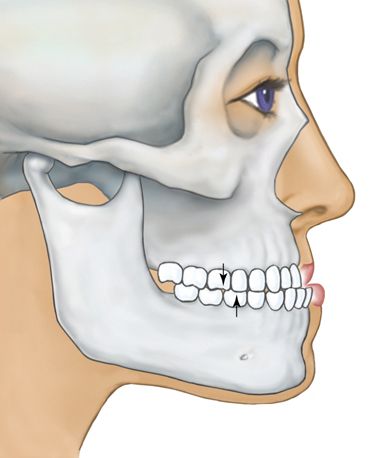
The mandibular incisor teeth may be used as a guide to determine what anteroposterior and vertical movements are required.
Fundamentals of orthodontics—types of movements
Types of appliances
Orthodontic tooth movements may be accomplished with many different types of orthodontic appliances. General dentists typically use clear aligner therapy, whereas orthodontic specialists have many other appliance choices. Some examples of typical orthodontic appliances are as follows:
1. Anterior ceramic or plastic brackets bonded to the facial surfaces of the teeth
2. Metal brackets bonded to the facial surfaces of the teeth
3. Lingual appliance—Specially designed metal brackets can be bonded to the lingual surfaces of teeth. Specially designed lingual arch wires must be used and the biomechanics of treatment must be analyzed to use this appliance.
4. Hawley appliance—A removable acrylic and metal wire appliance that can move teeth or can be used as a retainer (Fig. 15-2 A).
5. Functional appliances (e.g., Andresen, Bimler, Fränkel, Monobloc)—Removable appliances can fit over the teeth and reposition the maxilla or mandible to stimulate growth of the jaws to obtain the desired occlusion. Some of the appliances have plastic flanges that fit in the labial vestibule and prevent the buccal and orofacial musculature from contacting the teeth, thereby allowing some expansion of the jaws.
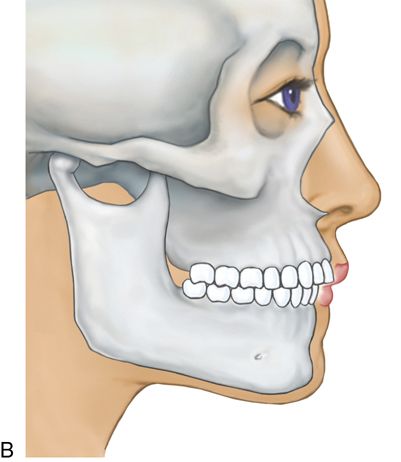
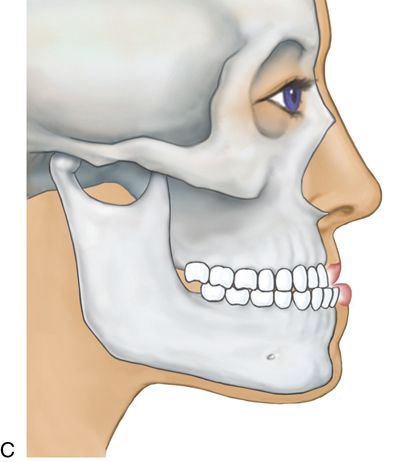
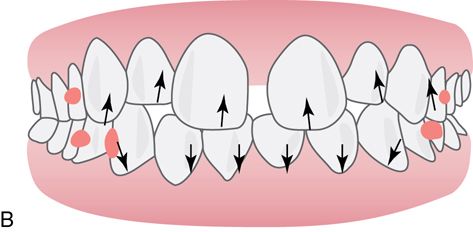
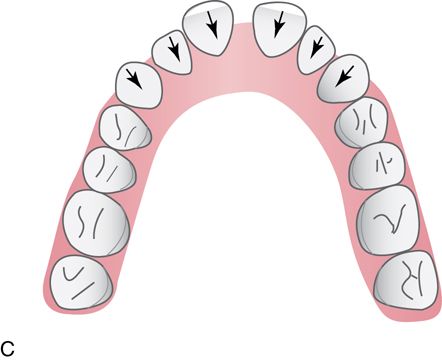
6. Spring aligners are removable appliances that can correct anterior tooth malpositions such as minor crowding or spacing. Anterior teeth are reset in an ideal setup in wax on a stone model. A removable appliance with active springs is fabricated over this ideal setup and the appliance is worn full time until the teeth achieve an acceptable alignment (Figs. 15-2 BC). It may then be worn at night as a retainer.
7. Clear aligners—Invisalign (Align Technology, Inc.), Insignia Clearguide (Ormco Corp.), or ClearCorrect (ClearCorrect) PVC vacuum formed appliances. Most clear aligners are sequentially fabricated through a three-dimensional computer technology to improve the position of the teeth incrementally. Essix appliances (Raintree Essix, Dentsply International) can be fabricated by either the clinician or the laboratory technician.



The most common modality used by general dentists is clear aligners such as the Invisalign System. Clear aligners have made it easier for the generalist to apply orthodontic forces to correct or improve malocclusions without the need for fixed traditional orthodontic therapy. A series of thermoplastic removable aligners achieve predictable movements. After treatment, occlusal stability must be ensured. An adjustment to the occlusion is usually necessary to balance the dentition in maximal intercuspation and all excursive movements. Changes in the occlusion occur during fixed and removable orthodontic treatment and the definitive positions of the teeth must have stability and long-term retention. Relapse can easily result from reoccurring interocclusal interferences during maximal intercuspation and/or excursive movements if the occlusion is not evaluated and adjusted, if necessary, at the end of any active phase of orthodontics. Proper training in this, and any approach to orthodontic therapy, is mandatory.
If Invisalign is used then, treatment begins with a ClinCheck design (Align Technology, Inc.), a web-based software product that creates and analyzes the dentition and creates a staged three-dimensional plan on virtual diagnostic casts. ClinCheck plans that are designed by the company should not to be accepted as a fully accurate representation of what the clinical outcome will be. Because of variability in the amount of time a patient wears the aligners, the fit of the aligners, the elasticity of the aligner material, and an individual’s physiologic responses to tooth movement, the proposed treatment plan may produce a treatment outcome that will be quite different than anticipated by the ClinCheck plans. The technicians involved in the treatment plans must be instructed by the dentist as to what the treatment objectives are for each patient. Each step (i.e., aligner change) needs to be evaluated by the doctor, who must predict if this plan will work. Clinicians can be as involved in the design as they wish to be. Some will design their own tooth movement sequences and attachment designs and others will rely on assistance from the laboratory. However, the dentist is ultimately responsible for treatment and results, even if assistance was requested. Treatment should begin only when the clinician is confident with the software-generated plan. Cases with questionable outcomes or questionable mechanics should be referred to an orthodontist.
With any removable device, tooth movement is dependent on proper patient compliance. Intermittent forces from less than ideal compliance result in the inability to attain the definitive treatment goals, which further results in orthodontic relapse, as will interocclusal interferences left unattended at the end of the active phase of orthodontics.
Clear aligner attachments
To enhance tooth movement with clear aligner therapy, small bonded shapes are placed on specific teeth with a template as a guide (Fig. 15-3 A).






The attachments help to optimize root control, extrusive movements and help with rotations. Originally, only oval attachments were available to assist the clear aligners with anchorage for tooth movements. Currently there are several types of clear aligner attachment shapes used to achieve specific tooth movements. These attachments not only provide the aligners with a better grip on the teeth, but also deliver a broader pushing surface to achieve a more controlled movement.
Clear aligner cases that are sequentially fabricated through a three-dimensional computer technology are delivered with an attachment template along with a series of aligners. The attachment template (Fig. 15-3 B) is a thinner, passive aligner, which is designed to create the shape of the desired attachments. After etching and priming the teeth, unpolymerized composite resin is placed into the wells of the template, which is then placed onto the maxillary and mandibular arches. The composite resin is light cured through the template plastic, the template is removed, and excess composite resin is eliminated.
Precision cuts serve as hooks in the plastic, which allow for the placement of interarch elastics. Precision cuts serve as hooks in the plastic that allow elastics to be used from maxillary to mandibular arches. The location of the cuts will create a direction of force, which will assist in directing the movements of the teeth. The direction of the elastic pull will determine the movement. The desired effect from the elastics is achieved only if the elastic is stretched in a way that favors the movements of the teeth. To correct a Class II malocclusion, a vector of force can be achieved with elastics stretched from the maxillary anterior teeth to the mandibular molars. A Class III force can be achieved with elastics directed from the mandibular anterior teeth to the maxillary molars. The resultant movement depends on patient compliance with proper wearing of the elastics with the clear aligners.
Treatment of clinical problems—general considerations
For the sake of simplicity, each type of malocclusion is discussed as a single entity. Often, however, the patient exhibits a combination of disharmonies. The definitive treatment plan must account for all the factors causing a malocclusion, allowing the dentist to select the most appropriate mechanotherapy to treat the particular patient.
Generalized spacing
Diagnosis.
Generalized spacing can be caused by the following:
3. Generalized spacing is confirmed by measuring the size of the teeth on diagnostic casts.
Generalized spacing is confirmed by measuring the size of the teeth on diagnostic casts. These conditions may be treated successfully with restorations by the general dentist, orthodontic space closure, or a combination of both orthodontics and restorative dentistry
If diastemata are localized, the clinician should suspect sucking or tongue habits. A large tongue that is physiologically active usually has a scalloped edge because of constantly pushing against the teeth. Sucking habits can range from involvement of the thumb to several fingers turned in various positions when placed in the mouth. The fingers that are used in a sucking habit invariably are cleaner than their neighbors and often exhibit a callus where the mandibular incisors contact them.
Treatment.
Elimination of pernicious habits is never easy but can be accomplished if the clinician is patient, persistent, and, most importantly, enlists the cooperation of the patient. The first step is to convince the patient that it is his or her responsibility to break the habit and that the doctor only offers assistance. It is helpful to encourage young patients to “give permission” for their parents to remind them that the habit exists. However, parents should not force the patient to stop. Start with small successes and build on them. It is essential to avoid discouraging the patient if small episodes of backsliding occur.
The plethora of devices used to break sucking habits speaks for their lack of singular success. They may be used, but should be considered adjuncts to the primary treatment previously described. Wearing cotton gloves is sometimes successful, as is the use of a bitter substance placed on the finger or fingernail used during the habit. Success can often be obtained by asking the patient to wear an elastic bandage around the elbow during the times the patient is concentrating on breaking the habit (usually at bedtime and reading time and while watching television). The patient’s parent should place the bandage so that no pressure occurs when the arm is extended. It should become tight when the elbow is bent. The resultant pressure on the elbow reminds the patient of the desire to stop the sucking habit. Frequent office visits reinforce patient progress. After the habit has been stopped, the spaces may correct by themselves or orthodontic closure may sometimes be necessary.
Diastema closure via arch contracture
In order to treat multiple spacing with contraction of the maxillary arch, the orthodontist must ensure that the mandibular antagonist does not interfere with movement.
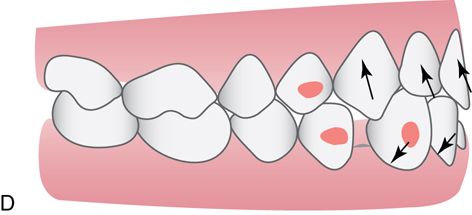
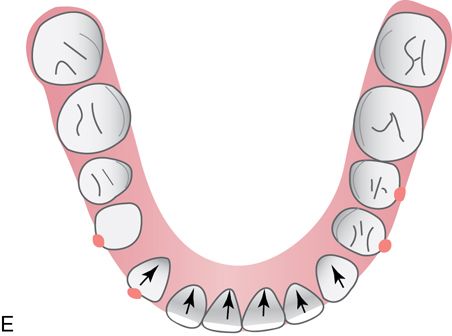
The most common generalized spacing situations involve anterior spacing and well aligned, Class I molar and premolar occlusion with tight interproximal contacts. The spaces occur most often due to outward tongue pressures against the lingual surfaces of the maxillary and mandibular incisors. The proclination of the incisors also may lead to maxillary and mandibular lip protrusion. The most effective way to eliminate this condition is to retract and intrude both the maxillary and mandibular anterior teeth simultaneously. Although the chief complaint will often refer to maxillary diastemata, the key to the correction is the retraction of the mandibular incisors, which would otherwise interfere with the retraction of the maxillary teeth (Fig. 15-4).
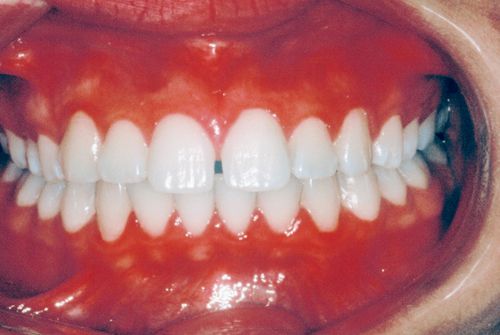
Mandibular spacing often occurs in these situations as well. In some instances, there are either no mandibular anterior spaces or mild crowding, which will then require interproximal reduction (IPR) to reposition the mandibular anterior teeth lingually. Intruding the mandibular anterior teeth during the retraction will help minimize these interferences. An evaluation must be performed for the presence of interferences between the mandibular incisal edges and the palatal and incisal surfaces of the maxillary incisors.
Localized spacing—clinically absent teeth
Diagnosis.
Causes of the clinical absence of teeth include the following:
Overlong retention of primary teeth can cause ectopic impaction of the permanent successors. Congenitally missing lateral incisors are discussed later in this chapter in the section on localized spacing of maxillary central incisors. The diagnosis ultimately is confirmed by examination of the appropriate radiographs.
Prosthetic treatment sometimes is complicated by the mesiodistal drifting of teeth adjacent to the edentulous space. This drifting can occur through tipping or bodily movement. In the latter situation, the crown and the apex of the root move bodily through the bone with the long axis of the tooth remaining perpendicular to the occlusal plane. In the former condition, the crown tips mesially or distally ahead of the apex of the root. Radiographs confirm the type of movement that has occurred.
Attempts to correct a mesiodistally drifted tooth with an abnormally proportioned restoration often create periodontal problems. Therefore, teeth should be orthodontically uprighted before prosthetic treatment.
Treatment.
Ectopic impaction should be treated by extraction of the primary teeth. If less than half of the root has formed, the permanent tooth usually is delayed in eruption. If more than half of the root is present and the tooth has failed to erupt despite the loss of the primary tooth, surgical exposure of the crown may be required, often followed by mechanical orthodontic therapy to force eruption of the tooth.
Congenitally missing teeth can be treated by prosthetic replacement. However, orthodontic intervention often is necessary if adjacent teeth have shifted mesiodistally.
Localized spacing of maxillary central incisors
Because of the great esthetic impact of localized spacing of the maxillary central incisors, this condition is described separately. The most common causes of this spacing are as follows:
2. Imperfect fusion of the midline
4. Congenitally missing lateral incisors
Radiographic evidence will confirm a spade-shaped septum when the labial frenum is malpositioned. This radiologic characteristic also is seen in imperfect fusion of the midline, but in such situations no blanching of the frenum occurs when the lip is stretched. Supernumerary teeth and congenitally missing lateral incisors are confirmed with radiographs. Spacing as part of normal growth also can occur in patients with small bony bases and large teeth. The large crowns of the developing and unerupted lateral incisors and canines push the central incisor roots mesially toward each other, causing the central incisor crowns to erupt with a distal inclination and an accompanying diastema. Anatomically small teeth may be confirmed by measurement.
Treatment
Normal growth.
If the spacing is determined to be part of normal growth, observe the patient until the lateral incisors and canines have erupted. In many instances, the diastema closes during the normal eruption process.
Imperfect fusion of the midline.
In the primary and mixed dentition, imperfect fusion of the midline becomes evident with the eruption of the permanent anterior teeth, including the canines, and should be treated in the permanent dentition stage. Treatment of imperfect fusion of the midline in the permanent dentition consists of moving the teeth together and retaining the positions.
Diastema closure—removable appliance
Simple closure of a maxillary midline diastema often creates spacing distally. For this reason, restorative dentistry may also be required to achieve proper esthetics (see Fig. 15-12).
The maxillary midline diastema is one of the most common chief complaints. The midline diastema in some patients is accompanied by small maxillary lateral incisors and/or mild mandibular crowding. There is usually a history of the familial maxillary midline diastema with a slow increase in diastema size over time. If restorations for enlargement of the lateral incisors are planned, the maxillary midline diastema can be closed and this space can be distributed distally and evenly between the lateral incisors. If there is no plan to change the dimension of the maxillary lateral incisors, then this situation is treated similarly to the generalized diastemata treatment plan. The goal is to retract and intrude the mandibular anterior teeth followed by maxillary anterior teeth retraction and intrusion. Mild mandibular crowding and/or the absence of anterior diastemata require IPR to allow for the retraction and intrusion of the mandibular incisors.


Diastema closure—fixed appliance
Fixed appliances require that the generalist be absolutely familiar with all aspects of fixed orthodontic therapy. Failure to adhere to proper orthodontic technique could have adverse consequences. Because simple closure of a maxillary midline diastema often creates spacing distally, restorative dentistry may also be required to achieve proper esthetics. To confidently maintain the space closure of the maxillary midline diastema, a fixed bonded retainer is suggested. Place a bonded wire palatally from central incisor to central incisor (Ortho-Flextech 30-inch gold chain [Reliance Orthodontic Products]). The bonded retainer must be out of occlusion or it will debond, causing flaring of the maxillary incisors, or cause unwanted movement of the mandibular incisors.
Enlarged or malpositioned frenum
Treatment and retention are identical to those described in the section on Generalized Spacing of maxillary central incisors earlier in this chapter except that a frenectomy is necessary.
Supernumerary teeth
Supernumerary teeth—for example, a mesiodens—must be extracted. After removal of the supernumerary tooth in the primary or mixed dentition, normal tooth eruption may correct the situation. If spacing, ectopic eruption, or malposition persists, use conventional orthodontic therapy. In the permanent dentition, conventional orthodontic therapy is required.
Congenitally missing lateral incisors
Congenitally missing permanent lateral incisors are not clinically evident in the primary dentition. If the condition is suspected from the family history, radiographs may be taken.
In the mixed dentition, congenitally missing lateral incisors can be clinically distinguished from other causes of localized spacing of the maxillary central incisors by overretention of the primary lateral incisors. Radiographs confirm the diagnosis.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


