Chapter 30
Drug and Alcohol Abuse
The abusive use of drugs and alcohol is a huge and growing public health problem in the United States, as well as in many other countries worldwide. Drug and alcohol abuse has far-reaching effects on persons engaging in such activity, as well as their families and communities, with a consequent heavy impact on law enforcement, the judicial system, politics, and health care. It is inevitable that dental practitioners will encounter abusers of drugs and/or alcohol among their patients, and unfortunately, some practitioners will themselves turn to such abuse. This chapter discusses the effects of drug and alcohol abuse as they pertain to dental management. Another legal drug of abuse, nicotine, is discussed in < ?xml:namespace prefix = "mbp" />
Definitions
According to the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV), of the American Psychiatric Association,
Alcoholism is a term commonly used to describe a condition of substance abuse focused on consumption of alcohol. A more precise definition, however, has been proposed by O’Conner: “a primary chronic disease with genetic, psychosocial, and environmental factors … often progressive and fatal … characterized by impaired control over drinking, preoccupation with the drug alcohol, use of alcohol despite future consequences, and distortions of thinking, most notably denial.”
Epidemiology
Incidence and Prevalence
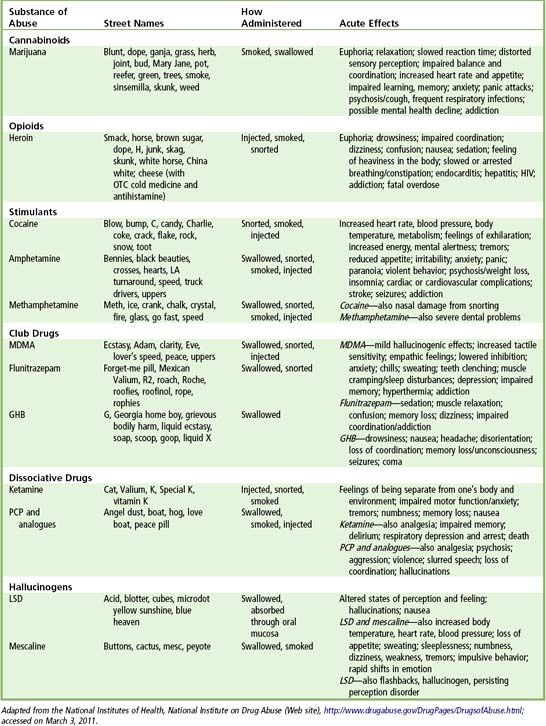
Illicit drugs of abuse include marijuana and hashish, heroin, cocaine (including crack), methamphetamine and its analogues, so-called club drugs, hallucinogens, and dissociative drugs (
Marijuana is the most commonly used illicit drug. In 2009, there were 16.7 million past-month users. Among persons aged 12 or older, the rate of past-month marijuana use and the number of users in 2009 (6.6%, or 16.7 million) were higher than in 2008 (6.1%, or 15.2 million) and in 2007 (5.8%, or 14.4 million). In 2009, there were 1.6 million current cocaine users aged 12 or older, comprising 0.7% of the population. These estimates were similar to the number and rate in 2008 (1.9 million, or 0.7%) but were lower than the estimates in 2006 (2.4 million, or 1.0%). An estimated 3.7 million people have reported previous use of heroin, with an estimated 150,000 persons becoming new users every year.
The use of prescription opioids (e.g., OxyContin) for nonmedical reasons is currently one of the fastest-growing dimensions of drug abuse in the United States, with a 225% increase from 1992 to 2000.
According to the 2009 NSDUH,
The prevalence of problem drinking in general outpatient and inpatient medical settings has been estimated to be between 15% and 40%.
Etiology
The neurobiology of addiction and dependence is complex and involves a unique set of variables. Disruption of the endogenous reward systems in the brain is a common feature of all of the major drugs of abuse; most of these drugs act by disrupting dopamine circuits in the brain.
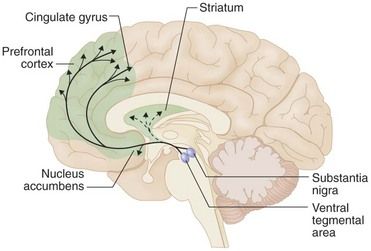
FIGURE 30-1 Brain reward circuits.
The major dopaminergic projections to the forebrain that underlie brain reward are shown superimposed on a diagram of the human brain: projection from the ventral tegmental area to the nucleus accumbens, and prefrontal cerebral cortex. Also shown are projections from the substantia nigra to the dorsal striatum, which play a role in habit formation and in well-rehearsed motor behavior, such as drug seeking and drug administration.
(From Hyman SE: Biology of addiction. In Goldman L, Ausiello D, editors: Cecil medicine, ed 23, Philadelphia, 2008, Saunders.)
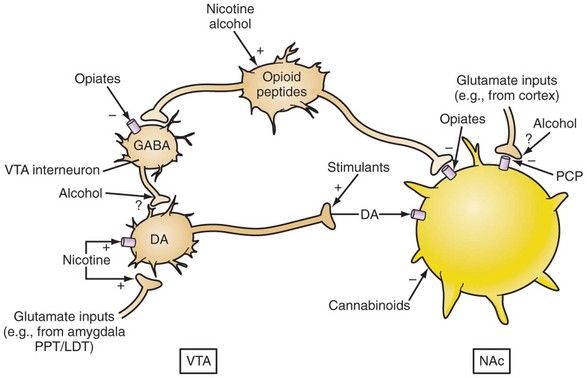
FIGURE 30-2 Converging acute actions of drugs of abuse on the ventral tegmental area and nucleus accumbens. DA, Dopamine; GABA, γ-aminobutyric acid; LDT, Laterodorsal tegmentum; NAc, Nucleus accumbens; PCP, Phencyclidine; PPT, Pedunculopontine tegmentum; VTA, Ventral tegmental area.
(From Renner JA, Ward EN: Drug addiction. In Stern TA, et al, editors: Massachusetts General Hospital comprehensive clinical psychiatry, Philadelphia, 2008, Mosby.)
Clinical Presentation and Medical Management
Substance dependence occurs when the person using the substance takes it in larger amounts or over a longer period than was originally intended. A great deal of time may be spent in activities needed to procure the substance, take it, or recover from its effects. The person gives up important social, occupational, and recreational activities because of substance use. Marked tolerance to the substance may develop; therefore, progressively larger amounts are needed to achieve intoxication or to produce the desired effect. The person with the disorder continues to take the substance, despite persistent or recurrent social, psychological, and physical problems that result from its use.
Substance abuse denotes substance use that does not meet the criteria for dependence (
TABLE 30-2 Diagnostic Criteria for Dependence and Drug Abuse
From Samet JH: Drug abuse and dependence. In Goldman L, Ausiello D, editors: Cecil textbook of medicine, ed 23, Philadelphia, 2008, Saunders.
Withdrawal occurs when the person with substance dependence stops or reduces intake of the substance. Withdrawal symptoms vary in accordance with the substance involved. Physiologic signs of withdrawal are common after prolonged use of alcohol, opioids, sedatives, hypnotics, and anxiolytics. Such signs are less obvious in withdrawal from cocaine, nicotine, amphetamines, and cannabis.
Marijuana
Marijuana is the common name for cannabis, which is the most commonly used illicit drug in the world.
Opioids
The primary effects of the opioids (opiate-like drugs) are to decrease pain perception, cause modest levels of sedation, and produce euphoria. Drugs in this category include those derived from naturally occurring alkaloids morphine and codeine. Semisynthetic drugs produced from morphine or thebaine molecules include hydrocodone, hydromorphone, heroin, and oxycodone. Synthetic opioids include meperidine, propoxyphene, diphenoxylate, fentanyl, buprenorphine, methadone, and pentazocine. Tolerance to any single opioid is likely to generalize to other drugs in the group.
Through direct effects on the central nervous system (CNS), opiates may produce nausea and vomiting, decreased pain perception, euphoria, and sedation. Additives in street drugs can cause permanent damage to the nervous system, including peripheral neuropathy and CNS dysfunction. Users of such drugs may experience constipation and anorexia. Respiratory depression occurs as the result of a decreased response of the brain stem to carbon dioxide tension. This effect is part of the toxic reaction to opiates,as described later on, but it also can be significant in patients with compromised lung function.
Complications are common among abusers of narcotics, especially when administered intravenously. Cardiovascular effects of the opiates are mild, and no direct effect on heart rhythm or myocardial contractility has been noted with their use. Orthostatic hypotension, probably caused by dilation of peripheral vessels, may occur. The major complication with intravenous use of these drugs involves the use of contaminated or shared needles; pathogens introduced in this manner can cause hepatitis B and C and bacterial endocarditis, and an association with increased risk for infection with human immunodeficiency virus (HIV) also has been noted.
Dependence on opiates can be seen in at least three groups of patients. The first group is the minority of patients with chronic pain syndromes who misuse their prescribed drugs. The second group at high risk consists of physicians, dentists, nurses, and pharmacists. These persons have easy access to drugs with abuse potential.
Toxic reactions (overdose) are seen with all opiates. These reactions are more frequent and dangerous with more potent drugs such as fentanyl, which is 80 to 100 times more powerful than morphine. Intravenous overdose can lead immediately to slow, shallow respirations, bradycardia, a drop in body temperature, and lack of responsiveness to external stimulation. Emergency treatment includes support of vital signs with the use of a respirator and administration of a reversal agent such as naloxone by intramuscular or intravenous injection.
In contrast with sedative withdrawal, withdrawal from opiates is an unpleasant but not life-threatening experience. Gastrointestinal upset, muscle cramps, rhinorrhea, and irritability are the prominent signs and symptoms. Opiate users with memory impairment or cognitive dysfunction should be assessed for HIV infection by evaluation of risk />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses