients with high caries risk, multi-surface composite resin restorations are not indicated. Typically, a child requiring full-mouth rehabilitation under general anesthesia should receive full coverage restorations42, 45 unless the carious lesions being treated are very small. Multi-surface composite resin restorations can be successful but should be used with caution, especially in patient with higher risk for caries and patients who demonstrate signs of bruxism or erosion. Bonded restorations to primary enamel and dentin present some unique challenges. Because the size of the preparations is smaller than that for permanent teeth, the bonded area is smaller. A lack of cooperation may complicate proper isolation. A conservative slot preparation has been advocated for class II restorations,46 and this has become the most frequently used design by some pediatric dentists. No studies have shown better survival for a traditional class II preparation (with a dovetail) versus a conservative slot preparation (no dovetail). Clinicians should maintain a good ratio between the occlusal load and the bonded area. A restoration that receives a high occlusal load but has minimal bonded enamel is at a higher risk of dislodging. Because the size of the ideal preparations are rather small, these preparations can be bulk filled.47 Some clinicians have advocated using a layer of flowable composite resin followed by regular composite resin to achieve better adaptation.
Posterior glass ionomer and resin-modified glass ionomer restorations
Glass ionomers and resin-modified glass ionomers are unique among dental materials because they release fluoride and physically and chemically bond to tooth structure with no need for etch and prime. However, nonmodified glass ionomers are brittle and have a tendency to wear. They are indicated for class I restorations but not ideal for definitive class II restorations of primary teeth because they have been shown to fail at a higher rate than other restorative materials.48 Conventional glass ionomers are especially indicated for atraumatic restorative treatment or IRT intermediate restorative treatment wherein partial caries removal is followed by restoration with a fluoride-releasing material in a non-cooperative or precooperative child.
Whereas traditional glass ionomer cements were opaque, newer resin-modified glass ionomers have attained a much better esthetic match to dentin and enamel. In clinical studies, resin-modified glass ionomers have greater longevity than conventional glass ionomers for class II restorations.49 These restorations do not provide ideal esthetics and are not discussed in this chapter.
Resin-bonded composite strip crowns
Resin-bonded composite strip crowns are among the most esthetically desirable anterior restorations for primary teeth, but they are also among the most technique sensitive procedures. These are clear celluloid plastic empty crown forms (3M ESPE or Nowak Pediatric Strip Crowns, Nowak Dental Supplies, Inc.) that the clinician sizes appropriately and then fills with resin-bonded composite and bonds to the prepared tooth. With crowding of the anterior teeth, and/or hemorrhage or poor salivary control, it is quite challenging to perform a direct composite resin restoration. These crowns are also more susceptible to loss and fracture when compared with stainless steel crowns. Patients with edge to edge occlusion and moderate to severe bruxism are poor candidates for restorations with these crowns.50
There should be sufficient incisal reduction (about 1.5 mm) to avoid incisal fracture. In the preferred design, more reduction on the facial surface is required. On the lingual surface there is often minimal reduction (about 0.5 mm) and a featheredged gingival margin.
Armamentarium
Clinical technique
1. Local anesthesia and rubber dam or Isolite isolation
2. Select the correct celluloid crown form depending on the mesiodistal width of the teeth.
3. Remove the caries using high-speed #330 carbide and slow-speed round bur.
4. Using a high-speed tapered diamond or tungsten carbide bur, reduce the incisal height by approximately 1.5 to 2 mm and prepare interproximal slices.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


