According to most large series reported in the literature, fractures of the mandibular condyle account for 26% to 57% of all mandibular fractures. The male-to-female sex ratio ranges from 3 : 1 to 2 : 1 depending on which population is studied. Between 48% and 66% of patients with condylar fractures also have a fracture of the mandible body or angle.
Approximately 84% of condylar fractures are unilateral, and the most common causes are interpersonal violence, sports injury, falls, and road traffic accidents. According to Silvennoinen et al., approximately 14% are intracapsular, 24% condylar neck, 62% subcondylar, and 16% associated with severe displacement. The highest incidence of fractures is seen in patients between 20 and 39 years of age.
Fractures may be classified according to their location: intracapsular or condylar head, condylar neck, and subcondylar. Further subdivision may be made according to deviation, displacement, and dislocation of fragments in relation to the glenoid fossa. The importance of any classification is to be able to identify a subgroup so that outcomes can be meaningfully compared.
To avoid confusion, it should be noted that in the literature from continental Europe, the term “dislocation” may be used to indicate displacement, as it would be called in the United Kingdom and in the United States. Likewise, the European term “luxation” may be used instead of dislocation (UK/USA). In this chapter, the UK/USA nomenclature is used.
Classifications include that of Spiessel and Schroll :
| Type I: | Undisplaced condylar neck fracture |
| Type II: | Displaced low condylar neck fracture |
| Type III: | Displaced high condylar neck fracture |
| Type IV: | Fracture-dislocation—low neck |
| Type V: | Fracture-dislocation—high neck |
| Type VI: | Head or intracapsular fracture |
Other classifications include those of MacLennan and Lindahl and Hollender.
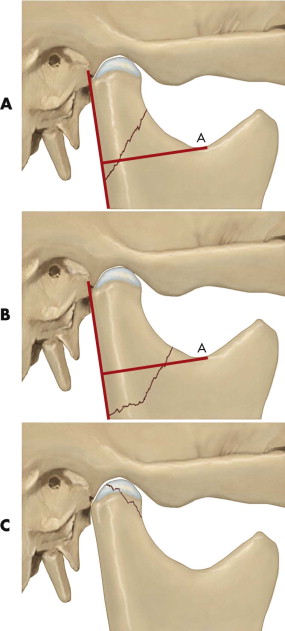
The classification adopted by the Strasbourg Osteosynthesis Research Group (SORG) in their pan-European prospective, randomized, controlled trial was as follows ( Fig. 16-1 ):
- 1
Diacapitular fracture (through the head of the condyle): The fracture line starts in the articular surface and may extend outside the capsule.
- 2
Fracture of the condylar neck: The fracture line starts somewhere above line A, the perpendicular line through the sigmoid notch to the tangent of the ramus; in more than half of cases, it runs above the line A in the lateral view.
- 3
Fracture of the condylar base: The fracture line runs behind the mandibular foramen and, in more than half of cases, below line A.
There has been a change in the evolving nomenclature of fractures of the condylar head. Previously, these fractures were known as intracapsular fractures, but it was found that in large numbers of cases, the condylar head fracture extends outside and inferior to the capsule on the medial aspect. This name was therefore abandoned because it is anatomically incorrect. The more accurate name, diacapitular fracture, was then adopted.
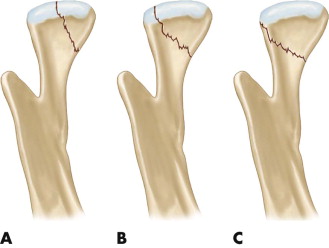
Subsequently, a more anatomical nomenclature was proposed, in which condylar head fractures were divided into three types ( Fig. 16-2 ). More recently, the importance of associated ramus shortening with these injuries was highlighted as an indicator for open intervention. Almost any direction of fracture propagation is possible, and in general, the greater the displacement of fragments, the less favorable the outcome.
Condylar fractures are complicated by their intimate relationship with the temporomandibular joint (TMJ). Direct fracture involvement of the joint or prolonged immobilization during treatment can lead to problems with deranged occlusion, internal derangement of the joint, ankylosis, and reduced mandibular growth. Symptomatically, these conditions manifest with long-term pain, limitation of jaw movement and function, asymmetrical growth, and malocclusion. TMJ ankylosis due to trauma is thought to account for only 0.4% of ankylosis cases.
In contrast to mandibular body fractures, which are now almost universally treated with osteosynthesis plates, there exists considerable variation in the management of condylar fractures in patients older than 12 years of age. Protagonists of conservative (closed) treatment methods cite evidence in the literature of satisfactory outcome with closed fracture management. They believe that the risks of scar formation, seventh nerve injury, and vascular compromise to the condylar head usually are not justified in simple condyle fractures.
In this chapter, we attempt to draw on the published literature, consensus practice, and our own unit’s policies to guide the reader in practical decision making when managing these fractures.
Clinical Findings and Investigations
Most condylar fractures are a result of blunt trauma to the anterior mandible. Forces are transmitted to the condylar region, where posterior movement of the mandible is limited by the glenoid fossa, the TMJ capsule, and insertion of the lateral pterygoid muscles. When the force is sufficient to overcome the strength of the condylar region, fracture follows. Trauma involving the open mouth leads to flexion fractures of the condyle. Symmetrical impact is said to cause bilateral fractures. Unilateral impact causes contralateral condylar fractures, and shearing forces are thought to produce intracapsular fractures. Closed-mouth fractures tend to distribute some of the energy to the occlusal surface of the teeth, and cuspal fractures are common.
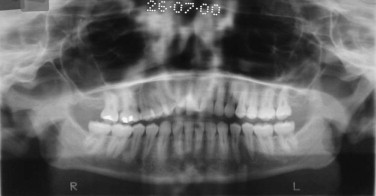
Under the influence of the masticatory muscles, the mandibular ramus may shorten vertically and produce premature occlusal contacts distally ( Fig. 16-3 ). The condylar fragment can dislocate out of the fossa, usually in an anterior direction; however, it may displace laterally, medially, or centrally into the middle cranial fossa. Any combination of fractures is possible, and joint maceration poses considerable surgical and healing difficulties.
Direct trauma to the TMJ area is unusual but may be associated with fractures of the zygomatic complex.
The derangement of the occlusion may give an indication of the fracture pattern. A unilateral fracture with sufficient fragment overlap or dislocation results in premature posterior contact and midline deviation on the affected side. Bilateral condylar fractures with overlap or dislocation produces bilateral posterior premature contact and anterior open bite with little or no chin deviation.
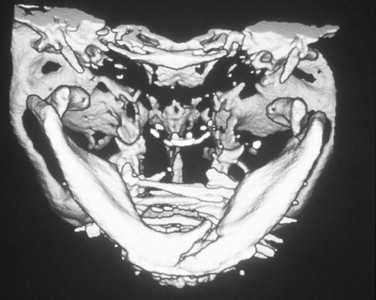
Comminuted mandibular fractures with bilateral condyle fractures produce crossbites and tend to increase the interangular distance, making accurate reduction challenging. Failure to recognize and correct this increased interangular distance leads to fixation of the body with a malocclusion ( Fig. 16-4 ). Accurate reduction with the use of temporary intermaxillary fixation (IMF) avoids this problem and is worth the time and effort before fixation of the mandibular body with miniplates.
Radiological imaging in two planes is required. An orthopantomogram (OPG) and posteroanterior (PA) mandible films are commonly used. Other projections include reverse Towne’s, lateral oblique, and basic tomographic views.
If surgery is being considered, computed tomography is recommended and may identify previously undiagnosed sagittal (diacapitular) or comminuted fractures. If meniscus and capsular disruption are suspected, magnetic resonance imaging is also advisable.
Management Strategies
The aims of condyle fracture treatment are to achieve:
- •
pain-free mouth opening with interincisal distance >40 mm.
- •
good movement of the jaw in all excursions.
- •
restoration of the pre-injury occlusion.
- •
stable TMJs.
- •
good facial and jaw symmetry.
Much of the debate is based on the fact that not all of these goals have an equal impact on the patient’s quality of life and outcome. For example, a jaw that deviates on opening is less of a problem than a severe anterior open bite.
Indications for Open Reduction and Internal Fixation
Absolute indications for open reduction and internal fixation (ORIF) in adult patients are:
- •
displacement into the middle cranial fossa or external auditory meatus.
- •
inability to obtain adequate occlusion by nonsurgical treatment.
- •
invasion by foreign body or gross contamination.
- •
lateral extracapsular displacement.
Relative indications are:
- •
bilateral fractures in edentulous jaws.
- •
IMF contraindicated for medical reasons.
- •
bilateral condyle fractures associated with comminuted midface fractures.
Indications for Nonsurgical Treatment
Nonsurgical treatment may be the appropriate management strategy in cases of:
- •
condylar neck fractures in children <12 years of age.
- •
high condylar neck fractures without displacement.
- •
intracapsular (diacapitular) condylar fractures without loss of ramus height.
- •
poor anesthetic risk.
Conservative Closed Functional Treatment
Definition of Closed Treatment
Closed treatment is treatment of condylar fractures by means other than surgical exploration, reduction, and fixation of the fracture line (i.e., not involving an open surgical exposure of the fracture). Traditionally, this has been achieved by arch bars, splints fitted over the remaining dentition, IMF, screws, or bonded brackets. Once reduction of the occlusion has been achieved, a period of immobilization may be required to encourage bony healing. Early mobilization is advised to minimize the risk of fibrous and bony TMJ ankylosis. This method of treatment is based on the principle that condylar nonunion is unlikely despite mobilization.
Definition of Closed Functional Treatment
Closed functional treatment involves the principles of closed treatment but is followed by at least 3 months of rehabilitation, including guiding elastics and mobilization regimens. It was found that when a full range of jaw movement is attained, normal jaw growth is not hindered. Adult muscles are more powerful than children’s and commonly cause jaw shift, leading to malocclusion. The application of elastics to guide the occlusion allows some degree of remodeling and articulation in its new position. Early mobilization reduces the development of soft tissue scarring and promotes increased mobility. Use of intermittent maxillomandibular elastic traction each night, followed by release in the morning for full daytime use, results in daily stretching of the soft tissues. The motion enables linear and circumarticular healing of these tissues sufficient to allow a full range of joint and jaw movement. Scarring and tethering are inevitable, but this treatment may allow full jaw mobility. Repeated holding of the jaw in occlusion at night results in a balance between remodeling of the condylar fracture and firm extension of the soft tissue healing. These are the principles of closed functional treatment.
To encourage mobilization, mechanical devices have been developed to provide continuous passive motion. However, they are cumbersome and expensive. An alternative is the use of wooden spatulas to achieve 40 mm of interincisal opening. The number of spatulas placed between the upper and lower molar and premolar teeth is gradually increased until the desired opening is achieved. They are then taped together to allow use four to five times per day during the 3 months of rehabilitation. Protrusive and excursive movements are equally important during this period.
The literature is inconclusive regarding the success of conservative treatment, because series are often contradictory. Original work carried out by the Chalmers J. Lyon Club provided the basis for the conservative approach, with good results reported in 120 cases treated conservatively. MacLennan and Blevins and Gores also published results supporting conservative treatment.
Based on research showing that bony union occurs in condylar fractures whether IMF is applied or not, the restoration of occlusion in a unilateral or bilateral condylar fracture through the use of IMF for 7 to 10 days and nonrigid immobilization for 3 to 4 weeks has provided a satisfactory functional outcome in many reported series. If there is gross displacement of the condylar fragment, IMF can achieve function through bony union of the fracture ends followed by pseudoarthrosis and re-education of the TMJ system over a 2- to 6-month period.
These early studies have been criticized heavily. In the case of the Chalmers J. Lyon Club, only 60 of the 120 patients were examined; the remainder were surveyed by mail. In MacLennan’s study, only 67 of the 120 patients were examined, and Blevins and Gore used a postal questionnaire. Furthermore, there was no stratification of severity of injury, and the caseloads spanned all ages. Subsequently, it was found that bony remodeling and restoration of function vary with age, raising questions about the interpretation of these series.
Evidence Supporting Closed Treatment of Unilateral Condylar Fractures in Adult Patients
Over a 12-year period, Marker et al. reviewed 348 patients who had closed treatment of mandibular condyle fractures. IMF was applied for 4 weeks in patients with condylar fractures alone and for 6 weeks in those with combined fractures of the mandible body. Patients were assessed for complaints, mouth opening, malocclusion, and deviation after treatment and again after 1 year. In this series, 72% of patients had unilateral fractures, and 28% had bilateral condylar fractures. After 1 year, 13% of patients stated that they had one or more physical complaints, including reduction in mouth opening, deviation on opening, malocclusion, clicking, and limited chewing ability. In these 13%, there was no difference in severity or frequency of symptoms according to whether a unilateral or bilateral fracture pattern was present. However, there was an association between cause of fracture and complaint. Unilateral fractures caused by sporting accidents and bilateral condylar fractures caused by road traffic accidents produced the greatest number of subjective complaints, although this difference was not statistically significant. Only 3% of the 348 patients complained of pain in the TMJ or muscles.
Mouth opening was recorded as abnormal immediately after treatment in 55% of cases; after 1 year, this had fallen to only 10%. In these patients, there was an almost equal distribution between unilateral and bilateral fracture pattern. Among patients with persistent limitation of movement at 1 year, 69% were treated by IMF and the remainder had soft diet alone. Malocclusion was detected in only 2% of the 348 patients assessed. On review of the degree of displacement and malocclusion, it was found that 31% of patients with bilateral displacement but only 5% of those with unilateral displacement developed malocclusion. Of the overall 2% with malocclusion, most could be treated with simple occlusal grinding; the remainder of patients were not concerned and did not wish further treatment. Only one patient required a sagittal split osteotomy to correct the malocclusion. Deviation on opening was recorded in 10% of cases and was more frequently associated with high forces at impact. The results were amalgamated to conclude that there were more complaints in the bilateral fracture group compared with the unilateral fracture group when measured objectively.
There was no record of the degree of angulation or overlap at presentation in Marker’s publication, but Silvennoinen et al. estimated that 50% of condylar fractures would fall into the operative category, and that estimate suggests that there should be more dissatisfied patients. However, complaints were few. Marker’s group therefore concluded that such rules are by no means a definite criterion for surgery. They advocated closed treatment but were cautious in applying this method to dislocations of the condylar head and bilateral fractures.
Joos and Kleinheinz published a prospective study of 122 adult patients with 138 condylar fractures. Fracture types were limited to Spiessel type II and type IV low condylar neck fractures. The patients were allowed to choose between closed and open treatment. Assessment included clinical examination, three-dimensional axiography, radiographic assessment, and ultrasound TMJ evaluation. The results showed no significant differences in outcome. The authors also tried to predict mathematically the potential for vertical repair and angulation repair in the nonoperated condyle. They concluded that 6 degrees of angulation can resolve and 4 mm of height can be regained. However, angles greater than 37 degrees can remodel little and lead to clinical problems.
Hidding et al. retrospectively analyzed 34 patients with unilateral displaced fractures of the condylar neck; 20 were treated surgically by ORIF and 14 by closed treatment. Outcome was assessed subjectively and analytically by axiography, radiography, and clinical and functional examination. Although some significant differences in measurement parameters were found, they could not conclude from the patients’ own mastication ability that one group recovered better than the other. One possible limitation to this paper is that results were measured only 5 years after treatment, and possible long-term sequelae are not predictable. However, Dahlstrom et al. suggested that there was little long-term change in their series. The authors concluded that ORIF of the displaced condylar fracture should be undertaken on the grounds of better measurement criteria rather than subjective outcome.
Konstantinovic and Dimitrijevic compared surgical versus nonsurgical treatment of unilateral condylar process fractures. By computer-simulated graphic presentations of PA radiographs of the mandible, actual posttreatment condylar reduction was compared with ideal reduction as determined by the computer. Based on standardized clinical evaluation (maximal mouth opening, deviation, and protrusion), no statistical difference was found between the open treatment ( n = 26) and closed treatment ( n = 54) groups. However, the radiographic examination showed a statistically better position of the surgically reduced condyle process fracture. This study would seem to discourage open surgery on the grounds of overtreatment. However, the patients’ treatment methods were not randomized, and there were many more patients with severe condylar displacement in the surgical group, as stated in the article. Therefore, if one assumes that the likelihood of problems after trauma becomes greater as the degree of condylar displacement increases, then this study also tends to support open treatment, because the two groups had similar treatment results.
Dahlstrom et al. reported on a 15-year follow-up of conservatively treated condylar fractures in 36 patients. This series provides the best data available on the long-term outlook of closed treatment. Those patients who had sustained their injury in childhood had excellent results, with no growth restriction. Adults had some degree of restriction, as did the teenage group (12-19 years). Twice as many patients in the older group experienced symptoms of dysfunction compared with the younger group. Radiologically, the younger group showed better ability to restore condylar morphology. Interestingly, the symptoms and signs at 6 months were similar to those at 15-year follow-up, suggesting that long-term gradual improvement cannot necessarily be expected. Also, it may be concluded that future study design may not need to be protracted.
In a prospective evaluation of 26 class VI fractures randomized to ORIF or conservative treatment, Landes et al. failed to demonstrate a benefit of the former treatment modality. Based on their results, the authors advocated closed treatment of these injuries. However, this study was based on a small cohort of patients, some of whom were not randomly allocated in order to achieve a balanced distribution between the two groups, thus deviating from the original protocol.
A study by Ellis et al. looked at the position of the condylar fragment when closed treatment was deemed appropriate and found that the condylar position was different after IMF than at the outset of treatment. This brings up the question: If the condyle position in an individual meets operative criteria after IMF, should conservative treatment be abandoned for ORIF? In this study, 65 patients were treated by closed treatment. Coronal and sagittal displacement was assessed before, immediately after, and 6 weeks after IMF, and a statistically significant difference (mean, −5.5 degrees) in the coronal position of the condylar process before and after arch bars was found. The change in a sagittal plane was not statistically significant. Other planes of movement were noticed but did not reach significance. Further changes were noted at 6 weeks’ follow-up. The authors concluded that care must be taken in basing treatment decisions on the degree of displacement or dislocation of the condylar process observed on presurgical radiographs.
In a more recent study by Ellis, all unilateral extracapsular fractures treated over a 10-year period (1998-2008) were reviewed retrospectively. Ellis concluded that the determination of which patients would not benefit from ORIF can be made clinically during surgery more reliably than with preoperative imaging studies. This conclusion was based on intraoperative assessment of mandibular deviation and “dropback.” If these are not found at operation, then open treatment is not necessary. However, closed functional treatment can also be used successfully in patients displaying deviation and the dropback phenomenon.
Evidence Supporting Open Treatment of Unilateral Fractures in Adult Patients
Palmieri et al. studied 136 patients with fractures of the condylar process; 74 were treated by closed methods and 62 by open methods. The patients were assessed for mandibular and condylar mobility at 6 weeks, 6 months, and 1, 2, and 3 years after surgery. A jaw-tracking device was used to assess mandibular motion. Radiographs were traced and digitized to assess condylar displacement and condylar mobility. It was accepted that patients treated by open reduction had significantly greater initial displacement of their condylar fractures compared with the closed-treatment group. As expected, condylar malposition persisted after closed treatment compared with open treatment. At 6 weeks, some measures of mobility were significantly greater in patients treated by the closed method compared to ORIF. However, after 6 weeks, there were minimal differences between the two groups, and subsequently there was significant improvement in mobility in the ORIF group. No measure of presurgical displacement correlated with mobility measures in patients treated by ORIF. However, several measures of condylar displacement correlated with measures of mobility in patients treated by the closed method, indicating that the more displaced the condylar process, the more limited the mobility. The authors concluded that patients treated by ORIF had somewhat greater condylar mobility than those treated by the closed method, even though the former group had more severely displaced fractures before surgery, and that ORIF can produce functional benefits in patients with severely displaced condylar process fractures.
Worsaae and Thorn published a series in which they evaluated 52 patients (24 with dislocated fractures) who were randomly assigned to receive either ORIF (24 patients) or closed treatment (28 patients). All fractures were unilateral, and the condyles were displaced from the fossa or overlapped at the fracture site (or both). All patients were 18 years of age or older and dentate. High condylar neck fractures were excluded from the study. The open treatment consisted of a submandibular incision and wire osteosynthesis followed by 6 weeks of IMF. The nonsurgical (closed) treatment consisted of an average of 30 days of IMF (range, 0 to 47 days). Both treatment groups had a median of 7 days of interarch training elastics after release of IMF. The mean follow-up period was 21 months for the ORIF group and 30 months for the closed treatment group, with each group having the same range, 6 to 64 months. The complication rate was 39% (11/28) in the nonsurgical group and only 4% (1/24) in the surgical group. The one patient with a problem in the surgical group had a collapse of the repositioned condyle and developed a malocclusion and muscle pain. In the nonsurgical group, there were three patients with mandibular asymmetry, eight with malocclusions, three with reduced mouth opening (<35 mm), two with persistent headaches, and six with muscle pain and impaired masticatory function. The median mouth opening for both groups was 45 mm, despite the relatively long periods in IMF; therefore, the extent of mouth opening alone did not separate the two groups. This study could have produced better results if more rigid fixation had been used instead of wire osteosynthesis. Also, IMF was used in both treatment groups.
Eckelt published a series of 103 patients treated by ORIF, 26 of whom had bilateral fractures. The results were far more superior than those achieved with closed treatment. He reported normal anatomical alignment in 84% and limitation of protrusion in only 6% of cases.
Hidding et al. investigated 34 patients with displaced fractures of the condylar neck, of whom 20 had been treated by open reduction and 14 by closed functional treatment. Assessment was by clinical, radiographic, and axiographic means. The clinical results were almost equal in both groups, but instrumental registration and radiographic findings showed considerable deviation in joint physiology in the closed-treatment group. Nineteen of the 20 patients who underwent surgery showed near-anatomical reconstruction with good functional results. It might reasonably be assumed that these patients would do better functionally in the long term as well.
Takenoshita et al. reported a comparison of open and closed reduction in 36 cases of condylar fracture with a 2-year follow-up. Sixteen patients underwent ORIF via preauricular and short Risdon incision, followed by 3 weeks of IMF. The other 20 patients were treated by only 3 weeks of IMF. The two groups were not randomly selected. The ORIF group was selected for surgery because they had dislocated or severely displaced condylar processes. The authors’ comparison showed that both groups had a similar result. If one assumes that severe condylar displacement is more likely to result in compromised jaw function, for which there is some evidence, then ORIF was beneficial for this surgical group. Again, IMF was used in both groups studied.
In a prospective investigation spanning 7 years, Ellis et al. studied occlusal results after open and closed treatment of unilateral condylar fractures. Treatment was decided according to patient choice after explanation of the two treatment modalities. Assessment of occlusion was made by examination of posttreatment standardized occlusal photographs by an orthodontist (blinded condition) and by surgeon (unblinded). Patients treated by ORIF had significantly more pretreatment condylar displacement than those treated by the closed technique. Patients treated by the closed technique had a significantly greater percentage of malocclusion than those treated by ORIF.
Hlawitschka et al. compared the results of open and closed treatment of diacapitular fractures of the mandible. Fifteen such fractures, associated with ramus shortening, were treated by ORIF. Outcomes were compared with those of 34 similar fractures treated with the use of a closed-technique. After ORIF, patients showed better radiological results with regard to mandibular ramus height, resorption, and pathological changes to the condyle. In both groups, some signs of dysfunction persisted, although there were slightly better results in the ORIF group. In 30% of the closed treatment group, lateral deviation during mouth opening, crepitus, and occlusal disturbances were noted. No cases of occlusal disturbance were observed in the ORIF group. Axiographic examinations revealed significant limitation of movement of the fractured condyle in both groups. However, after open treatment, the TMJ displayed significantly fewer irregularities in the condylar paths.
More recently, several clinical trials have attempted to address the clinical controversy surrounding decision making in relation to condylar fracture treatment. The data provided by these randomized, prospective studies indicate that better functional results can be expected by open reduction and internal fixation for moderately displaced condylar fractures with ramus shortening compared with closed treatment.
The SORG prospective, randomized trial involved seven international centers and compared operative and conservative treatment of displaced condylar fractures. The results were clearly in favor of the operative approach. The trial reported on 66 patients treated for 79 fractures and followed up for 6 months. Evaluation included radiographic assessment and clinical, functional, and subjective parameters including visual analogue scales for pain and the Mandibular Function Impairment Questionnaire index for dysfunction. Operative treatment was found to be superior in terms of all of the objective and all but one of the subjective functional parameters.
In another prospective, randomized trial, conducted between 2007 and 2009, both treatment options for condylar fractures yielded acceptable results. However, operative treatment was superior in terms of all objective and subjective functional parameters except occlusion.
Bilateral Condylar Fractures in Adults
In the consensus study by Baker et al., bilateral undisplaced fractures of the condyle were managed similarly by surgeons throughout the world. However, the introduction of condylar displacement, dislocation, and intracapsular fracture patterns revealed great variation in treatment preference when dealing with bilateral condylar fractures.
The Gronigen Consensus Group determined that there was good evidence that displaced bilateral condylar fractures benefit from treatment of at least one side by ORIF. It was accepted that this may cause an increased risk of even further displacement on the other side. It was noted that some displaced bilateral fractures can be treated successfully by the closed method but that predicting a favorable outcome is difficult.
Newman published a series of 61 patients with bilateral condylar fractures; 51% of patients had bilateral condylar fractures alone, and the remainder also had other fractures, mainly parasymphyseal. Almost half of the condylar fractures (46%) were undisplaced. In 39 patients (21%), the condylar fractures were managed by the closed method with wire rigid IMF for a mean of 37 days; 13 patients had conservative management (no intervention), and 9 patients (15%) with 10 fractured condyles underwent ORIF. The most common complaint after treatment was persistent limitation in mouth opening, which was significantly less in the ORIF group compared with the IMF group (mean opening ± standard deviation, 44 ± 2 mm versus 28 ± 2 mm; P < .01). More importantly, 10% of the patients treated by IMF required orthognathic surgery to correct a persistent anterior open bite, despite the long periods in rigid IMF. The authors also commented that most of those requiring orthognathic surgery had minimal angulation at presentation. They concluded that the risk of complications from ORIF were minimal and that, in the case of bilateral condylar fractures, ORIF should be undertaken on at least on one side if displacement or angulation is present.
Our unit policy involves the use of interarch elastic traction for a period of 1 week, followed by further assessment. If the occlusion is found to be satisfactory and the condylar fragments are undisplaced on OPG and PA views, we treat the fracture by the closed method. If the fragments are seen on one side to be overlapped by more than 2 mm or if the angulation is greater than 10 degrees, we select ORIF of the displaced fracture. If both sides show significant displacement and measurement of angulation and overlap are greater than the values stated, we advise ORIF on both sides ( Fig. 16-5 ), with each side being assessed on its own merits.

Particular care is needed to achieve very accurate reduction of the fragments before fixation. It may not be possible to hold the teeth in occlusion during the fixation procedure, because a downward distraction of the angle may be the only way to retrieve and reduce the condylar fragment. Once satisfactory fixation is achieved, the patient can be mobilized immediately postoperatively. To date, we have not experienced any seventh nerve injury that would change this policy.
The benefits of ORIF are:
- •
direct visualization of the fragments for accurate reduction and fixation.
- •
early mobilization of the mandible.
- •
early restoration of normal mouth and jaw activity.
Reported complications of open treatment include:
- •
poor esthetic result from the skin incision (particularly relevant if keloid scarring is likely).
- •
neural damage, especially to the facial nerve.
- •
intraoperative bleeding from the maxillary artery.
- •
loss of blood supply to the condylar head, leading to avascular necrosis.
Management of Condylar Fractures in Panfacial Injury
Panfacial injuries pose considerable challenges to the maxillofacial surgeon. Reduction and fixation of the facial skeleton must restore the correct anteroposterior (AP), lateral (width), and vertical dimensions. In the case of severe comminution of the midface and mandible, the only point of reference from which to start reconstruction is the stable posterior area (temporal bone and proximal zygomatic arch). One works sequentially to restore the AP projection, followed by reduction in width and restoration of the nasoethmoidal and orbital complex. Attention is then applied to accurate restoration of posterior vertical height by repositioning and fixation of the condylar ramus fracture. Access to the condylar fragment can be gained by extending the coronal incision that was used to access the zygomatic arch. Once posterior vertical height is restored, the anterior mandible can be fixed with accurate reduction in intercondylar width. Finally, occlusion is attended to, with fixation being applied lastly at the Le Fort I level, although some surgeons prefer to fix the occlusion at an earlier stage.
Management Strategies
The aims of condyle fracture treatment are to achieve:
- •
pain-free mouth opening with interincisal distance >40 mm.
- •
good movement of the jaw in all excursions.
- •
restoration of the pre-injury occlusion.
- •
stable TMJs.
- •
good facial and jaw symmetry.
Much of the debate is based on the fact that not all of these goals have an equal impact on the patient’s quality of life and outcome. For example, a jaw that deviates on opening is less of a problem than a severe anterior open bite.
Indications for Open Reduction and Internal Fixation
Absolute indications for open reduction and internal fixation (ORIF) in adult patients are:
- •
displacement into the middle cranial fossa or external auditory meatus.
- •
inability to obtain adequate occlusion by nonsurgical treatment.
- •
invasion by foreign body or gross contamination.
- •
lateral extracapsular displacement.
Relative indications are:
- •
bilateral fractures in edentulous jaws.
- •
IMF contraindicated for medical reasons.
- •
bilateral condyle fractures associated with comminuted midface fractures.
Indications for Nonsurgical Treatment
Nonsurgical treatment may be the appropriate management strategy in cases of:
- •
condylar neck fractures in children <12 years of age.
- •
high condylar neck fractures without displacement.
- •
intracapsular (diacapitular) condylar fractures without loss of ramus height.
- •
poor anesthetic risk.
Conservative Closed Functional Treatment
Definition of Closed Treatment
Closed treatment is treatment of condylar fractures by means other than surgical exploration, reduction, and fixation of the fracture line (i.e., not involving an open surgical exposure of the fracture). Traditionally, this has been achieved by arch bars, splints fitted over the remaining dentition, IMF, screws, or bonded brackets. Once reduction of the occlusion has been achieved, a period of immobilization may be required to encourage bony healing. Early mobilization is advised to minimize the risk of fibrous and bony TMJ ankylosis. This method of treatment is based on the principle that condylar nonunion is unlikely despite mobilization.
Definition of Closed Functional Treatment
Closed functional treatment involves the principles of closed treatment but is followed by at least 3 months of rehabilitation, including guiding elastics and mobilization regimens. It was found that when a full range of jaw movement is attained, normal jaw growth is not hindered. Adult muscles are more powerful than children’s and commonly cause jaw shift, leading to malocclusion. The application of elastics to guide the occlusion allows some degree of remodeling and articulation in its new position. Early mobilization reduces the development of soft tissue scarring and promotes increased mobility. Use of intermittent maxillomandibular elastic traction each night, followed by release in the morning for full daytime use, results in daily stretching of the soft tissues. The motion enables linear and circumarticular healing of these tissues sufficient to allow a full range of joint and jaw movement. Scarring and tethering are inevitable, but this treatment may allow full jaw mobility. Repeated holding of the jaw in occlusion at night results in a balance between remodeling of the condylar fracture and firm extension of the soft tissue healing. These are the principles of closed functional treatment.
To encourage mobilization, mechanical devices have been developed to provide continuous passive motion. However, they are cumbersome and expensive. An alternative is the use of wooden spatulas to achieve 40 mm of interincisal opening. The number of spatulas placed between the upper and lower molar and premolar teeth is gradually increased until the desired opening is achieved. They are then taped together to allow use four to five times per day during the 3 months of rehabilitation. Protrusive and excursive movements are equally important during this period.
The literature is inconclusive regarding the success of conservative treatment, because series are often contradictory. Original work carried out by the Chalmers J. Lyon Club provided the basis for the conservative approach, with good results reported in 120 cases treated conservatively. MacLennan and Blevins and Gores also published results supporting conservative treatment.
Based on research showing that bony union occurs in condylar fractures whether IMF is applied or not, the restoration of occlusion in a unilateral or bilateral condylar fracture through the use of IMF for 7 to 10 days and nonrigid immobilization for 3 to 4 weeks has provided a satisfactory functional outcome in many reported series. If there is gross displacement of the condylar fragment, IMF can achieve function through bony union of the fracture ends followed by pseudoarthrosis and re-education of the TMJ system over a 2- to 6-month period.
These early studies have been criticized heavily. In the case of the Chalmers J. Lyon Club, only 60 of the 120 patients were examined; the remainder were surveyed by mail. In MacLennan’s study, only 67 of the 120 patients were examined, and Blevins and Gore used a postal questionnaire. Furthermore, there was no stratification of severity of injury, and the caseloads spanned all ages. Subsequently, it was found that bony remodeling and restoration of function vary with age, raising questions about the interpretation of these series.
Evidence Supporting Closed Treatment of Unilateral Condylar Fractures in Adult Patients
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


