Restorative Interrelationships
Biologic Considerations
Margin Placement and Biologic Width
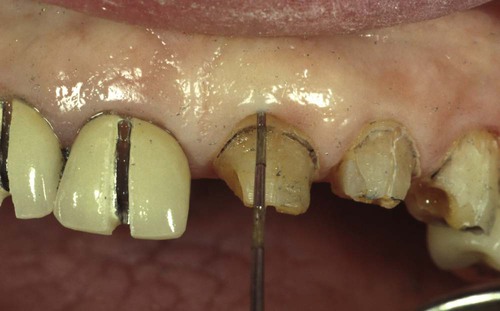
A clinician is presented with three options for margin placement: supragingival, equigingival (even with the tissue), and subgingival.69 The supragingival margin has the least impact on the periodontium. Classically, this margin location has been applied in unesthetic areas because of the marked contrast in color and opacity of traditional restorative materials against the tooth. With the advent of more translucent restorative materials, adhesive dentistry, and resin cements, the ability to place supragingival margins in esthetic areas is now a reality (Figures 67-1 and 67-2). Therefore, whenever possible, these restorations should be chosen not only for their esthetic advantages but also for their favorable periodontal impact.

The preparations for six porcelain veneers with the margins placed at the level of tissue are shown.

Note the invisible gingival finish line, even though the margin has not been carried below tissue.
The greatest biologic risk occurs when placing subgingival margins.42 These margins are not as accessible as supragingival or equigingival margins for finishing procedures. In addition, if the margin is placed too far below the gingival tissue crest, it violates the gingival attachment apparatus.
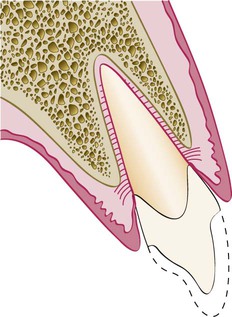
As described in Chapter 1, the dimension of space that the healthy gingival tissues occupy between the base of the sulcus and the underlying alveolar bone is comprised of the junctional epithelial attachment and the connective tissue attachment. The combined attachment width is now identified as the biologic width. Most authors credit Gargiulo, Wentz, and Orban’s 1961 study18 on cadavers with the initial research establishing the dimensions of space required by the gingival tissues. They found that, in the average human, the connective tissue attachment occupies 1.07 mm of space above the crest of the alveolar bone and that the junctional epithelial attachment below the base of the gingival sulcus occupies another 0.97 mm of space above the connective tissue attachment. The combination of these two measurements, averaging approximately 1 mm each, constitutes the biologic width (Figure 67-3). Clinically, this information is applied to diagnose biologic width violations when the restoration margin is placed 2 mm or less away from the alveolar bone and the gingival tissues are inflamed with no other etiologic factors evident.
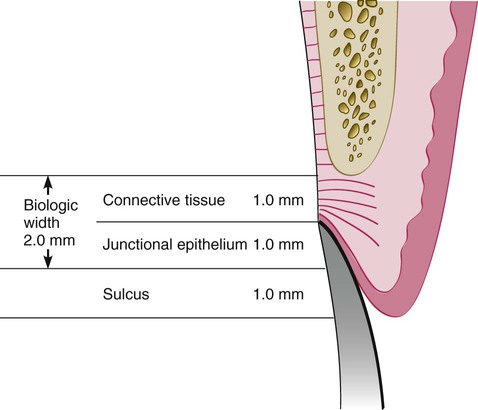
Connective tissue attachment 1 mm in height; junctional epithelial attachment 1 mm in height; sulcus depth of approximately 1 mm. The combined connective tissue attachment and junctional epithelial attachment, or biologic width, equals 2 mm.
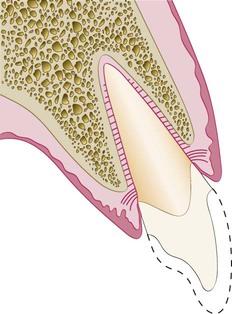
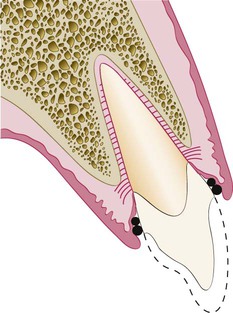
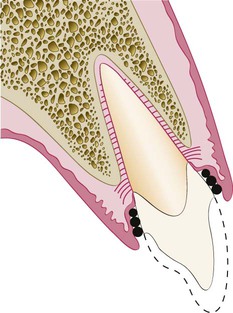
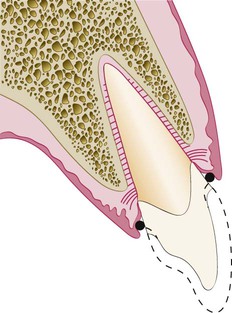
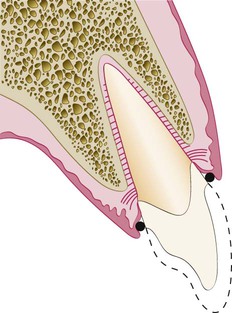
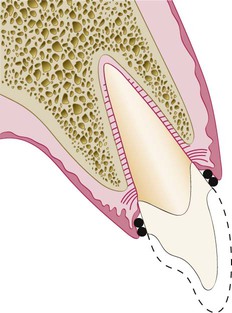
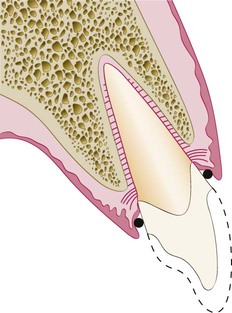
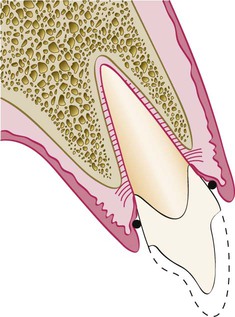
Restorative considerations frequently dictate the placement of restoration margins beneath the gingival tissue crest. Restorations may need to be extended gingivally (a) to create adequate resistance and retentive form in the preparation, (b) to make significant contour alterations because of caries or other tooth deficiencies, or (c) to mask the tooth–restoration interface by locating it subgingivally. When the restoration margin is placed too far below the gingival tissue crest, it impinges on the gingival attachment apparatus and create a violation of biologic width.49 Two different responses can be observed from the involved gingival tissues (Figure 67-4).
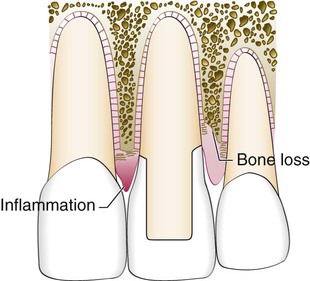
On the mesial surface of the left central incisor, bone has not been lost, but gingival inflammation occurs. On the distal surface of the left central incisor, bone loss has occurred, and a normal biologic width has been reestablished.
One possibility is that bone loss of an unpredictable nature and gingival tissue recession occurs as the body attempts to recreate room between the alveolar bone and the margin to allow space for tissue reattachment. This is more likely to occur in areas in which the alveolar bone surrounding the tooth is very thin in width. Trauma from restorative procedures can play a major role in causing this fragile tissue to recede. Other factors that may impact the likelihood of recession include (a) whether the gingiva is thick and fibrotic or thin and fragile and (b) whether the periodontium is highly scalloped or flat in its gingival form. It has been found that highly scalloped, thin gingiva is more prone to recession than a flat periodontium with thick fibrous tissue.47
Biologic Width Evaluation
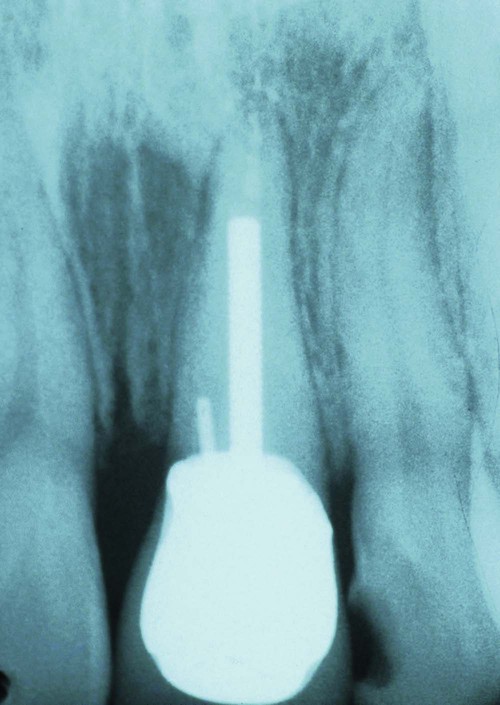
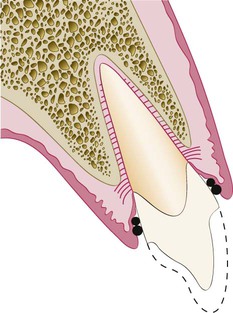
A more positive assessment can be made clinically by measuring the distance between the bone and the restoration margin using a sterile periodontal probe. The probe is pushed through the anesthetized attachment tissues from the sulcus to the underlying bone. If this distance is less than 2 mm at one or more locations, a diagnosis of biologic width violation can be confirmed. This assessment is completed circumferentially around the tooth to evaluate the extent of the problem. However, biologic width violations can occur in some patients in whom the margins are located more than 2 mm above the alveolar bone level.22 In 1994, Vacek et al70 also investigated the biologic width phenomenon. Although their average width finding of 2 mm was the same as that previously presented by Gargiulo et al,18 they also reported a range of different biologic widths that were patient specific. They reported biologic widths as narrow as 0.75 mm in some individuals, whereas others had biologic widths as tall as 4.3 mm (Figure 67-5).
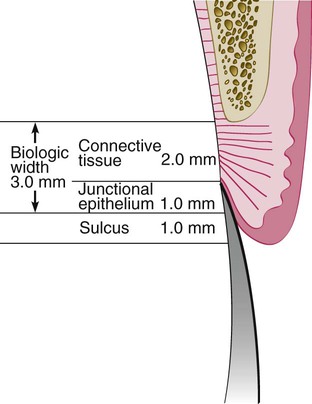
Connective tissue attachments and junctional epithelial attachments may be variable. In this example, the connective tissue attachment is 2 mm in height, the junctional epithelial attachment 1 mm in height, and the sulcus depth 1 mm, for a combined total tissue height above bone of 4 mm. However, the biologic width is 3 mm. This is just one variation that can occur from the average depicted in Figure 67-3.
Correcting Biologic Width Violations
Biologic width violations can be corrected either by surgically removing bone away from proximity to the restoration margin or by orthodontically extruding the tooth and thus moving the margin away from the bone. Surgery is the more rapid of the two treatment options.57 It is also preferred if the resulting crown lengthening creates a more pleasing tooth length. Indications and contraindications for surgical crown lengthening are presented in Chapter 66 and illustrated with clinical examples. In these situations, the bone should be moved away from the margin by the measured distance of the ideal biologic width for that patient, with an additional 0.5 mm of bone removed as a safety zone.
There is a potential risk of gingival recession after removal of bone.7 If interproximal bone is removed, there is a high likelihood of papillary recession and the creation of an unesthetic triangle of space below the interproximal contacts. If the biologic width violation is on the interproximal side, or if the violation is across the facial surface and the gingival tissue level is correct, orthodontic extrusion is indicated27 (Figures 67-6 to 67-9). The extrusion can be performed in two ways. By applying low orthodontic extrusion force, the tooth will erupt slowly, bringing the alveolar bone and gingival tissue with it. The tooth is extruded until the bone level has been carried coronal to the ideal level by the amount that needs to be removed surgically to correct the attachment violation. The tooth is stabilized in this new position and then is treated with surgery to correct the bone and gingival tissue levels. Another option is to perform rapid orthodontic extrusion where the tooth is erupted to the desired amount over several weeks.32 During this period, a supracrestal fiberotomy is performed circumferentially around the tooth weekly in an effort to prevent the tissue and bone from following the tooth. The tooth is then stabilized for at least 12 weeks to confirm the position of the tissue and bone, and any coronal creep can be corrected surgically.

The patient is unhappy with the appearance of the tissue surrounding the restoration (see Figures 67-7, 67-8, and 67-9).
Removal of interproximal bone would create an esthetic deformity. This patient is better treated with orthodontic extrusion (see Figures 67-6 and 67-8).

The tooth has been erupted 3 mm to move the bone and gingiva coronally 3 mm on the left central incisor. It is now possible to reposition the bone surgically to the correct level and position the gingiva to the correct level, reestablishing normal biologic width.
Margin Placement Guidelines
When determining where to place restorative margins relative to the periodontal attachment, it is recommended that the patient’s existing sulcular depth be used as a guideline in assessing the biologic width requirement for that patient. The base of the sulcus can be viewed as the top of the attachment, and therefore the clinician accounts for variations in attachment height by ensuring that the margin is placed in the sulcus and not in the attachment.4,36,37,56 The variations in sulcular probing depth are then used to predict how deep the margin can safely be placed below the gingival crest. With shallow probing depths (1.0 to 1.5 mm), extending the preparation more than 0.5 mm subgingivally risks violating the attachment. This assumes that the periodontal probe will penetrate into the junctional epithelial attachment in healthy gingiva an average of 0.5 mm. With shallow probing depths, future recession is unlikely because the free gingival margin is located close to the top of the attachment. Deeper sulcular probing depths provide more freedom in locating restoration margins farther below the gingival crest. In most circumstances, however, the deeper the gingival sulcus, the greater is the risk of gingival recession.
Clinical Procedures in Margin Placement
Rule 1: If the sulcus probes 1.5 mm or less, place the restoration margin 0.5 mm below the gingival tissue crest. This is especially important on the facial aspect and will prevent a biologic width violation in a patient who is at high risk in that regard.
Rule 2: If the sulcus probes more than 1.5 mm, place the margin half the depth of the sulcus below the tissue crest. This places the margin far enough below tissue, so that it will still be covered if the patient is at higher risk of recession.
Rule 3: If a sulcus greater than 2 mm is found, especially on the facial aspect of the tooth, evaluate to see if a gingivectomy could be performed to lengthen the teeth and create a 1.5-mm sulcus. Then the patient can be treated using Rule 1.
The rationale for Rule 3 is that deep margin placement is more difficult and the stability of the free gingival margin is less predictable when a deep sulcus exists. Reducing the sulcus depth creates a more predictable situation in which to place an intracrevicular margin. The clinician cannot be sure that the tissue will remain at the corrected level, however, because some gingival rebound can occur after gingivectomy. However, sulcular depth reduction ensures that the restorative margins will not be exposed and visible in the patient’s mouth (Figures 67-10 to 67-14).

She is unhappy with the exposed margins and notes that the margins were covered the day the restorations were placed (see Figures 67-11 to 67-14).
This patient in Figure 67-10 had an altered eruption pattern and a sulcus depth of more than 3 mm when these restorations were placed.


Note the tissue level and that the tissue is rebounding coronally over the margins. This is a common finding when a pure gingivectomy is done.

Note the tissue level has been maintained, with a sulcus depth of 2 mm on the facial surface.
The placement of supragingival or equigingival margins is simple because it requires no tissue manipulation. With regard to overall tooth preparation, the amount reduced incisally or occlusally, facially, lingually, and interproximally is dictated by the choice of restorative materials. Before extending subgingivally, the preparation should be completed to the free gingival margin facially and interproximally. This allows the margin of the tooth preparation to be used as a reference for subgingival extension once the tissue is retracted (Figure 67-15).
Tissue Retraction
Once the supragingival portion of the preparation is completed, it is necessary to extend below the tissue.6,23 The preparation margin must now be extended to the appropriate depth in the sulcus, applying the guidelines presented previously. In this process the tissue must be protected from abrasion, which will cause hemorrhage and can adversely affect the stability of the tissue level around the tooth. Access to the margin is also required for the final impression, with a clean, fluid-controlled environment. Tissue management is achieved with gingival retraction cords using the appropriate size to achieve the displacement required. Thin, fragile gingival tissues and shallow sulcus situations usually dictate that smaller diameter cords be chosen to achieve the desired tissue displacement.
For a Rule 1 margin (sulcus depth 1.5 mm or less), the cord should be placed so that the top of the cord is located in the sulcus at the level in which the final margin is to be established, which will be 0.5 mm below the previously prepared margin (Figure 67-16). On the interproximal aspects of the tooth, the cord is usually 1.0 to 1.5 mm below the tissue height because the interproximal sulcus is often 2.5 to 3.0 mm in depth. With this initial cord in place, the preparation is extended to the top of the cord, with the bur angled to the tooth so that it does not abrade the tissue (Figure 67-17). This process protects the tissue, creates the correct axial reduction, and establishes the margin at the desired subgingival level. To create space and allow access for a final impression, it is now necessary to pack a second retraction cord. The second cord is pushed so that it displaces the first cord apically and sits between the margin and the tissue (Figure 67-18). For the final impression, only the top cord is removed, leaving the margins visible and accessible to be recorded with the impression material (Figure 67-19). The initial cord remains in place in the sulcus until the provisional restoration is completed.
Here, a single cord has been placed 0.5 mm below the previously prepared margin.
This impression cord is placed so that it is between the margin of the preparation and the gingiva to create adequate space for impression material after removal of the cord.
The deflection cord is still in place maintaining the open sulcus but has been displaced apically another 0.5 mm by the placement of the impression cord, exposing tooth structure apical to the margin so that it can be captured in the impression.
As an alternative to additional retraction cords, electrosurgery can be used to remove any overlying tissue in the retraction process. A fine-wire electrode tip is held parallel to the tooth and against the margin in the sulcus and moved through the overhanging tissue, opening up the margin and the retraction cord to visual access (Figures 67-20 to 67-23). The electrosurgery tip sits on top of the retraction cord in place in the sulcus. This controls the vertical position of the tip and results in the removal of the least tissue needed for access.

The soft tissue is falling over the margins of the preparation. In this situation, if the impression cord were removed, the impression would not capture the margins in the areas in which the tissue is overhanging.

Note that the deflection cord and the impression cord are still in place. The impression cord is now visible completely around the tooth, allowing easy access for the impression material to the margin after removal of the impression cord.


Note the first cord, or deflection cord, is still in place.
For Rule 2 situations in which the sulcus is deeper, two larger-diameter cords are used to deflect the tissue before extending the margin apically (Figures 67-24 to 67-26). The top of the second cord is placed to identify the final margin location at the correct distance below the previously prepared margin, which was at the gingival tissue crest level. The margin is lowered to the top of the second cord (Figure 67-27), then a third cord is placed in preparation for the impression (Figures 67-28 and 67-29). In the patient with a deep sulcus in which the margin may be 1.5 to 2.0 mm below the tissue crest, electrosurgery is often required to remove overhanging tissue. To avoid altering the gingival tissue height, it is important to hold the electrosurgery tip parallel to the preparation (Figure 67-30).
Note that the placement of a single deflection cord does not provide adequate deflection of the tissue to allow the margin to be carried below tissue without abrading the gingiva with the bur.
Combined, these two cords allow adequate deflection to open up the sulcus so that the margin can be carried below tissue without abrading the gingiva.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses