Advanced Implant Surgical Procedures
The high predictability of endosseous dental implants has led to routine use and an expectation for success. However, the ultimate success for any patient or any particular implant relies on several factors, the most important of which is the availability of bone. The loss of teeth, whether caused by disease or trauma, can result in severe deficiency of the alveolar bone. Horizontal bone deficiencies are managed quite predictably with localized bone augmentation procedures (see Chapter 76). However, vertical bone deficiencies are much more challenging. The edentulous posterior maxilla is challenging as the result of a general lack of bone volume and the omnipresent poor bone quality of the area; that is, posterior maxillary bone often consists of a thin cortical shell filled with sparse trabecular bone. Edentulous sites, in any anatomic location, that have suffered significant vertical alveolar bone loss are especially challenging to reconstruct.
Maxillary Sinus Elevation and Bone Augmentation
Rehabilitation of the edentulous posterior maxilla with endosseous dental implants often represents a clinical challenge because of insufficient bone volume resulting from pneumatization of the maxillary sinus and resorption or loss of alveolar crestal bone. Before the utilization of bone augmentation procedures, patients with missing teeth and deficient bone in the posterior maxilla could only be rehabilitated with removable prostheses, short implants, or cantilevered restorations (i.e., supported by adjacent teeth or implants). Historically, the failure rate for implants in the posterior maxilla has been significantly higher than failure rates for implants in all other anatomic locations.17 Consequently, procedures such as the maxillary sinus elevation and bone augmentation are needed to increase the amount of vertical bone height in the posterior maxilla for the placement of implants (see Video 77-1: Crestal Window Technique with Immediate Implant Placement).![]()
In 1980, Boyne and James4 first described a procedure to graft the maxillary sinus floor with autogenous marrow and bone for placing an implant (blade type). Access to the maxillary sinus was gained through a “Caldwell-Luc” procedure (i.e., an opening into the maxillary sinus created at the anterior–superior aspect). Since then several other techniques have been described, including variations on the lateral window osteotomy and a variety of techniques to lift the sinus floor from a crestal approach.
Various bone graft materials have been used to augment the maxillary sinus. The 1996 Consensus Conference on Maxillary Sinus Bone Grafting reviewed available data and concluded that allografts, alloplasts, and xenografts, alone or in combination with autogenous bone, can be effective as bone substitute graft materials for sinus bone augmentation.18 More importantly, it was concluded that the sinus graft procedure with implant placement is a highly predictable and effective therapeutic modality for the rehabilitation of the posterior maxilla. Sinus floor elevation with bone augmentation of the maxillary sinus is now a well-accepted procedure used to increase bone volume in the posterior maxilla. Numerous reports have validated the safety and efficacy of this procedure.7,10,12,42 Implant success rates are equal to or better than that of implants placed in nongrafted maxillary bone (i.e., areas of the posterior maxilla with adequate height of existing native bone).42 Thus bone augmentation of the maxillary sinus is a viable option for the vertically deficient posterior maxilla in which the interocclusal dimension is normal or only moderately increased.
Indications and Contraindications
Contraindications to maxillary sinus elevation and bone augmentation are similar to contraindications for other surgical procedures, with the added consideration of the maxillary sinus (Box 77-1). Patients must be in good general health and free of diseases that affect the maxilla or maxillary sinus. Local factors that are considered contraindications to maxillary sinus elevation and bone augmentation include the presence of tumors, maxillary sinus infection, severe chronic sinusitis, scar or deformity of the sinus cavity from previous surgery, dental infection, severe allergic rhinitis, and chronic use of topical steroids. Systemic contraindications to treatment include radiation therapy, uncontrolled metabolic disease (e.g., diabetes), excessive tobacco use, drug or alcohol abuse, and psychologic or mental impairment.
Surgical Procedures for Sinus Elevation
The maxillary sinus bone augmentation procedure was first described in the 1960s by Boyne (unpublished oral presentations to United States Navy Dental postgraduates, 1965-1968) and originally used as a preprosthetic surgical procedure for patients with large tuberosities and pneumatized sinuses.3 To reduce the size of the tuberosity without creating an oral-antral defect, bone was grafted into the sinus cavity to increase the volume of bone within the maxillary tuberosity. After a period of healing, the tuberosity was able to be reduced surgically from the alveolar ridge crest. As stated earlier, Boyne and James4 were the first to describe the use of the maxillary sinus bone-grafting procedure for placement of an implant (blade type) to retain a prosthesis. Greater use and further development of this procedure evolved along with the success of endosseous dental implants and the desire to replace missing posterior maxillary teeth with implant-retained restorations.
Presurgical Evaluation of Maxillary Sinus.
Presurgical evaluation of the maxillary sinus is primarily accomplished using radiographic examination techniques (Figure 77-1). Several observations about the anatomy can be made with a periapical or panoramic projection, but the internal anatomy is more accurately assessed with a three-dimensional scan, such as computed tomography (CT) or cone-beam CT (CBCT) scan. The maxillary sinus should be evaluated for any pathology, masses, or the presence of septa. If three-dimensional scans are available, the lateral wall should also be evaluated for the presence of medium or large intraosseous vascular channels (see Figure 54-15). Medium- to large-sized vessels occasionally traverse the lateral wall of the maxillary sinus, and identifying them is helpful in avoiding a bleeding problem during surgery (see Chapter 54).25
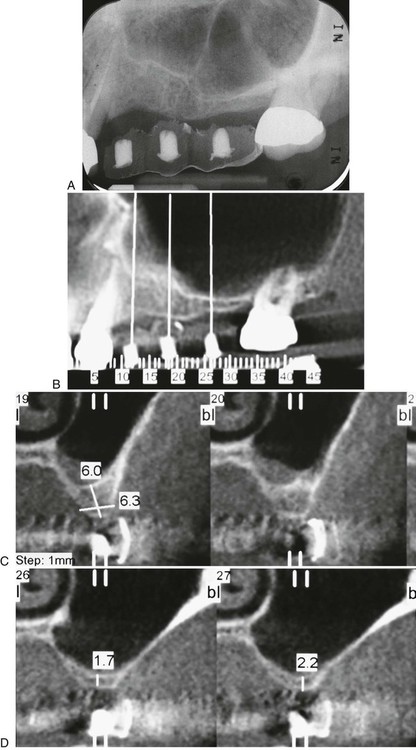
A, Periapical radiograph. B, Panoramic projection from cone-beam scan. Note the presence of maxillary septa in the premolar region. C, Cross-sectional image in premolar region showing about 6 mm of bone height and presence of maxillary septa. D, Cross-sectional image in molar region showing about 2 mm of bone height.
Simultaneous Implant Placement.
Simultaneous implant placement is possible with sinus elevation and bone augmentation procedures as long as the implant can be stabilized in the desired location with the existing native bone (Figure 77-2).
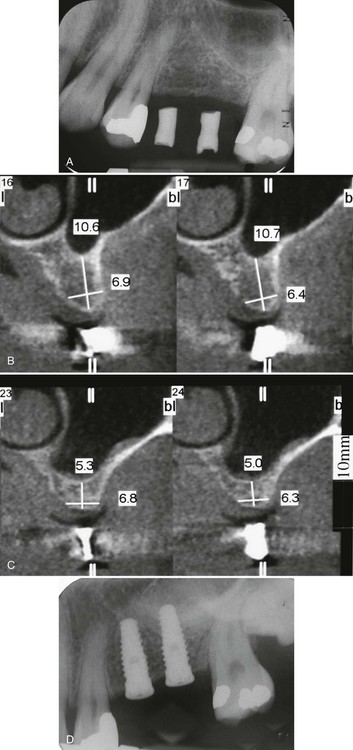
A, Preoperative periapical radiograph. B, Preoperative, cross-sectional image in premolar region demonstrating 10.6 mm of vertical bone height. C, Preoperative, cross-sectional image in molar region demonstrating 5.3 mm of vertical bone height. D, Postsurgical radiograph of graft and implants in place.
It has been suggested that a minimum of 5 mm of existing native bone in the alveolar crest is required for simultaneous implant placement. However, some clinicians claim that it is possible to place implants simultaneously with as little as 1 mm of remaining bone.23,48 The most important factor in determining whether implant(s) can be placed at the time of sinus bone augmentation is the ability to achieve implant stability in the existing bone rather than any measure of bone height. Factors that influence implant stability include bone height, bone quality, precision of osteotomy preparation, and the surgeon’s skill and experience. If inadequate native bone exists to place implants at the time of the bone augmentation procedure, they can be placed at a subsequent surgery after an appropriate healing period (Figure 77-3).
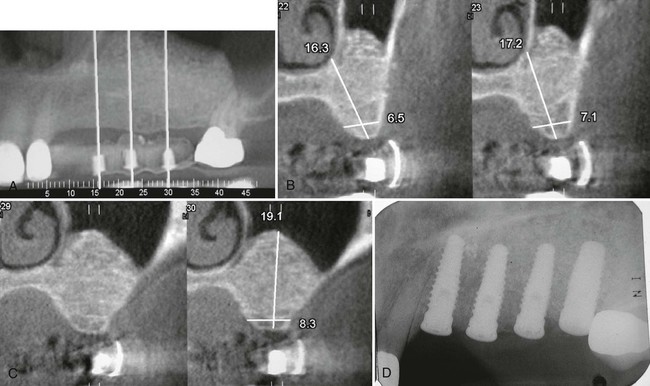
Same patient as in Figure 77-1. See preoperative radiograph and preoperative cross-sectional images. A, Postsurgical panoramic view of bone-augmented maxillary sinus. The maxillary left cuspid has been extracted because of a vertical fracture. B, Postsurgical cross-sectional image in premolar region demonstrating more than 17-mm vertical bone height. C, Postsurgical cross-sectional image in molar region demonstrating 19.1-mm vertical bone height. D, Postsurgical radiograph of implants placed in the previously grafted maxillary sinus (and cuspid site).
Bone Graft Materials.
Autogenous bone is often considered the “gold standard” for bone augmentation because of its osteoconductive, osteoinductive, and osteogenic properties.4 However, harvesting autogenous bone from intraoral or extraoral locations creates a second surgical site with additional morbidity. Numerous studies have demonstrated clinical success using many variations of bone graft materials and combinations.18,42
Several recent clinical studies and reports have attempted to evaluate the maxillary sinus augmentation procedures using a variety of bone-grafting materials, including autogenous bone from the iliac crest or oral cavity and bone substitutes such as freeze-dried demineralized bone, resorbable and nonresorbable hydroxyapatite, and xenografts. However, only a few studies have critically evaluated the long-term clinical outcome of this procedure, and most have used a small study population. Short- to long-term clinical studies of dental implants placed into grafted sinuses demonstrate an equivalent or higher survival rate as compared to implants placed in native maxillary bone (i.e., without the need of sinus augmentation).18,42 The results of these studies support the clinical predictability of maxillary sinus augmentation procedures for the rehabilitation of the edentulous posterior maxilla with implant-supported prostheses (Figure 77-4).
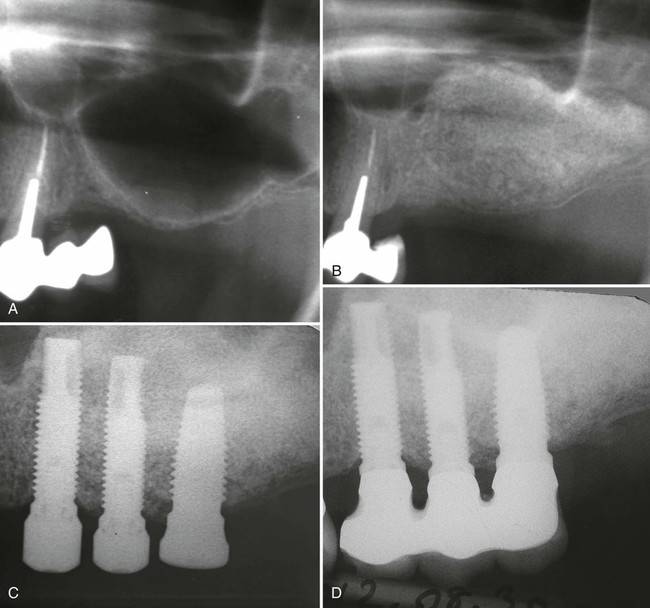
A, Preoperative radiograph demonstrates minimal residual crestal bone height. B, Postoperative radiograph demonstrates sinus graft healing after 6 months. C, Abutment connection of implants after 6 months of submerged healing. The three distal implants were placed into augmented bone. D, Periapical radiograph demonstrates stability of crestal bone around implants at 10 years loading. (From Urban IA, Lozada JL. A prospective study of implants placed in augmented sinuses with minimal and moderate residual crestal bone: results after 1 to 5 years. Int J Oral Maxillofac Implants. 25(6):1203-12, 2010.)
The use of bone-substitute graft materials can reduce the morbidity introduced by a second surgical site while maintaining equally good implant success rates.18 Anorganic bovine bone-derived mineral (ABBM; ABBM has also been referred to in the literature as deproteinized bovine bone mineral, deproteinized anorganic bovine bone, and anorganic bovine bone) has also been used successfully for sinus augmentation.46 This graft material has demonstrated good dimensional stability and high implant survival rates.10 These materials form an osteoconductive scaffold for bone growth but do not have any osteoinductive properties. A possible exception is demineralized freeze-dried bone allograft (DFDBA). This material has demonstrated osteoinductive potential but has not proved to be particularly advantageous in the maxillary sinus bone augmentation.18,45 In fact, the bone volume gained with the use of DFDBA is less than that achieved with mineralized graft materials as a result of moderate postoperative shrinkage of DFDBA-grafted bone.
Crestal Osteotomy Technique.
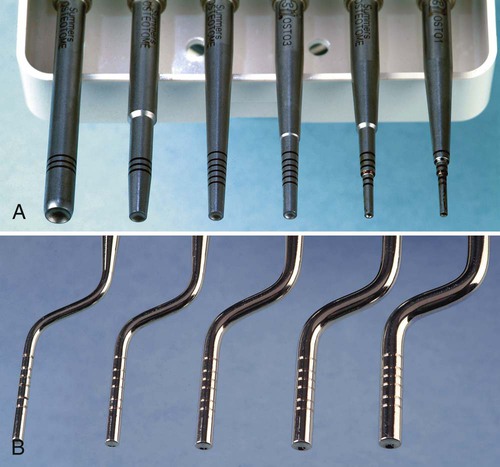
In cases with moderate bone height (e.g., 7 to 9 mm) that require limited sinus bone augmentation, a crestal approach to elevation may be desirable. The osteotome technique is a procedure that uses osteotomes (Figure 77-5) to compress bone (internally from the alveolar crest upward) against the floor of the sinus, ultimately leading to a controlled “inward fracture” of the sinus floor bone and the schneiderian membrane, which should remain intact above the inward-fractured bone.
The osteotome sinus floor elevation technique was described by Summers.35,36 It is considered to be a “conservative” approach to sinus elevation, but it is also a “blind” technique because it does not allow the operator to visualize the schneiderian membrane during the osteotomy. For this reason, it is a technique-sensitive procedure as well (i.e., the operator must “feel” the bone fracture and the membrane elevation). Verification of success can only be observed with radiographs and visualization of the bone graft material in the sinus cavity.
Procedure.
An osteotomy site is prepared with a series of drills (e.g., initial drills used for implant site preparation) to a depth that is approximately 1 to 2 mm from the floor of the maxillary sinus. Osteotomes are used to increase compressive forces gradually against the floor of the sinus by adding incremental quantities of graft material until the floor of the sinus fractures inward (Figure 77-6). After the controlled inward fracture of the maxillary sinus floor, bone graft materials continue to be slowly introduced, through the osteotomy site and into the maxillary sinus, which continues to elevate the membrane and thus allows a vertical expansion of the bone height in a localized area of the maxillary sinus. Once the sinus membrane is elevated with bone graft material to the desired height, the implant osteotomy can be completed, with a final drill used to finish preparation of the site, and an implant can be inserted. Multiple individual sites can be elevated and prepared simultaneously through separate osteotomy sites.
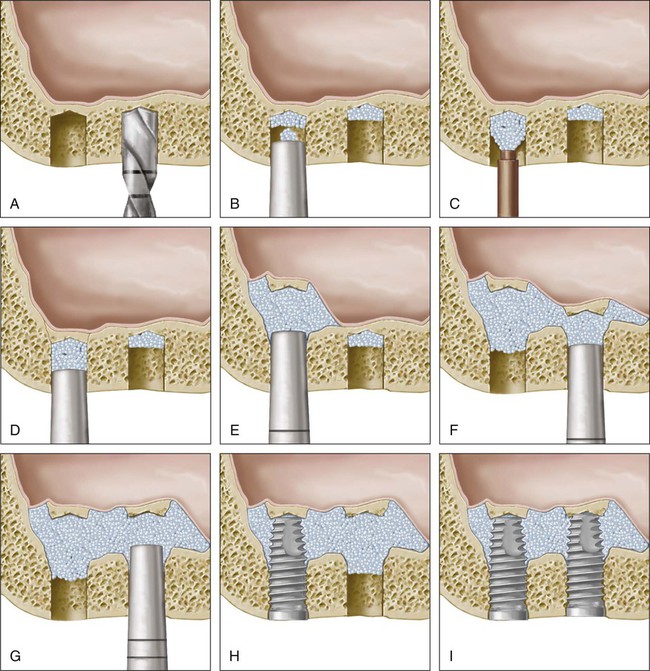
A, Osteotomy prepared with drills to a depth that is near the maxillary sinus floor. B, Graft material introduced into osteotomy and condensed with osteotome. C, Additional bone graft material is added to the osteotomy. D, Bone graft continues to be condensed by osteotomes. E, This process is continued until floor of sinus is “fractured” up internally and the floor is lifted with the bone graft material. F, Continuation of process shown in E for second site. G, Bone graft material continues to be added gradually to both sites with osteotome condensation to elevate the schneiderian membrane away from the bone (maxillary sinus walls) until sufficient height and volume are created for the placement of implants. H, The coronal aspect of the osteotomy is carefully prepared for the placement of implants (instrumentation not shown) and the implant is placed. I, Final view of two implants placed in the grafted m/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses