Chapter 7
Pulmonary Disease
Chronic obstructive pulmonary disease (bronchitis and emphysema) and asthma are common pulmonary diseases that cause obstruction in airflow. They are discussed in this chapter along with tuberculosis (TB), the most prevalent contagious disease in the world.
Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease (COPD) is a general term for pulmonary disorders characterized by chronic airflow limitation from the lungs that is not fully reversible. COPD encompasses two main diseases: chronic bronchitis and emphysema. Chronic bronchitis is defined as a condition associated with excessive tracheobronchial mucus production (at the bronchial level) sufficient to cause a chronic cough with sputum production for at least 3 months in at least 2 consecutive years in a patient in whom other causes of productive chronic cough have been excluded. Emphysema is defined as the presence of permanent enlargement of the air spaces distal to the terminal bronchioles accompanied by destruction of alveolar walls or septa (at the acinar level) without obvious fibrosis.< ?xml:namespace prefix = "mbp" />
Epidemiology
COPD is the third leading cause of death in the United States and is estimated to affect more than 24 million people. COPD affects approximately 8% of adults and 14% of older adults in the United States.
Etiology
Worldwide, the most important cause of COPD is tobacco smoking. Approximately 12.5% of current smokers and 9% of former smokers have COPD.
Pathophysiology and Complications
Chronic exposure to cigarette smoke induces pathophysiologic responses of the airways and lung tissue. Chronic bronchitis involves the large and small airways. In the large airways, tobacco smoke and irritants induce thickened bronchial walls with inflammatory cell infiltrate, increased size of the mucous glands, and goblet cell hyperplasia. Obstruction is exacerbated in the small airways by narrowing, scarring, increased sputum production, mucous plugging, and collapse of peripheral airways resulting from the loss of surfactant

FIGURE 7-1 Gross pathologic specimen shows lung changes (thickened bronchial walls, narrowing of small airways) due to chronic bronchitis.
(Courtesy McLay RN, et al: Tulane gross pathology tutorial, Tulane University School of Medicine, New Orleans, Louisiana, 1997.)
Emphysematous changes occur as chronic smoke inhalation injures lung parenchyma. The alveolar epithelium is damaged, causing a release of inflammatory mediators that attract activated macrophages and neutrophils. These inflammatory cells release enzymes (elastase) that destroy the alveolar walls, resulting in enlarged air spaces distal to the terminal bronchioles and loss of elastic recoil of the lungs (
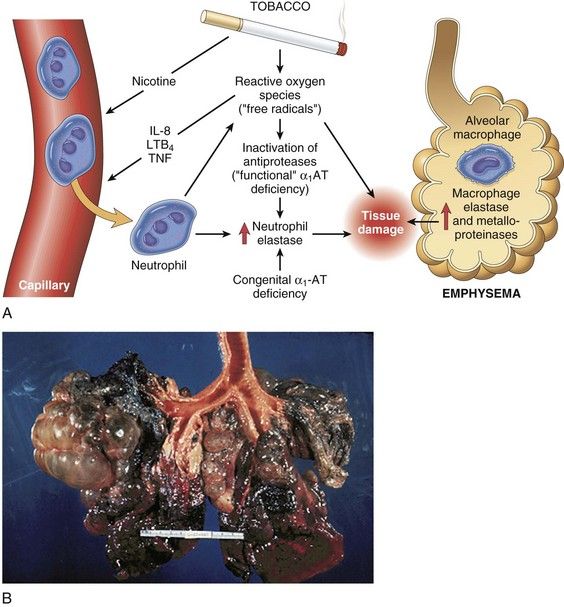
FIGURE 7-2 A, Pathogenesis of emphysema involving imbalance in proteases-antiproteases that results in tissue damage and collapse of alveoli. B, Gross pathologic specimen of an emphysemic lung.
(A, From Kumar V, Abbas A, Fausto N, editors: Robbins & Cotran pathologic basis of disease, ed 8, Philadelphia, 2010, Saunders. B, Courtesy McLay RN, et al: Tulane gross pathology tutorial, Tulane University School of Medicine, New Orleans, Louisiana, 1997.)
COPD usually is progressive, and the course is one of deterioration and periodic exacerbations, unless intervention is provided early in its onset.
Clinical Presentation
Signs and Symptoms
The onset phase of COPD takes many years in most patients and usually begins after age 40. Symptoms develop slowly, and many patients are unaware of the emerging condition. Key indicators are a chronic cough with sputum production that may be intermittent, unproductive or productive, scanty or copious, and dyspnea that is persistent and progressive or worsens with exercise. As the disease progresses, weight loss and decreased exercise capacity also are seen. Comorbid conditions include cardiovascular disease, respiratory infections, osteoporosis, and fractures.
Traditional teaching presented patients who had chronic bronchitis as sedentary, overweight, cyanotic, edematous, and breathless; accordingly, they were known as “blue bloaters.” Patients diagnosed with emphysema were traditionally known as “pink puffers” because they demonstrated enlarged chest walls for a “barrel-chested” appearance, weight loss with disease progression, severe exertional dyspnea with a mild nonproductive cough, lack of cyanosis, and pursing of the lips with efforts to forcibly exhale air from the lungs. Currently, it is recognized that most patients with COPD may exhibit features of both diseases (

Box 7-1 Predominant Findings in Patients with Chronic Obstructive Pulmonary Disease
History: Exposure to risk factors
Clinical: Cough, sputum production, exertional dyspnea
Laboratory: Spirometry revealing airflow limitation, blood gas abnormalities
Imaging: Chest radiograph/computed tomography scan revealing prominent bronchovascular markings and/or evidence of hyperinflation

Laboratory Findings
Diagnosing COPD in its early stages can be difficult, but the possibility of this clinical entity should be considered in any patient who experiences dyspnea with previously tolerated activities and demonstrates chronic cough with or without sputum production, as well as exposure to risk factors, especially cigarette smoking. Measures of expiratory airflow are the key diagnostic procedures performed. Forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV1) are determined by spirometry—a simple objective test that measures the amount of air a person can breathe out (
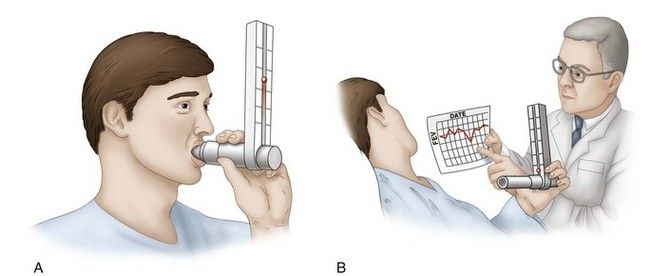
FIGURE 7-3 A, Measure of forced expiratory volume by spirometry. B, Discussion of daily spirometry results with physician.

Box 7-2 Stages of Chronic Obstructive Pulmonary Disease
Stage I—mild COPD: defined by an FEV1/FVC ratio of less than 70% and an FEV1 of 80% or more of that predicted
Stage II—moderate COPD: worsening airflow limitation and FEV1/FVC less than 70% and FEV1 of 50% to less than 80% predicted
Stage III—severe COPD: FEV1/FVC less than 70% and FEV1 of 30% to less than 50% predicted, with further worsening of airflow limitation
Stage IV—very severe COPD: FEV1/FVC less than 70%; FEV1 less than 30% predicted, with chronic respiratory failure and exacerbations that may be life-threatening

Arterial blood gas measurement and chest radiographs aid in the diagnosis. Patients with chronic bronchitis have an elevated partial pressure of carbon dioxide (Pco2) and decreased partial pressure of oxygen (Po2) (as measured by arterial blood gases), leading to secondary erythrocytosis, an elevated hematocrit value, and compensated respiratory acidosis. Patients with emphysema have a relatively normal (Pco2) and a decreased (Po2), which maintain normal hemoglobin saturation, thus avoiding erythrocytosis. Total lung capacity and residual volume are markedly increased. The ventilatory drive of hypoxia also is reduced in both types of COPD.
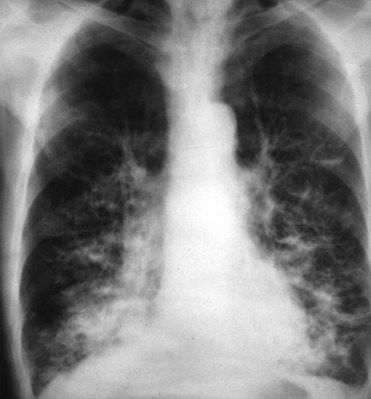
Chest radiographs and computed tomography scans assist in classifying COPD and identifying comorbid conditions. In chronic bronchitis, typical radiographic abnormalities consist of increased bronchovascular markings at the base of the lungs (
Medical Management
Management of COPD includes smoking cessation, influenza and pneumococcal vaccinations, and use of short- and long-acting bronchodilators. Other recommended measures include regular exercise, good nutrition, and adequate hydration. Use of bronchodilator drugs are recommended in a stepwise manner, as shown in
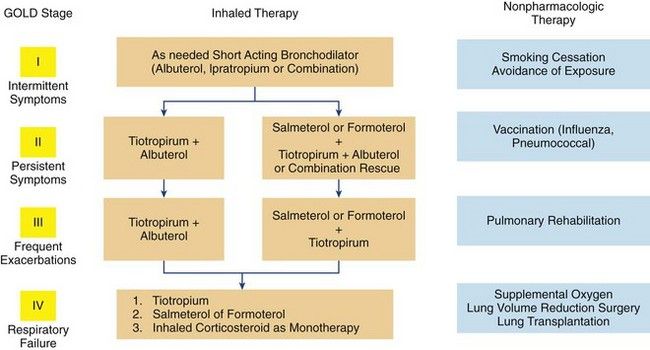
FIGURE 7-5 Clinical algorithm for treatment based on Global Initiative for Chronic Obstructive Lung Disease (GOLD) stages.
(Redrawn from Cooper CB, Tashkin DP: Recent developments in inhaled therapy in stable chronic obstructive pulmonary disease, BMJ 330:640-644, 2005.)
TABLE 7-1 Drugs Used in Outpatient Management of Chronic Obstructive Pulmonary Disease (COPD) and Asthma
| Drug | Trade Name | Dental Treatment Considerations |
|---|---|---|
| Antiinflammatory Drugs | ||
| Corticosteroids—Inhaled | ||
| Beclomethasone dipropionate | Vanceril, Beclovent | Not intended for acute asthma attack; may contribute to the development of oral candidiasis if used improperly or excessively |
| Budesonide | Pulmicort | |
| Dexamethasone | Decadron | |
| Flunisolide | AeroBid | |
| Fluticasone propionate | Flonase | |
| Triamcinolone acetonide | Azmacort | |
| Corticosteroids—Systemic | ||
| Prednisone | Deltasone or generic | Not intended for acute asthma attack; possible adrenal suppression, cushingoid features with long-term use |
| Prednisolone | Delta-Cortef | |
| Methylprednisolone | Solu-Medrol | |
| Antileukotrienes | ||
| 5-Lipoxygenase Inhibitor | Not intended for acute asthma attack | |
| Zileuton | Zyflo | |
| Leukotriene D4 Receptor Antagonists | ||
| Zafirlukast (Accolate) | ||
| Montelukast | Singulair | |
| Nonsteroidal—Chromones | ||
| Cromolyn sodium | Intal inhaler | Not intended for acute asthma attack |
| Nedocromil | Tilade inhaler | |
| β-Adrenergic Bronchodilators | ||
| Fast-Acting Nonselective β–Agonist Inhalers | ||
| Epinephrine |
Primatene Mist, Bronkaid (available in parenteral form also) |
For use during acute asthma attack |
| Ephedrine |
Eted II | |
| Intermediate-Acting Nonselective β-Agonist Inhalers (3 to 6 hours) | ||
| Isoproterenol |
Isuprel | Not best choice for use during acute asthma attack |
| Isoetharine | Bronkosol | |
| Metaproterenol |
Alupent, Metaprel, others | |
| β2-Selective Agonist Inhalers | ||
| Albuterol |
Proventil, Ventolin | For use during acute asthma attack |
| Bitolterol mesylate | Tornalate | |
| Fenoterol | Berotec | |
| Levalbuterol | Xopenex | |
| Pirbuterol | Maxair, Maxair | |
| Autohaler | ||
| Terbutaline |
Brethaire, Bricanyl | |
| Long-Acting β2-Selective Agonist Inhalers (>12 hours) | ||
| Salmeterol (slow onset, long duration) | Serevent | Not intended for acute asthma attack |
| Formoterol (rapid onset, long duration) | Foradil | |
| Anticholinergic Bronchodilators (Quaternary Ammonium Derivatives of Atropine) | ||
| Ipratropium bromide Tiotropium (long-acting) |
Atrovent Spiriva |
Not intended for acute asthma attack; generally used in combination with other antiasthma drugs |
| Phosphodiesterase (PD) Inhibitors | ||
| Theophylline (nonselective) | Theo-Dur | Adverse drug interaction with erythromycin and azithromycin; serum drug levels should be monitored for toxicity |
| Roflumilast (selective PD-4) | Daxas, Daliresp | Adverse effects of headache, coughing may affect diagnostic workup and treatment |
| Cilomilast (selective PD-4) | Ariflo | |
Injectable α1-proteinase inhibitor formulations (Aralast, Prolastin, Zemaira) are available for treatment of emphysema due to inherited α1-antitrypsin deficiency.
‡ Inhalation, oral, and parenteral.
§ Inhalation and oral. Some combination drugs are formoterol + budesonide propionate (Symbicort) and salmeterol + fluticasone propionate (Advair).
Bronchodilators serve as the cornerstone of management, with inhaled and regular therapy preferred. The primary inhaled agents are short- and long-acting anticholinergics (e.g., ipratropium, tiotropium) that reduce glandular mucus and relax smooth muscle by blocking acetylcholine at the muscarinic receptors; and short- and long-acting β2-adrenergic bronchodilators that relax smooth muscle by increasing cyclic adenosine monophate levels. Combining bronchodilators can lead to pronounced benefits, because they work by different mechanisms. Inhaled corticosteroids are added to the regimen for symptomatic patients at stage III or above who have repeated exacerbations.
Antibiotics are used for pulmonary infections, and low-flow supplemental O2 (2 L/minute) is recommended when the patient’s Po2 is 88% or less.
Dental Management
Prevention of Potential Problems
Most patients with COPD have a history of smoking tobacco. Dental health care providers can make an important contribution to the management of patients with COPD by encouraging those who smoke to quit. By providing information on the diseases associated with smoking, dental health providers may help patients to start thinking seriously about giving up the habit. Many interventional approaches (e.g., nicotine replacement, bupropion therapy) are available, and providers should help the patient implement the method with which they feel most comfortable (see
Before initiating dental care, clinicians should assess the severity of the patient’s respiratory disease and the degree to which it has been controlled. A patient coming to the office for routine dental care who displays shortness of breath at rest, a productive cough, upper respiratory infection, or an oxygen saturation level less than 91% (as determined by pulse oximetry) is unstable. Accordingly, the appointment should be rescheduled and an appropriate referral for medical attention should be made. If the patient is stable and the breathing is adequate, efforts should be directed toward the avoidance of anything that could further depress respiration (

Box 7-3 Dental Management
Considerations in Patients with Chronic Obstructive Pulmonary Disease (COPD)
Patient Evaluation/Risk Assessment (see
• Evaluate and determine whether COPD is present.
• Obtain medical consultation if the condition is poorly controlled (as manifested by dyspnea, coughing, or frequent upper respiratory infections) or undiagnosed, or if the diagnosis is uncertain. Review history and clinical findings for concurrent heart disease.
Potential Issues/Factors of Concern
| A | |
| Analgesics | No issues. |
| Antibiotics | Avoid erythromycin, macrolide antibiotics, and ciprofloxacin in patients taking theophylline. In patient who has received courses of antibiotics for upper respiratory infections, oral and lung flora may include antibiotic-resistant bacteria. |
| Anesthesia | Local anesthesia can be used without change in technique. Avoid outpatient general anesthesia. |
| Anxiety | Avoid nitrous oxide–oxygen inhalation sedation in patients with severe (stage 3 or worse) COPD. Consider low-dose oral diazepam or another benzodiazepine, although these agents may cause oral dryness. |
| Allergy | No issues. |
| B | |
| Bleeding | No issues. |
| Blood pressure | Patients with COPD can have cardiovascular comorbidity. Assess blood pressure. |
| C | |
| Chair position | Semisupine or upright chair position may be better for treatment in these patients. |
| D | |
| Devices | Avoid use of rubber dam in patients with severe disease. Use pulse oximetry to monitor oxygen saturation. Spirometry readings are helpful in determining level of control. |
| Drugs | Avoid use of barbiturates and narcotics, which can depress respiration. Avoid use of antihistamines and anticholinergic drugs because they can further dry mucosal secretions. Supplemental steroids are unlikely to be needed to perform routine dental care; the usual morning corticosteroid dose should be taken on the day of surgical procedures. |
| E | |
| Equipment | Monitor oxygen saturation with pulse oximeter during sedation and invasive procedures. Use low-flow (2 to 3 L/minute) supplemental O2 when oxygen saturation drops below 95%; it may become necessary when oxygen saturation drops below 91%. |
| Emergencies | No issues. |
| F | |
| Follow-up | At each follow-up appointment, encourage patient to quit smoking, and examine oral cavity for lesions that may be related to smoking. Avoid treatment if upper respiratory infection is present. |

No contraindication to the use of local anesthetic has been identified. However, the use of bilateral mandibular blocks or bilateral palatal blocks can cause an unpleasant airway constriction sensation in some patients. This concern may be more important in the management of a patient with severe COPD with a rubber dam, or when medications are administered that dry mucous secretions. Humidified low-flow O2 can be provided to alleviate the unpleasant airway feeling produced by nerve blocks, use of a rubber dam, and/or medications.
If sedative medication is required, low-dose oral diazepam (Valium) may be used. Nitrous oxide–oxygen inhalation sedation should be used with caution in patients with mild to moderate chronic bronchitis. It should not be used in patients with severe COPD and emphysema, because the gas may accumulate in air spaces of the diseased lung. If this sedation modality is used in the patient with chronic bronchitis, flow rates should be reduced to no greater than 3 L/minute, and the clinician should anticipate induction and recovery times with nitrous oxide approximately twice as long as those in healthy patients.
Patients with COPD often have comorbid conditions such as hypertension and coronary heart disease that require dental management considerations (see
Treatment Planning Modifications
No technical treatment planning modifications are required in patients with COPD.
Oral Complications and Manifestations
Patients with COPD who are chronic smokers have an increased likelihood of developing halitosis, extrinsic tooth stains, nicotine stomatitis, periodontal disease, premalignant mucosal lesions, and oral cancer. Anticholinergics are associated with dry mouth. In rare instances, theophylline has been associated with the development of Stevens-Johnson syndrome.
Asthma
Definition
Asthma is a chronic inflammatory disease of the airways characterized by reversible episodes of increased airway hyperresponsiveness resulting in recurrent episodes of dyspnea, coughing, and wheezing.
Epidemiology
Incidence and Prevalence
Asthma affects 300 million persons worldwide and accounts for 1 of every 250 deaths worldwide. In the United States, its prevalence has more than doubled since the 1960s, from about 2% to 7% or greater (affecting 23 million people).
Etiology
Asthma is a multifactorial and heterogeneous disease whose exact cause is not completely understood. Its development requires interaction between the environment and genetic susceptibility, with clinical manifestations resulting from dysfunction of the airway epithelium, smooth muscle, immune cells, and neuronal elements. Many triggers of asthma are recognized; these factors traditionally have been grouped into one of four categories based on pathophysiology: extrinsic (allergic or atopic), intrinsic (idiosyncratic, nonallergic, or nonatopic), drug-induced, and exercise-induced. Today, from a management perspective, the type of trigger is more important than the category.
Allergic or extrinsic asthma is the most common form and accounts for approximately 35% of all adult cases. It is an exaggerated inflammatory response that is triggered by inhaled seasonal allergens such as pollens, dust, house mites, and animal danders. Allergic asthma usually is seen in children and young adults.
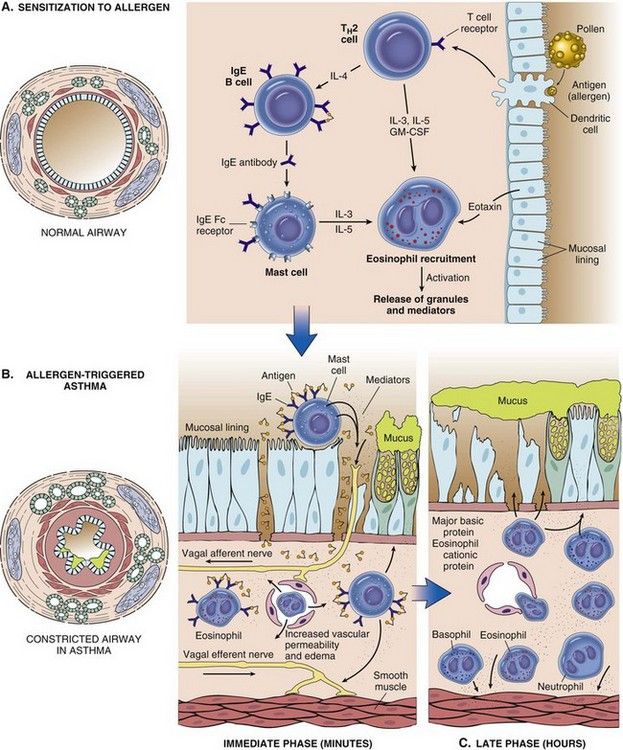
FIGURE 7-6 Processes involved in allergic (extrinsic) asthma.
(From Kumar V, Abbas A, Fausto N, editors: Robbins & Cotran pathologic basis of disease, ed 8, Philadelphia, 2010, Saunders.)
Intrinsic asthma accounts for about 30% of asthma cases and seldom is associated with a family history of allergy or with a known cause. Patients usually are nonresponsive to skin testing and demonstrate normal IgE levels. This form of asthma generally is seen in middle-aged adults, and its onset is associated with endogenous factors such as emotional stress (implicated in at least 50% of affected persons), gastroesophageal acid reflux, or vagally mediated responses.
Ingestion of drugs (e.g., aspirin, nonsteroidal antiinflammatory drugs, beta blockers, angiotensin-converting [ACE] enzyme inhibitors) and some food substances (e.g., nuts, shellfish, strawberries, milk, tartrazine food dye yellow color no. 5) can trigger asthma.
Metabisulfite preservatives of foods and drugs (specifically in local anesthetics containing epinephrine) may cause wheezing when metabolic levels of the enzyme sulfite oxidase are low.
Exercise-induced asthma is stimulated by exertional activity. Although the pathogenesis of this form of asthma is unknown, thermal changes during inhalation of cold air provoke mucosal irritation and airway hyperactivity. Children and young adults are more severely affected because of their high level of physical activity.
Infectious asthma is a term previously used to describe persons who developed asthma because of the inflammatory response to bronchial infection. Now it is recognized that several respiratory viral infections during infancy and childhood can result in the development of asthma. Also, causative agents of respiratory infections (bacteria, dermatologic fungi I Trichophyton), and Mycoplasma organisms) can exacerbate asthma. Treatment of the respiratory infection generally improves control of bronchospasm and constriction.
Pathophysiology and Complications
In asthma, obstruction of airflow occurs as the result of bronchial smooth muscle spasm, inflammation of bronchial mucosa, mucus hypersecretion, and sputum plugging. The most striking macroscopic finding in the asthmatic lung is occlusion of the bronchi and bronchioles by thick, tenacious mucous plugs (

FIGURE 7-7 Section of a lung with the bronchioles occluded by mucous plugs.
(Courtesy McLay RN, et al: Tulane gross pathology tutorial, Tulane University School of Medicine, New Orleans, Louisiana, 1997.)
Asthma is relatively benign in terms of morbidity. Most patients can expect a reasonably good prognosis, especially those in whom the disease develops during childhood. In many young children, the condition resolves spontaneously after puberty. In one reported series, however, two thirds of asthmatic children still had symptoms at age 21 years.
Clinical Presentation
Signs and Symptoms
Asthma is a disease of episodic attacks of airway hyperresponsiveness. For reasons that are unclear, attacks often occur at night but also may follow or accompany exposure to an allergen, exercise, respiratory infection, or emotional upset and excitement. Typical symptoms and signs of asthma consist of reversible episodes of breathlessness (dyspnea), wheezing, cough that is worse at night, chest tightness, and flushing. Onset usually is sudden, with peak symptoms occurring within 10 to 15 minutes. Inadequate treatment results in emergency department visits for about 25% of patients.
Laboratory Findings
Diagnostic testing by a physician is important in the differentiation of asthma from other airway diseases. Experienced clinical judgment and recognition of the signs and symptoms are essential, because laboratory tests for asthma are relatively nonspecific and no single test is diagnostic. Commonl/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses