In the mid 1990s a new category of processed composite resin was introduced. Polymer-glass, polymer-ceramic, and cercomer (ceramic-optimized polymer) are all terms used to describe these materials. In reality, they are all composite resins with improved properties. Several systems also have incorporated fiber reinforcement to allow fabrication of metal-free fixed partial dentures.
Premise indirect
Premise Indirect (Kerr Corp.) dual cure indirect polymer-ceramic is a low-wear, high-strength microhybrid for inlays, onlays, anterior veneers, implants, full coverage crowns, metal-free fixed partial dentures, long-term provisional restorations, or splints. The opalescence of Premise Indirect is reported to achieve optimal shade matching capabilities. Trimodal curing (light, heat, and pressure) achieves over 98% material conversion as compared to 60% to 70% achieved with light-cure only materials. The material is a combination of large prepolymerized filler particles, 0.4 micron structural filler, and small silica nanoparticles that allow higher filler loading, improved physical properties, optimized handling, higher surface gloss, and reduced polymerization shrinkage. The coefficient of thermal expansion is similar to natural dentin and the wear rate over a 5 year period was similar to that of tooth structure. A reinforcing fiber material of woven polyethylene braids coated with a reactive monomeric solution that allows the product (Connect, Kerr Corp.) to be bonded to a resin based crown and fixed partial denture substructure by the application of heat is recommended for use in metal-free fixed partial dentures made with Premise Indirect.
Sinfony
Sinfony (3M ESPE), an ultrafine particle composite resin (or ultrafine particle hybrid composite resin) contains two kinds of filler: macrofiller (strontium aluminum borosilicate glass with a mean particle diameter of 0.5 to 0.7 μm; 40% by wt.) and microfiller (pyrogenic silica; 5% by wt.), which can flow into the gaps between the macrofiller particles. The Sinfony monomer system contains no Bis-GMA or TEGDMA. It is used as an indirect laboratory composite resin that combines strength, beauty, and versatility. Indirect restorations created from Sinfony indirect laboratory composite resin offer excellent esthetics, translucency, natural vitality, amber opalescent effect, and fluorescence. Composite resin is excellent for inlays/onlays, veneers, and full crowns. A completely new feature is the addition of a special glass ionomer (5% by wt.), which influences the surface potential of Sinfony so that plaque accumulation is minimized. At the same time this additive does not change the other favorable composite resin properties including color and acid stability.
GC gradia (GC America)
GC Gradia (GC America Inc.) is a light-cured high strength microhybrid (Microfill reinforced composite [MFR] formulation) that can be used for inlays/onlays, veneers. and crowns. GC Gradia couples a microfine ceramic/prepolymer filler with a urethane dimethacrylate matrix to produce a superior ceramic composite resin with exceptionally high strength, wear resistance, and superior polishability. GRADIA is biocompatible and kind to opposing teeth with excellent polishability, high wear resistance, but kind to the opposing dentition. The Foundation Opaque and Opaque shades can be used to mask discoloration effectively. Polymerization doesn’t affect color so that the lab technician can visualize the definitive restoration. The system consists of a variety of opaques, intensive colors, enamel shades and translucent materials so that the restorations can be built up like porcelain. In addition to tooth colored composite resins, GC Gradia Gum provides a variety of natural gingival shades with good adaptation to the GC Gradia composite resin system. It is also a microfilled composite resin with high strength and wear resistance. Oxygen also plays an important role in the apparent translucency or opacity of the polymerized resin restoration. Oxygen also plays an important role in the apparent translucency or opacity of the polymerized resin restoration. Removing all of the air causes the restoration to become considerably more translucent.
TESCERA ATL
TESCERA ATL (Bisco, Inc.) is a dual-cured microhybrid composite resin that is provided in every Classic Vita shade. The incremental layers are condensed with pressure and then polymerized to prevent delamination and keep the restoration free of voids. Final polymerization occurs in an oxygen-free environment to achieve a high-gloss–free surface to reduce staining. Tescera Opaceous Dentin composite resins emulate the most dense and most opaque area of the tooth; it will also reflect light resulting in optimal aesthetics. Tescera Opaceous Dentin composite resins emulate the most dense and most opaque area of the tooth; it will also reflect light resulting in optimal aesthetics. TESCERA U-BEAM is a U-shaped, unidirectional, prestressed, quartz fiber reinforced beam for fixed partial dentures. It is resistant to twisting and flexing because of its I-beam effect.
Rods: Unidirectional, pretensed quartz fiber reinforcement bars are used for posterior and anterior fixed partial dentures
Signum heraeus kulzer
Signum ceramic is a glass-ceramic composite resin with microfine filler particles, which was specifically developed for the requirements of metal-free restorations; its particularly high intrinsic durability (E-modulus) makes the restoration more durable, even if high levels of stress are encountered.
Ceramage shofu
Ceramage is a zirconium silicate integrated indirect restorative for both anterior and posterior regions. A progressive fine structure filling of more than 73% plus an organic polymer matrix delivers superior flexural strength, elasticity, and excellent polishability. It has flexural and compressive strength beyond 140 MPa, excellent abrasion resistance of opposing dentition, transmission and diffusion of light with a refractive index similar to natural teeth, and superior color stability over 5 years.
Anterior composite resin laminate veneers
Many composite resins wear much like natural tooth structure and do not cause iatrogenic wear of the opposing dentition. Indirect composite resin laminate veneers are the treatment of choice in many situations:
• Darkly stained teeth. Indirect composite resin can cover dark color without opaquing agents while retaining a vital appearance.
• Conservation of tooth structure. Tooth preparation for composite resin laminate veneers can be more conservative than that for porcelain alternatives because composite resin does not require 0.5 mm thickness, as does porcelain. Composite resin can be much thinner in spots and still function well.
• Fabrication alternatives. Indirect composite resin laminate veneers can be fabricated either in the office or in the dental laboratory. They can be polymerized or processed. They can be made of microfilled, small particle, or hybrid composite resin. The glass in the small particle or hybrid composite resin can be etched with hydrofluoric acid, which provides micromechanical retention rivaling that of etched porcelain.
• Chairside repairs. These restorations can be repaired at the chairside with light-cured composite resins.
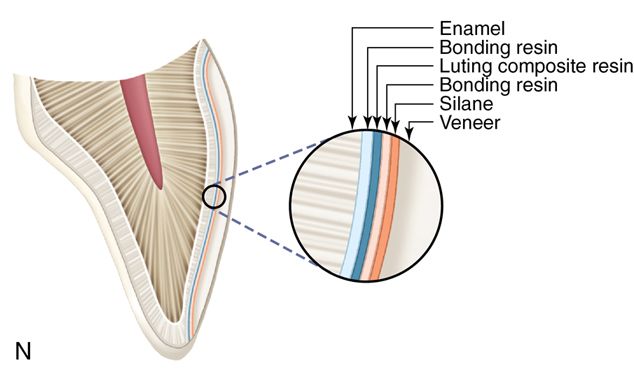
The technique described below is for a light-cured hybrid composite resin that is heat tempered, etched with 10% hydrofluoric acid gel, and treated with silane. The silane chemically bonds to the remaining glass particles and then to the luting composite resin, which is used to attach the laminate veneer to the etched enamel surface of the tooth. (Note that techniques may vary among manufacturers.)
Armamentarium.
• Metal “plastic” instrument (e.g., Hu-Friedy, Inc.)
• Anterior scaler (U-15 Towner, Hu-Friedy, Inc.)
• Medium grit flame or chamfer diamond bur
• Vinyl polysiloxane impression material
• Irreversible hydrocolloid impression material
• Maxillary and mandibular full arch impression trays
• Light-cured or dual-cured luting composite resin (see Chapter 12)
• Toaster oven or Coltene oven
• 12- and 30-fluted carbide finishing burs (e.g., ET Esthetic Trimming, Brasseler USA)
• Fine finishing diamond burs (e.g., ET Esthetic Trimming, Brasseler USA)
• Rubber composite resin polishing cups (see Chapter 5)
• Composite resin finishing disks (see Chapter 5)
• Composite resin polishing paste (see Chapter 5)
• 37% phosphoric acid gel(see Chapter 5)
• Dentin-enamel bonding resin (see Chapter 3)
• Intraoral light-curing unit (e.g., Demi Plus LED Dental Curing Light, Kerr Corp.)
Clinical technique.
1. Clean the tooth and the neighboring teeth with pumice.
2. Select the desired shades of composite resin while the teeth are wet with saliva.
3. Determine the desired alignment of the teeth.
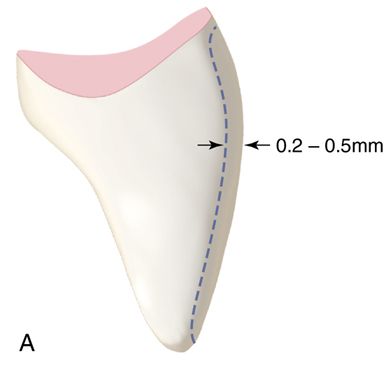
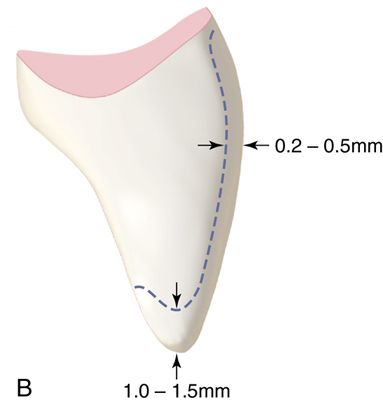
4. Prepare the eight maxillary anterior teeth by removing small amounts of enamel with a medium grit flame or chamfer diamond bur. If only minimum preparation is necessary to improve alignment and increase facial contour, remove only 0.25 to 0.50 mm of enamel from the facial area and none from the incisal area (Fig. 6-1 A). If incisal reduction is necessary, remove 1 to 1.5 mm (Fig. 6-1 B).











5. Make a full arch impression of the prepared teeth with a vinyl polysiloxane impression material. No retraction cord is needed because the margins are placed at the gingival crest.
6. Make a full arch irreversible hydrocolloid opposing impression.
7. Place a provisional restoration if needed (see Chapter 7)
8. Pour stone casts of both the prepared and the opposing arches. Laminate veneers can be fabricated on the stone cast by using a separating medium or on a flexible cast as described below.
9. After the stone is fully set, soak the cast of the prepared arch in water for 10 minutes and make an irreversible hydrocolloid impression of the cast.
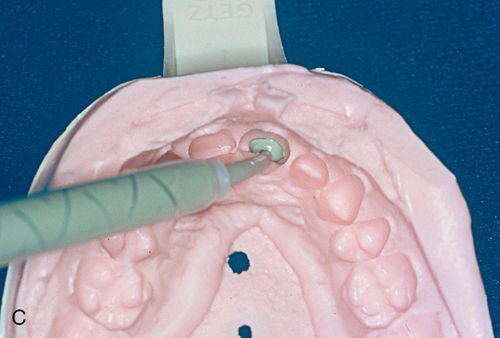
10. Inject a vinyl polysiloxane impression material (medium to heavy viscosity) into the irreversible hydrocolloid impression and form a flexible cast (Fig. 6-1 C). This technique was first developed by Dr. K. Michael Rhyne for use in indirect composite resin inlay fabrication.
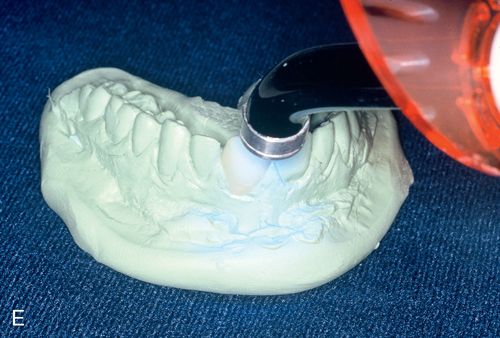
11. On the flexible cast, fabricate composite resin veneers using a technique similar to that described for direct intraoral application (Fig. 6-1 D).
12. Remove the laminate veneers from the flexible cast.
13. Contour and polish the laminate veneers using 12- and 30-fluted finishing carbide burs in a high-speed handpiece or porcelain contouring and polishing wheels on a lathe.
14. Place the laminate veneers on the original stone cast to check the fit and margins; adjust further if necessary (Fig. 6-1 F).
15. Heat treat the laminate veneers in boiling water or a heat device, such as the Coltene unit, for 10 minutes to achieve the heat-curing benefits.
16. Acid etch the lingual side of the laminate veneers with 10% hydrofluoric acid gel for 30 seconds (Fig. 6-1 G) or lightly sandblast with a microetcher or air abrasion unit and rinse thoroughly.
17. Evaluate the internal surfaces of the laminate veneers to ensure that an etched surface has been achieved (Fig. 6-1 H).
18. Clean the teeth with No. 4 fine pumice in a prophylaxis cup, rinse, and dry with water-free and oil-free air.
19. Clean the teeth with No. 4 fine pumice in a prophylaxis cup, rinse, and dry with water-free and oil-free air.
20. Use 37% phosphoric acid for 15 seconds to etch the enamel and remove the smear layer from any exposed dentin surface of the first central incisor (Fig. 6-1 I).
22. Leave the tooth surface slightly moist for wet bonding.
23. Using a brush, apply silane coupling agent to the internal surface of the laminate veneers and air dry.
24. Liberally coat the etched surfaces with a hydrophilic primer from a fourth generation dentin and enamel bonding agent (Fig. 6-1 J) and dry the primer with oil-free and water-free air until the surface appears glossy without being wet. This indicates that the “hybrid” layer has been established in the dentin and the enamel is thoroughly coated with the resin in the primer.
25. Paint a thin layer of bonding resin onto the internal surface of the laminate veneers.
26. Apply a luting composite resin to the internal surface of one of the laminate veneers. Place the laminate veneer on the prepared tooth and remove excess luting composite resin with a brush dipped in bonding agent (Fig. 6-1 K).
27. Polymerize for 40 seconds on the facial and lingual surfaces of the tooth (Fig. 6-1 L).
28. Remove excess polymerized luting composite resin with a #12 surgical blade or a scaler (Fig. 6-1 M).
29. Place the other laminate veneers in the same fashion.
30. Finish the margins with 12- and 30-fluted carbide finishing burs, fine diamonds, rubber polishing cups, finishing disks, or other composite resin finishing techniques (Fig. 6-1 N– P).
Prefabricated composite resin laminate veneers
Componeers (Coltene whaledent)
Componeers direct composite resin laminate veneers are polymerized, prefabricated composite resin enamel shells made of a nanohybrid composite resin in order to combine the advantages of direct composite resin with laboratory fabricated laminate veneers. The laminate veneers are 0.3 mm in thickness so that
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


