The treatment of fractures of the frontal sinus has become less contentious as the contemporary principles of modern maxillofacial trauma management have become more widely adopted. The key rationale to treat fractures of the frontal sinus has always been to produce a “safe” sinus and reduce the long-term risks of complications. Early treatment was based on experience from the management of infective frontal sinus disease extrapolated to equate with the frontal sinus involved in trauma. The difficulty has been in predicting exactly which patients are at risk for these complications. Progress has been hampered by studies of small numbers of patients in retrospective reviews. Complications may develop many years after the initial trauma, with patients often presenting to teams not involved in the initial management. We will suggest that management of dural tears is the key to a “safe” sinus and has been under emphasized in the past.
The aim of this chapter is to provide an overview of currently accepted principles of management of frontal sinus fractures based on the experience of others and our own experience of more than 163 consecutive cases of craniofacial trauma managed between 1988 and 2008.
Historical Perspectives
Traditionally, in view of the perceived risk of infection and neurological deterioration, craniofacial injuries have been managed in at least two separate stages. These injuries were treated as separate entities by neurosurgeons and maxillofacial surgeons often working in isolation. Understanding of the aims of other specialties was limited, and the overall management of these injuries suffered as a result of the fragmented nature of the treatment.
Initial treatment usually consisted of urgent craniotomy for the evacuation of intracranial clots, elevation of depressed bone fragments, and repair of the dura over the convexity of the brain. Wounds were débrided, and loose bone fragments were discarded. Facial fracture repair was carried out 7 to 14 days or longer after the initial neurosurgical management. Formal exploration and reconstruction of the anterior cranial fossa (ACF) was seldom done, basal repair being limited to cases of persistent cerebrospinal fluid (CSF) rhinorrhea. Fixation of facial fractures was usually achieved with closed techniques by means of bone pins, halo frames, and internal suspension wires, which were usually attached to the teeth with the patient placed into intermaxillary fixation. Direct visualization of fracture sites by elevation of the periosteum was kept to a minimum for fear of devitalizing bone fragments. Primary bone grafting was rarely, if ever, performed. Contour defects of the forehead were treated secondarily, often with the use of alloplastic material such as methyl methacrylate.
The limitations of traditional frontobasal repair, combined with the lack of coordinated treatment, resulted in inadequate functional and cosmetic results, particularly in the critical frontal nasoethmoidal and orbital regions. Late secondary correction of these posttraumatic sequelae was difficult and often produced unsatisfactory results.
Management of the frontal sinus was based on historical experience in the treatment of acute and chronic frontal sinusitis. Initial techniques were based on the Reidel procedure of sinus ablation with excision of the bony walls. This approach resulted in severe frontal deformity and was later replaced by several modifications intended to exenterate the sinus mucosa while preserving the bony anatomy of the sinus. All of these techniques carried a significant failure rate. They were subsequently replaced by techniques to obliterate the sinus by excising the sinus mucosa, plugging the frontonasal ducts (FNDs), and obliterating the sinus with autogenous or alloplastic materials.
Fractures of the frontal sinus form an integral part of craniofacial fracture management and cannot be considered in isolation. This chapter examines the contemporary principles of craniofacial fracture management with particular reference to management of the frontal sinus.
Classification of Craniofacial Fractures
Fractures of the naso-fronto-orbital region account for approximately 5% of facial fractures. Fractures involving the anterior or posterior wall of the frontal sinus occur in 2% to 12% of cranial fractures. Combined frontobasilar and facial injuries may be isolated to the cranio-orbital area, or they may be part of more extensive injuries involving the upper, middle, and lower facial regions. Craniofacial fractures may be divided into central and lateral groups.
Central Injuries
Central injuries are those that involve the skull base adjacent to the paranasal sinuses: the frontal, ethmoid, and sphenoid sinuses. Central injuries are subdivided into two types depending on the location of the fracture.
Type I Cribriform Fracture
A type I cribriform fracture is a linear fracture that extends through the cribriform plate without involvement of the ethmoid or frontal sinuses. These fractures may result from relatively low-energy injuries that would not cause fractures in stronger areas of the anterior skull base. The dura covers this area with the arachnoid layer, and together they form tubular sheaths around the branches of the olfactory nerves, with the dura being continued into the periosteum of the nose and the arachnoid into the neurolemma of the nerve. The cribriform plate is thin, is easily fractured, and may be difficult to repair, resulting in a high propensity for the development of CSF fistulae ( Fig. 11-1 ).

Type II Frontoethmoidal Fracture
Type II frontoethmoidal fractures involve the medial portion of the ACF and directly involve the frontal or the ethmoid sinuses or both. As with type I fractures, CSF pools toward the midline, and this may prevent brain herniation and seal by brain or adjacent tissues ( Fig. 11-2 ).

Lateral Injuries
Lateral injuries involve the frontal bone and the orbital roof. These fractures may lie lateral to the frontal sinus, or they may involve the superior or inferior walls of the lateral frontal sinus. In this area, the brain is completely invested in dura, and the brain lies superior to the fracture site, in contrast to the situation with central injuries. CSF fistulae are therefore more likely to subside spontaneously as a result of gravity and brain herniation through the dural laceration ( Fig. 11-3 ).
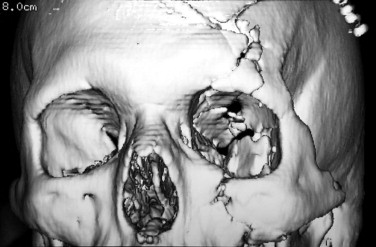
Complex injuries can occur in which a combination of central and lateral fracture patterns occurs ( Fig. 11-4 ).

Classification of Craniofacial Fractures
Fractures of the naso-fronto-orbital region account for approximately 5% of facial fractures. Fractures involving the anterior or posterior wall of the frontal sinus occur in 2% to 12% of cranial fractures. Combined frontobasilar and facial injuries may be isolated to the cranio-orbital area, or they may be part of more extensive injuries involving the upper, middle, and lower facial regions. Craniofacial fractures may be divided into central and lateral groups.
Central Injuries
Central injuries are those that involve the skull base adjacent to the paranasal sinuses: the frontal, ethmoid, and sphenoid sinuses. Central injuries are subdivided into two types depending on the location of the fracture.
Type I Cribriform Fracture
A type I cribriform fracture is a linear fracture that extends through the cribriform plate without involvement of the ethmoid or frontal sinuses. These fractures may result from relatively low-energy injuries that would not cause fractures in stronger areas of the anterior skull base. The dura covers this area with the arachnoid layer, and together they form tubular sheaths around the branches of the olfactory nerves, with the dura being continued into the periosteum of the nose and the arachnoid into the neurolemma of the nerve. The cribriform plate is thin, is easily fractured, and may be difficult to repair, resulting in a high propensity for the development of CSF fistulae ( Fig. 11-1 ).

Type II Frontoethmoidal Fracture
Type II frontoethmoidal fractures involve the medial portion of the ACF and directly involve the frontal or the ethmoid sinuses or both. As with type I fractures, CSF pools toward the midline, and this may prevent brain herniation and seal by brain or adjacent tissues ( Fig. 11-2 ).

Lateral Injuries
Lateral injuries involve the frontal bone and the orbital roof. These fractures may lie lateral to the frontal sinus, or they may involve the superior or inferior walls of the lateral frontal sinus. In this area, the brain is completely invested in dura, and the brain lies superior to the fracture site, in contrast to the situation with central injuries. CSF fistulae are therefore more likely to subside spontaneously as a result of gravity and brain herniation through the dural laceration ( Fig. 11-3 ).
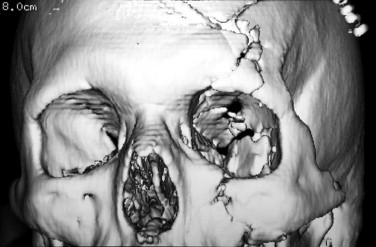
Complex injuries can occur in which a combination of central and lateral fracture patterns occurs ( Fig. 11-4 ).

Clinical Features
Up to one third of patients with a head injury and a Glasgow Coma Scale (GCS) score of 8 or less can be expected to have a major injury elsewhere in the body. All life-threatening conditions must be treated and stabilized before a full assessment of other injuries is undertaken. In addition, patients who are unconscious, particularly if they have sustained facial injuries, are unable to protect their own airway and should be intubated. The nature and severity of the craniofacial injuries are assessed once the patient has been stabilized after emergency treatment.
The risk of cervical spine injury in the unconscious patient with craniofacial injuries must be assumed until the spine can be “cleared” radiologically. The cervical spine should be stabilized with a hard cervical collar as part of the management of the airway, and the collar must be left in position until the cervical spine has been imaged. Radiographs should be taken to visualize the cervical spine from a lateral and an anteroposterior direction and a further film to visualize the odontoid peg. All seven cervical vertebrae must be visualized, including the cervicothoracic junction. If there is any doubt based on the plain radiographs, or if a soft tissue injury is suspected, computed tomography (CT) or magnetic resonance imaging (MRI) of the cervical spine (or both) must be obtained in the unconscious patient.
Clinical Examination
An initial assessment of the level of consciousness can be made using the acronym AVPU: a wake, responds to v ocal commands, responds to p ain, or u nresponsive. This provides a baseline against which more detailed assessment of the level of consciousness may subsequently be made.
Once the patient has been stabilized, a more detailed assessment of the level of consciousness is made and a thorough examination of the head and neck is performed. A full neurological assessment looking for focal or general neurological signs should also be included. The assessment of the level of consciousness should be repeated and recorded at regular intervals to detect any deterioration in the patient’s condition. The GCS provides a means of rapid and repeated assessment of the level of consciousness by individual or multiple clinicians and direct comparison of clinical findings. Any deterioration in the level of consciousness as evidenced by the GCS is an indication for an urgent CT scan. The GCS has three components: eye opening, best verbal response, and best motor response. The score in each group is totaled to give a final score of between 3 and 15. A score of 8 or less indicates that the patient is unconscious.
After assessment of the level of consciousness, examination of the head and neck should be undertaken, including the cervical spine if the patient is conscious. This should be performed in a systematic manner, starting with inspection of the scalp and working downward, noting any physical signs and palpating all bony margins. The eyes should be examined and the visual acuity, pupillary responses, range of eye movement, and presence of diplopia or restricted eye movements recorded. Visual fields should be tested to confrontation. The intercanthal distance should be recorded, particularly if nasoethmoidal injury is suspected. Sensation to light touch and pinprick should be tested in all three divisions of the trigeminal nerve. Facial nerve function should be assessed, particularly if a base-of-skull fracture is suspected or in the presence of facial lacerations that may involve the peripheral branches of the nerve. If the patient is conscious, it is important to inquire about loss of smell or hearing; if necessary, these should be formally tested. Initial assessment may be difficult in the acute situation because of the presence of blood in the nasal airway or external meatus.
The external auditory meatus should be inspected for the presence of hemotympanum, lacerations, damage to the tympanic membrane, and the presence of otorrhea.
Anterior rhinoscopy should be undertaken to examine for the presence of CSF rhinorrhea and nasal septal hematoma. This area may be difficult to visualize in the presence of blood. Clear secretions from the nose can be tested for glucose by the glucose oxidase test. This should be used only to confirm that the secretion is not CSF, because both nasal and lacrimal secretions may contain glucose. This test is unreliable and has been replaced by immunoelectrophoresis of the secretions for β 2 transferrin, which identifies CSF and does not produce false-positive results in the presence of nasal or lacrimal secretions or blood. β 2 transferrin is present in CSF but absent in tears, saliva, nasal secretions, and serum except perhaps in neonates and individuals with deranged liver function.
Intraoral examination should be performed to examine for bruising, swelling, and mobility of the tooth-bearing segments. The patient’s occlusion should be checked for evidence of derangement.
Clinical Findings
Skull vault fractures may manifest with localized scalp swelling and bruising with varying levels of consciousness. A range of neurological signs may also be present. The presence of an underlying intracranial hemorrhage correlates with the presence of a skull fracture and with the patient’s level of consciousness.
Fractures involving the ACF may show bilateral circumorbital ecchymoses, nasal epistaxis, and CSF rhinorrhea. A variety of eye signs may be demonstrated, including visual loss, and the patient may complain of loss of smell. Middle fossa fractures may demonstrate Battle’s sign (bruising around the mastoid process), blood in the external auditory meatus, and CSF otorrhea. There may be evidence of hearing loss or facial nerve weakness.
In craniofacial fractures, bruising around the eyes is common, and there may be evidence of subconjunctival hemorrhage. Subconjunctival hemorrhage as a physical sign merely demonstrates that bleeding has occurred deep to the orbital periosteum. Visual loss may occur as a result of the intracerebral insult or from direct trauma to the optic nerve itself, usually within the optic canal. Fractures extending into the orbital apex are rare because this area is the strongest part of the orbital skeleton. Fractures of the optic canal may occur, particularly with severe, high-energy injuries. Orbital fractures involving the superior orbital fissure may also occur and give rise to a range of physical signs depending on the individual nerves involved ( superior orbital fissure syndrome ). The oculomotor, trochlear, and ophthalmic divisions of the trigeminal and abducens nerves all pass through the superior orbital fissure and may produce limitation of eye movement, pupillary dilatation (mydriasis), and sensory disturbances in the frontal region (the supraorbital and supratrochlear branches of the ophthalmic division of the trigeminal nerve). The superior orbital fissure syndrome secondary to trauma is also a rare occurrence.
Pupillary mydriasis may be an indication of rising intracranial pressure as a result of its effect on the oculomotor nerve as it passes forward from the posterior aspect of the brainstem on its intracranial course. This occurs as a result of transtentorial herniation and is always secondary to a fall in the GCS. The oculomotor nerve contains parasympathetic fibers to the iris of the eye and is responsible for pupillary constriction (miosis). Direct damage to the oculomotor nerve may occur either intracranially or extracranially to produce an isolated third nerve palsy. The eye takes an abducted and depressed position with an associated mydriasis and upper eyelid ptosis. The direct pupillary reflex is absent, but is the consensual pupillary reflex are present if the ipsilateral optic nerve and the contralateral oculomotor nerve are both functioning normally. This is in contrast to an isolated optic nerve lesion, in which the ipsilateral direct and contralateral consensual pupillary reflexes are both absent.
Damage to the abducens and trochlear cranial nerves occurs less frequently. An isolated abducens nerve palsy produces an inability to abduct the eye, and an isolated trochlear nerve palsy produces an inability to abduct the eye in downward gaze. In all cases of damage to the third, fourth, and sixth cranial nerves, diplopia is present when the range of eye movements is assessed. With any suspected orbital or globe injury, an ophthalmic opinion must be sought. If eye signs are present, particularly restricted eye movements or diplopia, an orthoptic assessment should be performed, including a Hess chart.
The eyes should be assessed for the presence of enophthalmos. Assessment of enophthalmos in the acute situation may be difficult if its presence is masked by swelling of the periorbital tissues. Enophthalmos may occur with either orbital floor or medial wall blowout fractures if there is also rupture of the periorbita. Disruption of the medial orbital walls is invariably present in severe nasoethmoidal injuries and is therefore often present in craniofacial injuries.
Disruption of the attachments of the medial canthal tendons may also occur with nasoethmoidal injuries. The medial canthal tendon has an anterior limb that attaches to the anterior lacrimal crest and a posterior limb that lies posterior to the lacrimal sac. Disruption of the anterior limb of the tendon alone does not produce telecanthus (increase in the intercanthal distance). Telecanthus is a sign of disruption of both anterior and posterior limbs of the tendon and necessitates reattachment of the anterior limb to prevent persistence of the deformity postoperatively. The intercanthal distance should be checked in patients with suspected nasoethmoidal and craniofacial injuries. The normal intercanthal distance is 25.5 to 37.5 mm in women and 26.5 to 38.7 mm in men. Injuries to the medial canthal tendon may also occur with lacerations to the area in the absence of underlying fracture.
A fracture involving the frontal sinus may be suggested by the presence of a laceration in the region of the supraorbital ridge, glabella, or lower forehead.
Traumatic hypertelorism (increased inter-pupillary distance) may also occur in severe fronto-orbito-nasoethmoidal injuries with a true increase in the interorbital distance. Failure to appreciate the distinction between traumatic telecanthus and hypertelorism leads to inadequate treatment with a poor functional and cosmetic result.
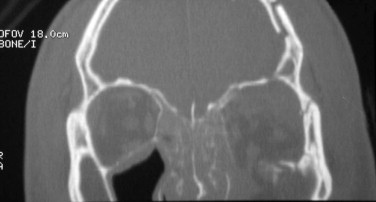
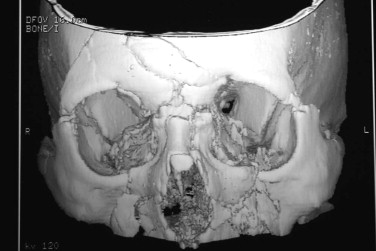
Radiological Assessment
CT scanning has revolutionized the management of craniofacial trauma by allowing precise delineation of injuries and exact preoperative planning before intervention. Assessment of both skeletal and soft tissue elements is possible with the use of appropriate bone and soft tissue windows. Scanning is performed in both the axial and coronal planes to allow visualization of all anatomical structures. The coronal views are essential for assessment of the orbital and frontal sinus roof and floor and for detailed assessment of the cribriform plate, the roofs of the ethmoid sinuses, the jugum sphenoidale, and the optic canals ( Fig. 11-5 ). All other fractures are usually demonstrated on the axial views. One-millimeter slices are required to allow adequate evaluation of the skull base and orbits. Three-dimensional (3-D) CT reconstruction often adds little in the way of practical information in the assessment of patients with craniofacial trauma but may be of benefit in selected complex cases ( Fig. 11-6 ).
Indications for Computed Tomography
CT scanning should be performed in all patients with suspected craniofacial injuries. In addition, a CT scan must also be obtained under any of the following circumstances:
- •
Basal skull fracture
- •
GCS <8
- •
Confusion persisting after resuscitation
- •
Deteriorating level of consciousness or progressive focal neurological deficit
- •
Seizure
- •
Neurological symptoms or signs including headache or vomiting
- •
CSF rhinorrhea or otorrhea
CT scanning is essential to precisely delineate the site and extent of injury associated with the frontal sinus. CT scanning may be used to assess injury to the ostia or ducts of the sinus. Fine-cut axial views will demonstrate disruption of the anterior and posterior walls of the sinus. Coronal views are necessary for adequate examination of the horizontal aspect of the frontal sinuses, the cribriform plates, the roofs of the ethmoid sinuses, and the orbits. It has been suggested that the level of fracture and degree of disruption of the base of the sinus predict the probability of ductal obstruction. We would question this. Our view is that it is not possible to predict with any degree of accuracy whether a sinus will continue to function after injury, based on imaging appearance alone.
Plain skull radiographs do not add to the information gained from CT scanning and are unnecessary in patients who are already undergoing CT.
Plain radiographs of the midface may give an extra overall dimension to information gained from the CT scan. It can be difficult to obtain satisfactory views in the unconscious patient, but plain films are of particular benefit in assessing facial symmetry after internal fixation of fractures.
If mandibular injury is suspected, the mandible may be imaged on plain films or as part of the overall CT scan.
Rationale for the Treatment of Craniofacial Fractures
Current management of craniofacial trauma is based on the principles of pediatric craniofacial surgery pioneered by Paul Tessier in 1967 and adopted to apply to craniofacial trauma by Merville in 1978. This was the first approach that addressed combined injuries in a definitive, single-stage repair. A frontal bone flap is raised to allow inspection of the dura, both convexity and basal, and its repair. The frontal sinus is cranialized, and the fronto-orbital and facial injuries are treated during the same anesthesia.
The aims of treatment for craniofacial injuries are twofold: (1) the restoration of satisfactory form and function and (2) the prevention of early and late complications, and in particular, infective sequelae.
Restoration of Satisfactory form and Function
The key to achieving accurate 3-D reconstruction in combined skull base and facial injuries is complete simultaneous exposure of the cranial vault, skull base, and facial fractures.
Accurate 3-D reconstruction of the frontal bandeau and orbital roofs is a prerequisite to satisfactory orbitofacial reconstruction. This may be achieved by reproducing the precise premorbid projection and convex curvature of the supraorbital rims. Laterally, the temporal buttresses of the frontal bone determine the projection and width of the upper midface. The position of the glabella in the midline determines the projection of the nasoethmoidal complex and may necessitate primary bone grafting in comminuted injuries or when bone is lost ( Fig. 11-7 ).

The convexity of the orbital roof in the anteroposterior and lateral planes must be reproduced to prevent globe displacement and disturbed ocular motility. Inaccurate reconstruction of the superior orbital rim and orbital roof resulting in inferior globe displacement is one of the most difficult posttraumatic deformities to correct satisfactorily. The premorbid ocular position can be reestablished by wide exposure and accurate reduction of the zygomatic arch and lateral orbital rim. The inner orbital skeleton can be reconstructed secondarily to the lateral position.
Prevention of Early and Late Infective Sequelae
Dural tears that communicate with the nasal cavity and paranasal sinuses are common in craniofacial fractures; if untreated, they may leave the patient at significant risk for either meningitis or a cerebral abscess. Importantly, the absence of an overt CSF leak does not indicate the absence of a dural tear. In the presence of a dural tear, the brain may act to plug the hole in the dura and prevent the CSF leak ( Fig. 11-8 ).

In 1954, Lewin showed the risk of meningitis to be at least 25% in patients with CSF rhinorrhea and cranial base fractures communicating with the paranasal sinuses in the absence of dural repair. In 1990, Eljamel and Foy reported on a series of patients with acute traumatic CSF fistulae. They found an overall incidence of meningitis of 30.6% before dural repair with a 10-year cumulative risk in excess of 80.5%. Surgical repair of the dura reduced the overall risk of meningitis from 30.6% before surgery to 4% after surgery; the cumulative risk at 10 years was reduced from 80.5% before dural repair to 7% after dural repair.
In 1989, Poole and Briggs published their approach to the management of craniofacial trauma based on their experience of 48 patients over a 7-year period. Their indications for combined craniofacial repair were:
- •
radiological evidence of displaced fractures involving the posterior wall of the frontal sinus, the cribriform plates, or the orbital roofs with or without the presence of CSF rhinorrhea.
- •
displaced fractures of the frontal bone or upper orbital skeleton.
- •
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


