Plaque Biofilm Control for the Periodontal Patient
Microbial plaque biofilm control is an effective way of treating and preventing gingivitis and is an essential part of all the procedures involved in the treatment and prevention of periodontal diseases,47 It is critical to the long-term success of all periodontal and dental treatment.3 In 1965, Löe et al86 conducted the classic study demonstrating the relationship between microbial plaque biofilm accumulation and the development of experimental gingivitis in humans. Subjects in the study stopped brushing and other plaque biofilm control procedures, resulting in the development of gingivitis in every person within 7 to 21 days. The composition of the biofilm bacteria also shifted so that more virulent gram-negative organisms predominated, and these changes were shown to be reversible within 7 days. Good supragingival biofilm control has also been shown to affect the growth and composition of subgingival plaque, so that it favors a healthier microflora and reduces calculus formation.117 Carefully performed daily home plaque biofilm control, combined with frequent professionally delivered plaque biofilm and calculus removal, reduces the amount of supragingival biofilm; decreases the total number of microorganisms in moderately deep pockets, including furcation areas; and greatly reduces the quantity of periodontal pathogens.27,58 Reviews of home care procedures in 2011 and 2013 confirm the positive effects of daily plaque biofilm removal but cautions that these gains appear to be small and best results also require professional maintenance care.30,103
Microbial biofilm growth occurs within hours, and it must be completely removed at least once every 48 hours in the experimental setting with periodontally healthy subjects to prevent inflammation.116 The American Dental Association (ADA) recommends that individuals brush twice per day and use floss or other interdental cleaners once per day to effectively remove microbial plaque biofilms and prevent gingivitis.3 They recommend twice daily brushing because most individuals do not adequately remove microbial biofilms at one brushing and doing it a second time improves the results.
Periodontal lesions are predominantly found in interdental locations, so toothbrushing alone is not sufficient to control gingival and periodontal diseases.72 It has been demonstrated in healthy subjects that plaque biofilm formation begins on the interproximal surfaces where the toothbrush does not reach. Masses of biofilm first develop in the molar and premolar areas, followed by the proximal surfaces of the anterior teeth and the facial surfaces of the molars and premolars. Lingual surfaces accumulate the least amount of biofilm. Patients consistently leave more plaque biofilm on the posterior teeth than the anterior teeth, with interproximal surfaces retaining the highest amounts of biofilm, exactly the places in which periodontal infections begin.116 In addition, periodontal patients have increased susceptibility to disease,120 complex defects in gingival architecture, and long exposed root surfaces to clean, compounding the difficulty of doing a thorough job of cleaning.
Chemical inhibitors of plaque biofilm and calculus that are incorporated in mouthwashes or dentifrices also play important roles in controlling microbial biofilms.30 Fluorides delivered through toothpastes and mouthrinses are essential for caries control.36 Many products are available as adjunctive agents to mechanical techniques. These medicaments, as with any drug, should be recommended and prescribed according to the needs of individual patients.
The Toothbrush
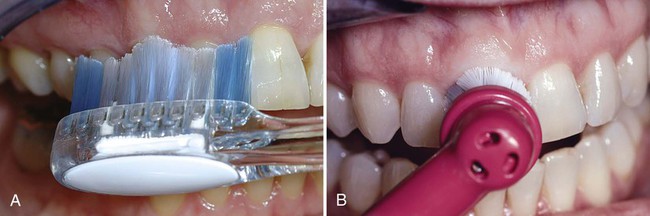
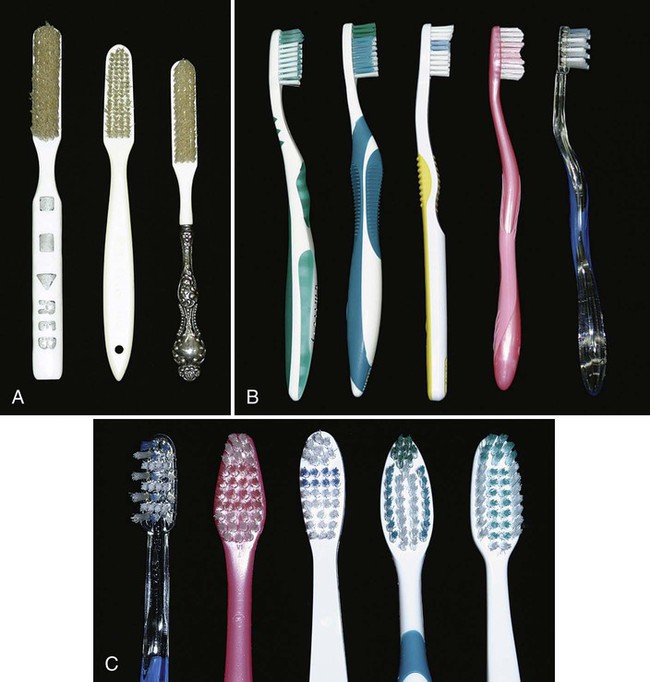
Toothbrushes vary in size and design as well as in length, hardness, and arrangement of the bristles111 (Figure 45-1). Some toothbrush manufacturers claim superiority of design for such factors as minor modifications of bristle placement, length, and stiffness. These claims are primarily based on plaque biofilm removal shown to be significantly superior to other toothbrushes in short-term clinical studies. However, the research does not show significant differences in gingivitis scores or bleeding indices, which are the more important measures of improved gingival health. In fact, at least one study compared four commercially available toothbrushes for total plaque biofilm removal at a single brushing; all four toothbrushes removed biofilms equally, and the authors concluded that no one design was superior to others.23 In addition, systematic review of multiple studies did not identify any one superior design.30
When recommending a particular toothbrush, ease of use by the patient and the perception that the brush works well are the important considerations. The effectiveness of and potential injury from different types of brushes depend to a great degree on how the brushes are used. Data from in vitro studies of abrasion by different manual toothbrushes suggest that brush designs permitting the bristles to carry more toothpaste while brushing contribute to abrasion more than brush bristles themselves.31 However, it has been shown that use of hard toothbrushes, vigorous horizontal brushing, and use of extremely abrasive dentifrices may lead to cervical abrasions of teeth and recession of gingiva.71
Toothbrush Design
Toothbrush bristles are grouped in tufts that are usually arranged in three or four rows. Rounded bristle ends cause fewer scratches on the gingiva than flat-cut bristles with sharp ends26,111 (see Figure 45-1). Two types of bristle material are used in toothbrushes: natural bristles from hogs and artificial filaments made of nylon. Both remove microbial plaque biofilms, but nylon bristle brushes vastly predominate in the market. Bristle hardness is proportional to the square of the diameter and inversely proportional to the square of bristle length.53 Diameters of common bristles range from 0.007 inch (0.2 mm) for soft brushes to 0.012 inch (0.3 mm) for medium brushes and 0.014 inch (0.4 mm) for hard brushes.60 Soft bristle brushes of the type described by Bass11 have gained wide acceptance. Handle design characteristics are entirely a matter of personal preference.
Softer bristles are more flexible, clean slightly below the gingival margin when used with a sulcular brushing technique,12 and reach farther onto the proximal surfaces.42 Use of hard-bristled toothbrushes is associated with more gingival recession.71 However, the manner in which a brush is used and the abrasiveness of the dentifrice affect the abrasion to a greater degree than the bristle hardness itself.90 Bristle hardness does not significantly affect wear on enamel surfaces.104
The amount of force used to brush is not critical for effective plaque biofilm removal.122 Vigorous brushing is not necessary and can lead to gingival recession, wedge-shaped defects in the cervical area of root surfaces,105 and painful ulceration of the gingiva.98
Toothbrushes must also be replaced periodically, although the amount of visible bristle wear does not appear to affect plaque biofilm removal for up to 9 weeks.25 Most clinicians recommend that toothbrushes be replaced every 3 to 4 months.
Recommendations
• Soft, nylon bristle toothbrushes clean effectively when used properly, remain effective for a reasonable time, and tend not to traumatize the gingiva or root surfaces.
• Toothbrushes should be replaced about every 3 to 4 months.
• If patients perceive a benefit from a particular brush design, they should use it.
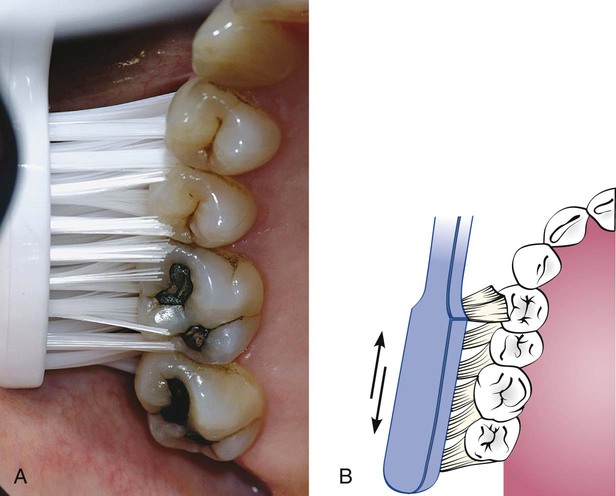
Powered Toothbrushes
Electrically powered toothbrushes designed to mimic back-and-forth brushing techniques were invented in 1939. Subsequent models featured circular or elliptical motions, and some had combinations of motions. Currently, powered toothbrushes have oscillating and rotating motions (Figure 45-2), and some brushes use low-frequency acoustic energy to enhance cleaning ability. Powered toothbrushes rely primarily on mechanical contact between the bristles and the tooth to remove plaque biofilm. The addition of low-frequency acoustic energy generates dynamic fluid movement and provides cleaning slightly away from the bristle tips.41 The vibrations have also been shown to interfere with bacterial adherence to oral surfaces. Neither the sonic vibration nor the mechanical motion of powered toothbrushes has been shown to affect bacterial cell viability.88 Hydrodynamic shear forces created by these brushes disrupt biofilms a short distance from the bristle tips, explaining the additional interproximal biofilm removal.64
Typically, comparison studies of powered toothbrushes, manual toothbrushes, or other powered devices demonstrate slightly improved plaque biofilm removal for the device of interest in short-term clinical trials.92,102 A recent Cochrane review reported that mechanical brushes with oscillating and rotating motions reduced microbial plaque biofilm 11% and demonstrated 6% greater reduction in gingival bleeding than manual brushing. These improvements were maintained over 3 months. Although long-term benefits have not been established, this particular style of mechanical brush resulted in better microbial plaque biofilm and gingivitis reduction in a number of well-controlled studies.30,55
Patient acceptance of powered toothbrushes is good. One study reported that 88.9% of patients introduced to a powered toothbrush would continue to use it.124 However, patients have also been reported to quit using powered toothbrushes after 5 or 6 months, presumably when the novelty is gone. Powered toothbrushes have been shown to improve oral health for (1) children and adolescents, (2) children with physical or mental disabilities, (3) hospitalized patients, including older adults who need to have their teeth cleaned by caregivers, and (4) patients with fixed orthodontic appliances. Powered brushes have not been shown to provide benefits routinely for patients with rheumatoid arthritis, children who are well-motivated brushers, or patients with chronic periodontitis.56
Recommendations
• Powered toothbrushes with oscillating and rotating motions remove plaque biofilm and reduce gingival bleeding slightly better than manual toothbrushes.
• Patients who want to use powered toothbrushes should be encouraged to do so.
• Patients need to be instructed in the proper use of powered devices.
• Patients who are poor brushers, children, and caregivers may particularly benefit from using powered toothbrushes.
Dentifrices
Dentifrices aid in cleaning and polishing tooth surfaces. They are used mostly in the form of pastes, although tooth powders and gels are also available. Dentifrices are made up of abrasives (e.g., silicon oxides, aluminum oxides, and granular polyvinyl chlorides), water, humectants, soap or detergent, flavoring and sweetening agents, therapeutic agents (e.g., fluorides, pyrophosphates), coloring agents, and preservatives.54,115 Abrasives are insoluble inorganic salts that enhance the abrasive action of toothbrushing as much as 40 times and make up 20% to 40% of dentifrices.90 Tooth powders are much more abrasive than pastes and contain about 95% abrasive materials. The abrasive quality of dentifrices affects enamel only slightly and is a much greater concern for patients with exposed roots. Dentin is abraded 25 times faster and cementum 35 times faster than enamel, so root surfaces are easily worn away, leading to notching and tooth sensitivity.115 Oral hygiene procedures mainly cause hard tissue damage from abrasive dentifrices, although gingival lesions can also be produced98,104 (Figure 45-3). Dentifrices are very useful for delivering therapeutic agents to the teeth and gingiva. The pronounced caries-preventive effect of fluorides incorporated in dentifrices has been proved beyond question.114 Fluoride ion must be available in the amount of 1000 to 1100 parts per million (ppm) to achieve caries reduction effects. Toothpaste products that have been tested by the ADA and have fluoride ion available in the appropriate amount carry the ADA seal of approval for caries control and can be relied on to provide caries protection.5

“Calculus control toothpastes,” also referred to as “tartar control toothpastes,” contain pyrophosphates and have been shown to reduce the deposition of new calculus on teeth. These ingredients interfere with crystal formation in calculus but do not affect the fluoride ion in the paste or increase tooth sensitivity. Dentifrice with pyrophosphates has been shown to reduce the formation of new supragingival calculus by 30% or more.67,89,129 Pyrophosphate-containing toothpastes do not affect subgingival calculus formation or gingival inflammation. The inhibitory effects reduce the deposition of new supragingival calculus but do not affect existing calculus deposits. To achieve the greatest effect from calculus control toothpaste, the patient’s teeth must be cleaned and completely free of supragingival calculus when adding these products to the daily home care regimen.
Recommendations
• Dentifrices increase the effectiveness of brushing but should cause a minimum of abrasion to root surfaces.
• Products containing fluorides and antimicrobial agents provide additional benefits for controlling caries and gingivitis.
• Patients who form significant amounts of supragingival calculus benefit from the use of a calculus control dentifrice.
Toothbrushing Methods
Many methods for brushing the teeth have been described and promoted as being efficient and effective. These methods can be categorized primarily according to the pattern of motion when brushing and are primarily of historic interest, as follows65:
Roll: Roll2 or modified Stillman technique61
Vibratory: Stillman,113 Charters,20 and Bass12 techniques
Patients with periodontal disease are most frequently taught a sulcular brushing technique using a vibratory motion to improve access to the gingival margin areas. It is important for patients to understand that the plaque biofilm removal at the dento-gingival junction is necessary to prevent caries as well as periodontal disease. This is referred to as “target hygiene.”118 The method most often recommended is the Bass technique because it emphasizes the placement of the bristles at this most important area. This sulcular placement of the bristle and adapting the bristle tips to the gingival margin to reach the supragingival plaque biofilm and accessing some of the subgingival biofilm may be the most important aspect of “target hygiene.” A controlled vibrating motion is used to dislodge microbial plaque biofilm and avoid trauma. The brush is systematically placed on all the teeth in both arches. Figures 45-4 and 45-5 illustrate this brushing technique.
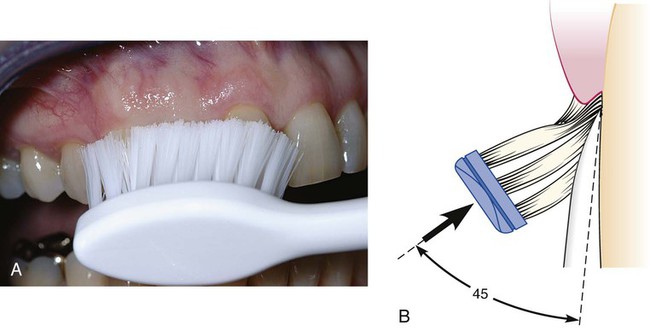
Bass Technique11
1. Place the head of a soft brush parallel with the occlusal plane, with the brush head covering three to four teeth, beginning at the most distal tooth in the arch.
2. Place the bristles at the gingival margin, pointing at a 45-degree angle to the long axis of the teeth.
3. Exert gentle vibratory pressure, using short, back-and-forth motions without dislodging the tips of the bristles. This motion forces the bristle ends into the gingival sulcus area (see Figure 45-4), as well as partly into the interproximal embrasures. The pressure should be firm enough to blanch the gingiva
Brushing with Powered Toothbrushes
The various mechanical motions built into powered toothbrushes do not require special techniques. The patient needs only place the brush head next to the teeth at the gingival margin, using a targeted hygiene approach, and proceed systematically around the dentition.121 A routine method of brushing all the teeth, similar to the method described for manual brushing, should also be used with powered toothbrushes (Figure 45-6).
Recommendations
• Targeted hygiene118 focuses brushing efforts on the cervical and interproximal portions of the teeth, where microbial plaque biofilm accumulates first.
• Brushing with either a manual or a powered toothbrush requires a systematic routine to clean all the accessible areas.92
• Patients will modify any technique to their needs but must achieve the goal of brushing effectively until the teeth are free of plaque biofilm on all accessible surfaces.
Interdental Cleaning Aids
Any toothbrush, regardless of the brushing method used, does not completely remove interdental plaque biofilms. This is true for all brushers, even periodontal patients with wide-open embrasures.44,107 Daily interdental plaque biofilm removal is crucial to augment the effects of toothbrushing because most dental and periodontal diseases originate in interproximal areas.1
Tissue destruction associated with periodontal disease often leaves large, open spaces between teeth and long, exposed root surfaces with anatomic concavities and furcations. These areas shelter plaque biofilms and are both difficult for patients to clean and poorly accessible to the toothbrush.72 Patients need to understand that the purpose of interdental cleaning is to remove microbial plaque biofilms, not just dislodge food wedged between teeth. Many tools are available for interproximal cleaning and they should be recommended based on the size of interdental spaces, presence of furcations, tooth alignment, and presence of orthodontic appliances or fixed prostheses. Also, ease of use and patient cooperation are important considerations. Common aids are dental floss and interdental cleaners such as wooden or plastic tips, and interdental brushes.
Dental Floss
Dental floss is the most widely recommended tool for removing biofilm from proximal tooth surfaces.43 Floss is made from nylon filaments or plastic monofilaments, and comes in waxed, unwaxed, thick, thin, and flavored varieties. Some prefer monofilament flosses made of a nonstick material because they are slick and do not fray. Clinical research has demonstrated no significant differences in the ability of the various types of floss to remove dental plaque biofilm; they all work equally well.38,59,69,70 Waxed dental floss was thought to leave a waxy film on proximal surfaces, thus contributing to biofilm accumulation and gingivitis. It has been shown, however, that wax is not deposited on tooth surfaces99 and that improvement in gingival health is unrelated to the type of floss used.38 Factors influencing the choice of dental floss include the tightness of tooth contacts, roughness of proximal surfaces, and the patient’s manual dexterity, not the superiority of any one product. Therefore recommendations about type of floss should be based on ease of use and personal preference.
Technique.
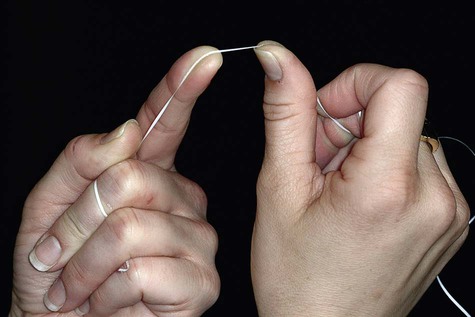
1. Start with a piece of floss long enough to grasp securely; 12 to 18 inches is usually sufficient. It may be wrapped around the fingers, or the ends may be tied together in a loop.
2. Stretch the floss tightly between the thumb and forefinger (Figure 45-7), or between both forefingers, and pass it gently through each contact area with a firm back-and-forth motion. Do not snap the floss past the contact area because this may injure the interdental gingiva. In fact, zealous snapping of floss through contact areas creates proximal grooves in the gingiva.
3. Once the floss is apical to the contact area between the teeth, wrap the floss around the proximal surface of one tooth, and slip it under the marginal gingiva. Move the floss firmly along the tooth up to the contact area and gently down into the sulcus again, repeating this up-and-down stroke two or three times (Figure 45-8). Then, move the floss across the interdental gingiva, and repeat the procedure on the proximal surface of the adjacent tooth.

4. Continue through the whole dentition, including the distal surface of the last tooth in each quadrant. When the working portion of the floss shreds or becomes dirty, move to a fresh portion of floss.
Flossing can be facilitated by using a floss holder (Figure 45-9, A). Floss holders are helpful for patients lacking manual dexterity and for caregivers assisting patients in cleaning their teeth. A floss holder should be rigid enough to keep the floss taut when penetrating into tight contact areas, and it should be simple to string with floss. The disadvantage is that floss tools are time-consuming because they must be rethreaded frequently when the floss shreds.
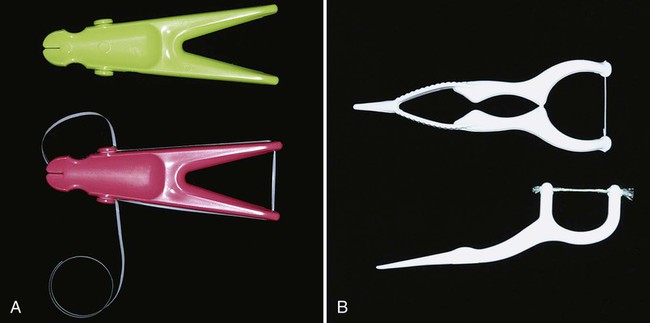
Disposable, single-use floss holders with prethreaded floss are also available. Short-term clinical studies suggest that plaque biofilm reduction and improvement in gingivitis scores are similar for patients using disposable floss devices as for patients who hold the floss with their fingers18,112 (Figure 45-9, B).
Powered flossing devices are also available (Figure 45-10). The devices have been shown to be safe and effective, but no better at plaque biofilm removal than holding the floss in the fingers.24,49

Establishing a lifelong habit of flossing the teeth is difficult to achieve for both patients and dentists, regardless of whether one uses a tool or flosses with the fingers. In fact, the daily use of floss is universally low. It has been reported that only about 8% of young teenagers in Great Britain flossed daily,87 with similar percentages reported for other countries.72 No information is available about the establishment of long-term flossing habits comparing the various tools to finger flossing. However, the tools may be useful to help some individuals begin flossing or to make flossing possible if patients have limited dexterity.
Interdental Cleaning Devices
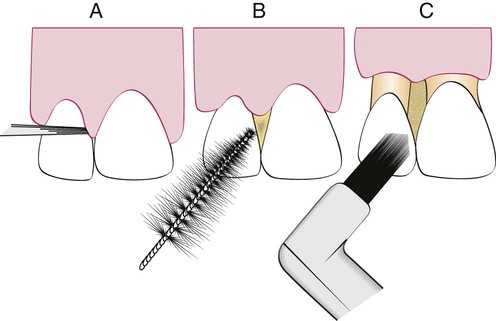
Concave root surfaces such as the mesial aspect of the maxillary first bicuspid and furcations are often present in periodontal patients who have experienced significant attachment loss and recession, and they are not cleaned well with dental floss. A comparison study of dental floss and interdental brushes used by patients with moderate to severe periodontal disease showed that the interproximal brushes removed slightly more interproximal plaque biofilm and that subjects found them easier to use than dental floss. However, no differences were seen in probe depth reductions or bleeding indices.21 Therefore interproximal cleaning aids, such as interdental brushes, are adequate for proximal cleaning of teeth when interdental spaces permit access.72
Embrasure spaces vary greatly in size and shape. Figure 45-11 provides a representation of the size and anatomy of three types of embrasures and the type of interdental cleaner often recommended for each. As a general rule, the larger the space, the larger the device needed to clean it.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses