Locally Delivered, Controlled-Release Antimicrobials
Drug Development and Clinical Research
Drug Development and Registration
Phases of Drug Development
The typical investigational drug is studied in many clinical trials before an application can be submitted to the U.S. Food and Drug Administration (FDA) for clearance for commercial marketing in the United States (New Drug Application [NDA]). In the most general terms clinical trials prior to registration are often considered in three phases. Phase I trials are usually conducted in small numbers of healthy volunteers to determine preliminary safety and dosing. Phase II trials are typically conducted in larger numbers of patients to characterize preliminary safety in patients and further to determine dosing to be evaluated in later trials. Phase III includes large trials, often called pivotal or registration trials and usually multicenter, blinded, and randomized, in sufficiently large numbers of patients to provide conclusive evidence of safety and efficacy to support the submission of an NDA to the FDA for registration for marketed use. Following FDA registration, additional trials (Phase IV) may be performed to provide additional information about drug products including longer term safety and efficacy in a broader number of patients or in alternative practice settings. The general objectives of the phases of clinical research as described by the National Institutes of Health86 are given in Table 90-1. These typical phases of drug development now seem less distinct as trials are more lately considered in either exploratory or confirmatory stages.85 Additionally, specialized clinical pharmacology trials may be conducted at any phase in order to provide specific information such as, for example, pharmacokinetics or to address specific treatment conditions such as specific patient populations (e.g., geriatric or pediatric patients, patients with hepatic or renal impairment) or the effect of the drug on cardiac electrophysiology (e.g., QT phase prolongation). For an overview of the drug development process, the reader is referred to Tonkens83 or Mathieu and Milne.52 The FDA also offers a continuing education tutorial regarding human drug development and regulation, accessible at http://www.fda.gov/Training/ForHealthProfessionals/ucm209538.htm.
TABLE 90-1

Evaluating Safety and Efficacy
To approve a drug for marketed use in the United States, the FDA requires conclusive evidence that a drug is safe and effective for its intended use. As a general rule, data from at least two pivotal Phase III trials are required for regulatory decisions, although in some circumstances, for example in the case of a life-threatening disease such as cancer, only one trial might be required (when it would be considered unethical to withhold an effective treatment from patients and conduct a second trial). The concern is that results of one trial may represent a chance occurrence and should thus be confirmed by a second trial. Earlier trials, that is, Phase I and II, cannot provide data on which to base regulatory or clinical decisions. The FDA notes that each of these pivotal trials must be “adequate and well-controlled” and describes common characteristics of study designs that are considered adequate and well-controlled (Table 90-2).85 Specific comments about trial design, especially Phase III trials, and these characteristics are made later in this chapter.
TABLE 90-2
Characteristics of Adequate and Well-Controlled (Phase III) Clinical Trial Designs*
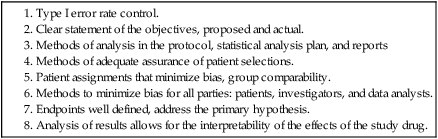
*Adapted from U.S. Food and Drug Administration (FDA) 21CFR314.126.85
Drugs must be shown to be safe and effective before they can be marketed.
Informed Consent and Legal Considerations
Informed consent is the standard within all dental practice. Clinicians must treat all patients under the principles of informed consent, and all patients must provide their consent for all treatment. With respect to clinical research, the FDA [adapted from 21CFR 50.25(a)84] describes eight elements of informed consent (Table 90-3). These elements apply to clinical practice as well. Appropriate treatment that satisfies the principles of informed consent generally includes treatment that is evidence-based, that is, supported by appropriate research data. Because locally delivered, controlled-release antimicrobials as adjuncts have been consistently shown in adequate and well-controlled clinical trials to enhance the efficacy of scaling and root planing (SRP) and provide an additional incremental benefit,31 performing SRP but not at least offering an adjunctive agent seems to violate the principles of informed consent.
TABLE 90-3
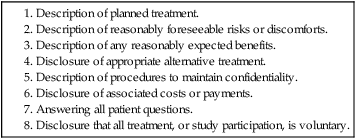
*Adapted from U.S. Food and Drug Administration (FDA) 21CFR 50.25.84
With respect to the issue of malpractice, undiagnosed or undertreated periodontitis are major sources of dental malpractice litigation.93 Since SRP procedures are commonly considered the standard of care for nonsurgical periodontal therapy,6,11 and available data support that adjunctive locally delivered, controlled-release antimicrobials enhance the efficacy of SRP,31 then SRP plus adjunctive therapy could potentially be considered a new standard. Other authors have noted the clinical relevance of locally delivered, controlled-release antimicrobials.* SRP without adjunctive therapy could accordingly be considered less than maximally effective. Would it be plausible to consider a possible defense in a malpractice litigation of alleged improperly managed periodontitis if it were claimed that the patient had not been offered maximally effective therapy (i.e., SRP with an adjunctive agent)?
Clinical Trial Evidence
Trial Design Considerations
Regulatory decisions generally depend on the data produced by adequate and well-controlled Phase III clinical trials to provide evidence that a drug is safe and effective when used as intended. These trials are usually large and conducted in many investigational centers in order (1) to enroll a sufficient number of patients to give the proper statistical power; and (2) to complete the trial within a reasonable length of time. Multicentered trials are enormously expensive and are difficult to perform. Clinical trials must be designed appropriately to test the hypotheses of interest. Some important design features of trials that are considered adequate and well-controlled are listed in Table 90-2 and further discussed below.
Endpoints Well Defined and Addressing the Primary Hypothesis.
A comment is needed about endpoints in periodontal trials. Current designs of clinical trials to assess periodontal outcomes are generally limited to the evaluation of surrogate endpoints (e.g., probing depth, attachment level) rather than direct and more clinically relevant endpoints such as tooth survival. An endpoint of tooth survival, although arguably more ideal, is not practical for a clinical trial that is to be conducted within a reasonable length of time or with a reasonable number of patients. Surrogate variables, however, are considered reasonable endpoints in periodontal clinical trials and relevant to tooth retention,28,34 although the inherent weaknesses of surrogate outcome variables have been noted.33 Additionally, there may be discordance among surrogate periodontal outcome endpoints,53 further highlighting the need for long-term data from clinical trials with tooth mortality as the primary objective.
Analysis of Results Allows for the Interpretability of the Effects of the Study Drug.
The pivotal trials for the chlorhexidine chip36 and the minocycline microspheres91 provide examples of Phase III designs for the study of adjunctive, locally delivered, controlled-release antimicrobials for the treatment of periodontitis. Representative populations of patients with chronic adult periodontitis were enrolled into multicentered, double-blinded clinical trials and were randomly assigned to treatment groups. Target pocket sites received SRP at baseline with or without adjunctive drug as per the randomization. At 3 and 6 months, sites randomized to drug received additional drug only if probing depth remained 5 mm or more. Final study results showed a reduction of probing depth from baseline at 9 months as expected in all groups, but the treatment group (SRP + adjunctive therapy) showed a significantly greater reduction from baseline versus control (SRP alone or SRP + placebo). If the adjunctive therapy had no effect, probing depth at these sites would have trended back toward baseline as in the SRP alone (or SRP + placebo) sites; the observation that probing depth remained reduced clearly demonstrated that the drug was efficacious. It should be noted for the chlorhexidine chip trials36 that baseline measurements were obtained following a supragingival scaling. Since a supragingival scaling might result in a mean probing depth reduction of approximately 0.3 to 0.4 mm,22 interpretation of the absolute changes in probing depth as a result of treatment should include a consideration of this potential prebaseline change.
Also with respect to these trials, it has been hypothesized that trial results might have been different had control groups also received repeated treatment (i.e., repeated SRP).5 If the control group had received repeated SRP, however, to maintain design balance the adjunctively treated group also would have had to receive repeated instrumentation. It cannot be assumed that results might have been different only for the control group. Additionally, locally delivered, controlled-release antimicrobials may be effective in the presence of calculus38 or with reduced amounts of instrumentation.90 Additional instrumentation also would have made data interpretation more difficult; multiple treatments at multiple times make it more difficult to separate treatment effects meaningfully. Further in support of the lack of an impact of additional instrumentation on the outcome, a similarly significant difference was reported when both treatment arms received SRP at baseline and a supragingival prophylaxis at 3 months.60
A final comment regarding locally delivered, controlled-release antimicrobials is needed regarding the consideration of adjunctive therapy or monotherapy. As suggested in Chapter 89, the general consensus of the professional community is that the best use for these products may be in the adjunctive setting. There are considerable data, however, that support efficacy in the monotherapy setting (for example, see Garrett et al25), and Garrett et al24 have suggested that monotherapy may be equally as effective as mechanical instrumentation for supportive periodontal maintenance. The authors cautioned, however, that further studies are needed to validate this treatment regimen and emphasized the importance of compliance including frequent supportive maintenance professional visits.
Clinical Use
Combination Adjunctive Therapy
Locally delivered, controlled-release antimicrobials have been shown to enhance the clinical efficacy of SRP. Similarly, adjunctive systemic therapy with low-dose (20 mg) doxycycline, given orally twice daily as a host-modulating agent (later reported as a once daily, modified-release formulation69), has also been shown to enhance the clinical efficacy of SRP68,16,13 (see Reddy et al70 or Ryan and Golub76 for a review of matrix metalloproteinase modulation as a treatment strategy). An obvious question is whether a combination of local antimicrobial and host-modulating adjunctive therapies will result in a greater clinical benefit compared with either adjunctive agent used alone.
In a 6-month clinical trial, combination adjunctive therapies resulted in significantly greater improvements in probing depth and clinical attachment compared with SRP alone.57 More sites showed a probing depth reduction 2.0 mm or more, and fewer sites had residual probing depth 5.0 mm or more.57 A single case report from this trial has been published.67 Because the appropriate control groups (SRP plus single adjunctive therapy) were not included in the trial, definitive conclusions regarding any increased benefit from combination versus single adjunctive therapy cannot be made. The potential for combined adjunctive therapy to enhance clinical benefit is promising and warrants additional research.
A final comment is needed regarding systemic adjunctive therapy with low-dose doxycycline. The focus of the present chapter is locally delivered, controlled-release antimicrobials—hence, the concentration on these agents. The data support the efficacy of these local antimicrobials,31 supporting the conclusion that SRP plus adjunctive therapy could potentially be considered a new standard for nonsurgical periodontal therapy. As above, available data also support the adjunctive efficacy of low-dose oral doxycycline69,68,16,13 to an extent that is numerically similar to that reported for locally delivered, controlled-release antimicrobials. Because appropriate comparative data are not available, comparisons of these therapies is not appropriate, and no conclusion can be reached regarding the most efficacious approach for adjunctive therapy, local or systemic with single agents, or combined as above.
Surgical Therapy
Pocket sites that do not seem to respond adequately to nonsurgical therapy and evidence residual probing depth with inflammation are often treated with follow-up surgical therapy. An interesting question is whether locally delivered, controlled-release antimicrobials could augment surgical results. This hypothesis was tested in a pilot study by Hellström and coworkers32 with minocycline microspheres at all pocket sites 5 mm or more. Sixty patients with at least one nonmolar pocket site with probing depth 6 mm or more in each of two quadrants were treated with either (1) microspheres at baseline, then immediately following each of two surgical procedures at weeks 2 and 3 and again at week 5; or (2) standard surgical therapy. The mean probing depth was reduced in both treatment groups, but the reduction was significantly greater in the test group versus control at 25 weeks (2.51 ± 0.10 mm vs. 2.18 ± 0.10 mm, respectively; p = 0.027).
A specialized periodontal surgical procedure, regenerative surgery, has become a standard procedure within periodontal practice. In this regard it had been suggested verbally, as early as 1993 (Killoy WJ, personal communication, 2002), and in print in 1998,40,45 that adjunctive locally delivered, controlled-release antimicrobials may improve outcomes following regenerative periodontal surgery. In a pilot clinical trial, the adjunctive use of the chlorhexidine chip with regenerative surgery resulted in more than a 100% greater mean improvement from baseline in bone height and mass 9 months after surgical treatment compared with SRP alone and surgery.71 It is worth noting that both groups had also received prophylactic systemic antimicrobial treatment as well prior to surgery, but the addition of a locally administered antimicrobial still resulted in a significant benefit compared with control.
Other reports support the lack of efficacy of systemic antimicrobials,54 and the benefit of locally delivered antimicrobials,92 as adjunctive treatments in the regenerative setting. A microbiological rationale for the use of locally delivered antimicrobials in the regenerative setting was also supported by Sbordone et al78 with regard to the tetracycline fiber. Aichelmann-Reidy and coworkers3 have suggested that regenerative surgical procedures should include an adjunctive locally delivered, controlled-release antimicrobial agent in order to provide a more consistent clinical benefit.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


