Chapter 28
Anxiety, Eating Disorders, and Behavioral Reactions to Illness
Problems may be encountered in the dental practice that stem from a patient’s behavioral patterns, rather than from physical conditions. A good dentist-patient relationship can reduce the number of behavioral problems encountered in practice and can modify the intensity of emotional reactions. A positive dentist-patient relationship is based on mutual respect, trust, understanding, cooperation, and empathy. Role conflicts between the dentist and the patient should be avoided or should be identified and dealt with effectively. The anxious patient should be offered support that minimizes the damaging effects of anxiety, and the angry or uncooperative patient should be accepted and encouraged to share reasons for feelings and behavior, allowing emergence of a more peaceful and cooperative state of mind. Patients with emotional factors that contribute to oral or systemic diseases or symptoms and patients with more serious mental disorders can be managed in an understanding, safe, and empathetic manner.
The dentist may treat patients with a variety of behavioral and mental disorders. The fourth edition of Diagnostic and Statistical Manual of Mental Disorders, text revision (DSM-IV-TR),< ?xml:namespace prefix = "mbp" />
TABLE 28-1 System for Classification of Psychosocial Health
| Type | Description |
|---|---|
| Axis I | Clinical disorders |
| Other conditions that may be the focus of clinical attention | |
| Axis II | Personality disorders |
| Mental retardation | |
| Axis III | General medical conditions |
| Axis IV | Psychosocial and environmental problems |
| Axis V | Global assessment of functioning |
Data from American Psychiatric Association: Diagnostic and statistical manual of mental disorders, fourth ed, text rev, Washington, DC, American Psychiatric Association, 2000.

Box 28-1
Axis I
Clinical Disorders and Other Conditions That May Be a Focus of Clinical Attention
• Disorders usually first diagnosed in infancy, childhood, or adolescence
• Delirium, dementia, and amnestic and other cognitive disorders
• Mental disorders caused by a general medical condition
• Schizophrenia and other psychotic disorders
• Sexual and gender identity disorders
• Psychological factors that affect medical conditions
• Impulse control disorders not elsewhere classified
• Other conditions that may be a focus of clinical attention
From American Psychiatric Association: Diagnostic and statistical manual of mental disorders, fourth ed, text rev, Washington, DC, American Psychiatric Association, 2000.

The American Psychiatric Association plans to publish the new edition of the Diagnostic and Statistical Manual of Mental Disorders (i.e., DSM-5) in 2013.
This chapter discusses anxiety disorders (panic, phobias, posttraumatic stress disorder, and generalized anxiety disorder), eating disorders, and behavioral reactions to illness (

Box 28-2
Classification of Behavioral and Psychiatric Disorders
Psychological Factors That Affect Medical Conditions
Substance Abuse Disorders
Cognitive Disorders
Delusional (Paranoid) Disorder
• Erotomania, grandiosity, jealousy, persecution complex, somatic delusions
Data from American Psychiatric Association: Diagnostic and statistical manual of mental disorders, fourth ed, text rev, Washington, DC, American Psychiatric Association, 2000.

Anxiety Disorders
Definition
Anxiety is a natural response and a necessary warning adapatation in humans. Anxiety becomes a pathologic disorder when it is excessive and uncontrollable, requires no specific external stimulus, and results in physical and affective symptoms and changes in behavior and cognition.
Anxiety is a sense of psychological distress that may not have a focus. It is a state of apprehension that may involve an internal psychological conflict, an environmental stress, a physical disease state, or a medicine or drug effect, or combinations of these. Anxiety can be a purely psychological experience, with few somatic manifestations. Alternatively, it can be experienced as a purely physical phenomenon encompassing tachycardia, palpitations, chest pain, indigestion, headaches, and so forth, with no psychological distress other than concern about the physical symptoms. The reason for the variability in physical responses is not clear.
An understanding of anxiety requires definitions of some related entities, phobia and panic attack. A phobia is defined as an irrational fear that interferes with normal behavior. Phobias are fears of specific objects, situations, or experiences. The feared object, situation, or experience has taken on a symbolic meaning for the patient. Unconscious wishes and fears have been displaced from an original goal onto an external object.
A panic attack consists of a sudden, unexpected, overwhelming feeling of terror with symptoms of dyspnea, palpitations, dizziness, faintness, trembling, sweating, choking, flushes or chills, numbness or tingling sensations, and chest pains. The panic attack peaks in about 10 minutes and usually lasts for about 20 to 30 minutes.
Epidemiology: Incidence and Prevalence
Anxiety disorders constitute the most frequently found psychiatric problem in the general population. Simple phobia is the most common of the anxiety disorders (up to 25% of the population will experience a phobia); however, panic disorder is the most common anxiety disorder in people who seek medical treatment (lifetime prevalence of 3.5%).
Etiology
Anxiety represents a threatened emergence into consciousness of painful, unacceptable thoughts, impulses, or desires (anxiety may result from psychological conflicts of the past and present). These psychological conflicts or feelings stimulate physiologic changes that lead to clinical manifestations of anxiety.
The cause of panic disorder is unknown but appears to involve a genetic predisposition, altered autonomic responsivity, and social learning. Panic disorder shows a familial aggregation; the disorder is concordant in 30% to 45% of monozygotic twins, and genome-wide screens have identified suggestive risk loci on 1q, 7p15, 10q, 11p, and 13q. Acute panic attacks appear to be associated with increased noradrenergic discharges in the locus coeruleus.
No single theory fully explains all anxiety disorders. No single biologic or psychological cause of anxiety has been identified. Psychosocial and biologic processes together may best explain anxiety. The locus coeruleus, a brain stem structure that contains most of the noradrenergic neurons in the central nervous system (CNS), appears to be involved in panic attacks and anxiety. Panic and anxiety may be correlated with dysregulated firing of the locus coeruleus caused by input from multiple sources, including peripheral autonomic afferents, medullary afferents, and serotonergic fibers.
Anxiety states also may be associated with organic diseases, other psychiatric disorders, use of certain drugs, hyperthyroidism, and mitral valve prolapse. Anxiety also is associated with mood disorders, schizophrenia, or personality disorders.
Clinical Presentation and Medical Management
From a psychological perspective, anxiety can be defined as emotional pain or a feeling that all is not well—a feeling of impending disaster. The source of the problem usually is not apparent to persons with anxiety. The feeling is the same in anxious patients as that in patients with fear, but the latter are aware of what the problem is and why they are “fearful.”
Physiologic reactions to anxiety and to fear are the same and are mediated through the autonomic nervous system. Sympathetic and parasympathetic components may be involved. Signs and symptoms of anxiety caused by overactivation of the sympathetic nervous system include increased heart rate, sweating, dilated pupils, and muscle tension. Signs and symptoms of anxiety resulting from stimulation of the parasympathetic system include urinary frequency and episodic diarrhea.
Most people periodically experience some degree of anxiety in one or more aspects of their lives. Anxiety can be a strong motivator; low levels of anxiety can increase attention and improve performance. Anxiety leads to dysfunction when it is constant, or it may result in episodes of extreme vigilance, excessive motor tension, autonomic hyperactivity, and impaired concentration. Anxiety is part of the clinical picture in many patients with psychiatric disorders. Patients with mood disorders, dementia, psychosis, panic disorder, adjustment disorders, and toxic and withdrawal states often report feelings of anxiety.
Phobias
Phobias consist of three major groups: agoraphobia, social, and simple. Agoraphobia is a fear of having distressful or embarrassing symptoms on leaving home. It often accompanies panic disorder. Social phobias may be specific, such as fear of public speaking, or general, such as fear of being embarrassed when with people. Simple phobias include fear of snakes, heights (
Panic Attack
About 15% of patients who are seen by cardiologists come to the doctor because of symptoms associated with a panic attack. Onset usually is between late adolescence and the mid-30s, but it may occur at any age. A key feature of panic is the adrenergic surge, which results in the fight-or-flight response. This response is an exaggerated sympathetic response (
TABLE 28-2 Anxiety, Panic Attack, Generalized Anxiety Disorder, and Posttraumatic Stress Disorder
Data from Schiffer RB: Psychiatric disorders in medical practice. In Goldman L, Ausiello D, editors: Cecil textbook of medicine, ed 23, Philadelphia, Saunders, 2008; and Lucey JV, Corvin A: Anxiety disorders. In Wright P, Stern J, Phelan M, editors: Core psychiatry, ed 2, Edinburgh, Elsevier, 2005.
Generalized Anxiety Disorder
Some patients present with a persistent, diffuse form of anxiety characterized by signs and symptoms of motor tension, autonomic hyperactivity, and apprehension (see
Posttraumatic Stress Disorder
Posttraumatic stress disorder (PTSD) is a syndrome of psychophysiologic signs and symptoms that develop after exposure to a traumatic event outside the usual range of human experience, such as combat exposure, a holocaust experience, rape, or a civilian disaster such as a hurricane (

FIGURE 28-2 Time lapse photo of Hurricane Andrew, which hit southern Florida in August 1992. During past years, a number of major hurricanes hit the United States. Hurricane Katrina, which hit the Gulf Coast states in August 2005, was the most destructive in recent history in terms of number of deaths and extent of property damage.

FIGURE 28-3 The 1980 eruption of Mount St. Helens resulted in an increased incidence of posttraumatic stress disorder among residents of the Pacific Northwest.
Most men with PTSD have been in combat (
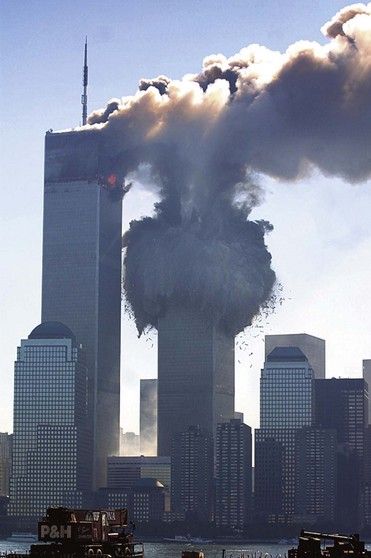
FIGURE 28-5 Attack on the Twin Towers of the World Trade Center in New York City on September 11, 2001.
(Courtesy Getty Images.)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses




