CHAPTER 7
Island Osteoperiosteal Flap
Everything has been thought of before, but the problem is to think of it again.
—Johann Wolfgang von Goethe
An island osteoperiosteal flap (i-flap) is a modified alveolar split osteotomy in which the greenstick fracture is completed and the facial plate, while remaining attached to mucoperiosteum, is detached from the basal bone.1 This enables freedom of movement of the facial plate in all directions and allows advancement of the facial plate crestally (or anteriorly/posteriorly) even as width is being gained. This type of bone flap has utility in situations where the alveolar crest is slanted inferiorly on the facial side from an ideal crestal morphology. This situation is common and is caused by facial plate resorption that becomes evident at root dehiscence sites left to heal without socket bone grafting after dental extraction.2,3
The utility of the i-flap is that the facial plate can be freed to widen the alveolus and then advanced crestally to lengthen the osseous facial alveolar dimension. Width and height are gained simultaneously in a very simple procedure.
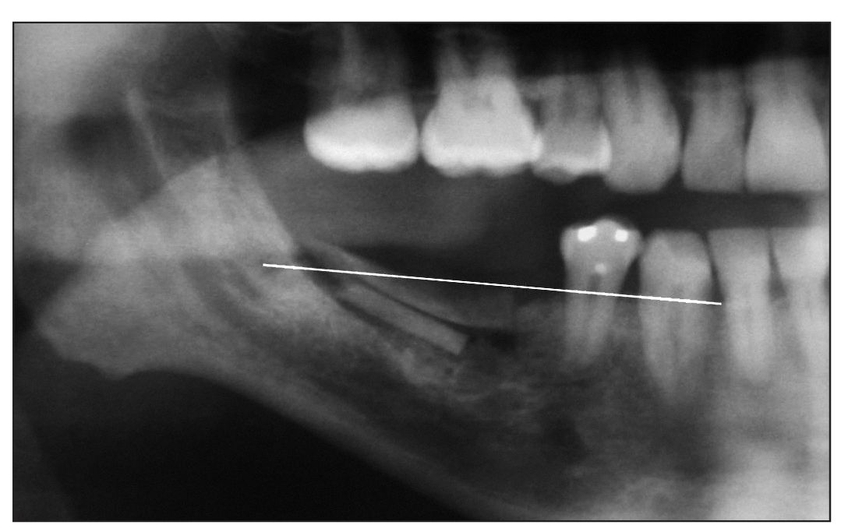
Fig 7-1 A cephalogram or panoramic radiograph generally suggests a level alveolar plane (white line), deviations from which indicate alveolar deficiency or alveolar hyperplasia. Shown here is a deficient alveolar plane corrected by a sandwich osteotomy procedure.
Use of the i-flap should probably be restricted to alveolar edentulous sites that are large enough to allow mobilization of a substantial ossicle (not too thin or too small). A 2-mm-thick plate of bone is recommended as a minimum.4 Also, the i-flap should be a full-length alveolar plate, perhaps 8 to 10 mm in height, to prevent small pieces of bone from becoming detached and devitalized. When possible, the i-flap should include bone marrow, and not just cortical bone, to provide a setting that is more conducive to rapid endosseous vascularization and incorporation of the interpositional bone graft.5,6
The i-flap is best used in healed extraction sites. When it is used to mobilize a thin facial plate in an immediate extraction site, even without reflection of a mucoperiosteal flap, the buccal plate resorbs at least in part due to functional disruption of bundle bone. When it is thin, the crestal bone at the facial margin in the extraction setting is often exclusively bundle bone and therefore resorbs following loss of the functional matrix of the periodontium. 7
The intraoral i-flap has not been well studied or critically evaluated but has been used inadvertently over the years without apparent late-term bone resorption. The intraoral i-flap has only recently been mobilized to distances of 5 mm or more from its original osseous position (Jensen et al, unpublished data, 2009).
 Case Selection
Case Selection
An ideal case for the i-flap is an alveolus with a moderately deficient width and an alveolar crest that slants a few millimeters toward the vestibule on the facial side. When the palatal plate is still in good crestal position, that is, at the alveolar plane, and 4 to 6 mm of width is available, an i-flap can be performed easily. The procedure is useful in the esthetic zone, where marginal gingival height is paramount for implant restorations. In contrast to the internal alveolar split graft that is indicated where the height of both the palatal and facial plates is deficient, the i-flap is used only for alteration of the facial plate, restoring the facial alveolar dimension so that it is level with the alveolar plane.
The alveolar plane may be thought of as a strictly radiographic finding that indicates the level of the alveolar crest across the arch as viewed on a panoramic radiograph or lateral cephalogram (Fig 7-1). Deviation from the radiographic alveolar plane is a gross indicator of the presence of a vertical alveolar defect. However, the alveolar plane can also be thought of as an anatomically based plane with two components, the plane of the palatal alveolar crestal bone level and the plane of the facial alveolar crestal bone level (Figs 7-2a to 7-2c). The i-flap is indicated when there is significant disparity between these two planes (Figs 7-2d and 7-2e). This is well demonstrated in a stereolithographic model (Fig 7-3).
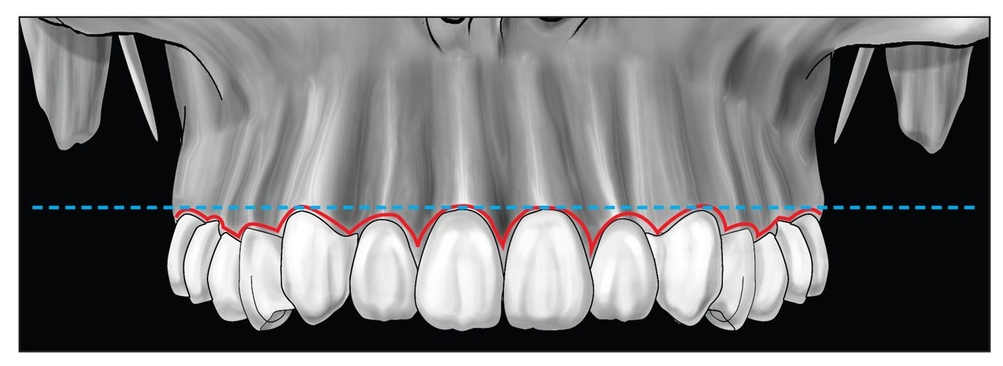
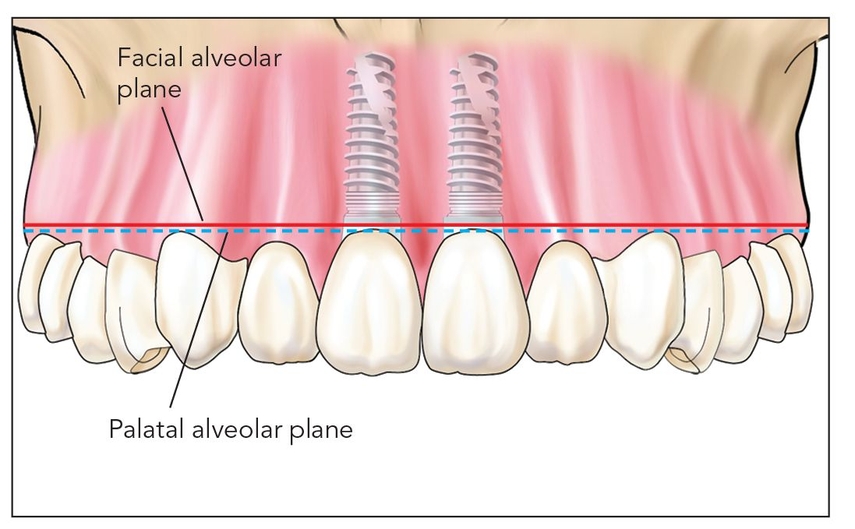
Fig 7-2a The radiographic alveolar plane (blue dashed line) shown above is not equivalent to the anatomic alveolar plane.
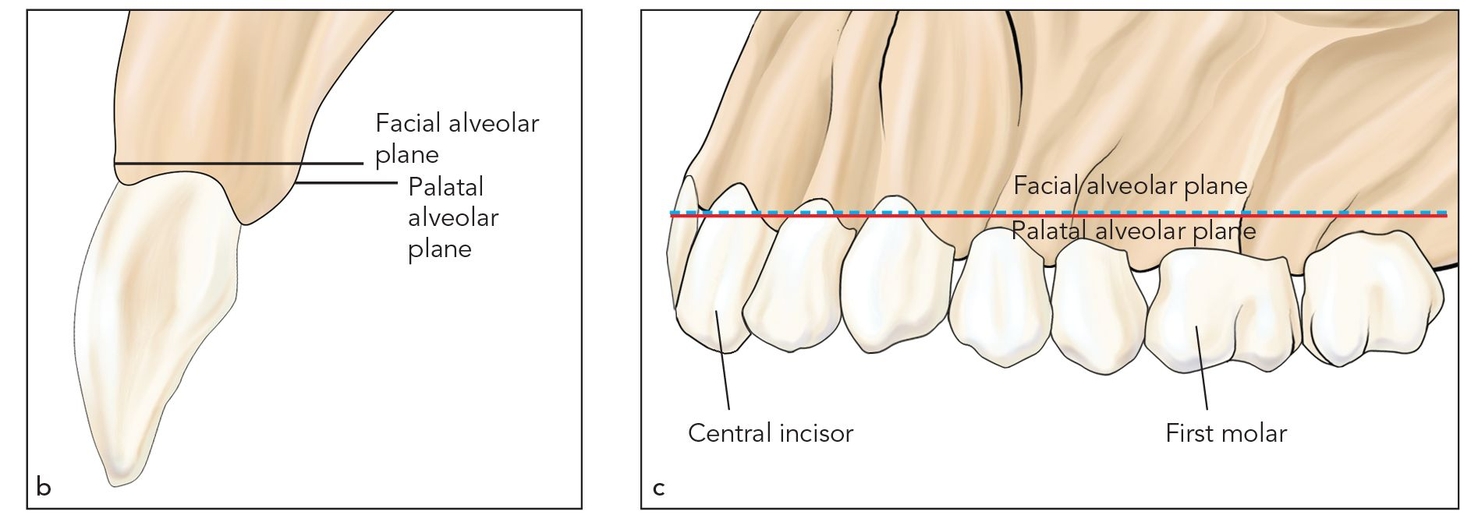
Figs 7-2b and 7-2c The anatomic alveolar plane has two components, the palatal alveolar crestal bone level (red line) and the facial alveolar crestal bone level (blue dashed line).
Figs 7-2d and 7-2e When there is a disparity between the palatal (red line) and facial (blue dashed line) alveolar planes, the i-flap is indicated to move the deficient facial plate to a correct alveolar plane position.
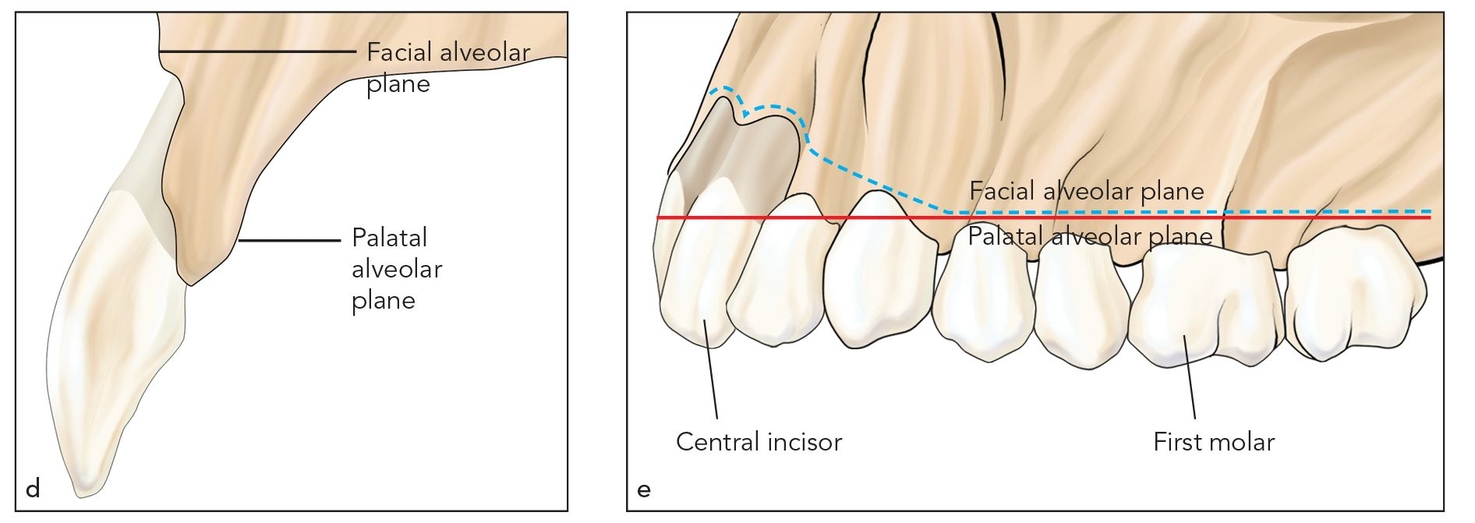
Figs 7-3a and 7-3b A stereolithographic model reveals the disparity in the facial and palatal alveolar planes.
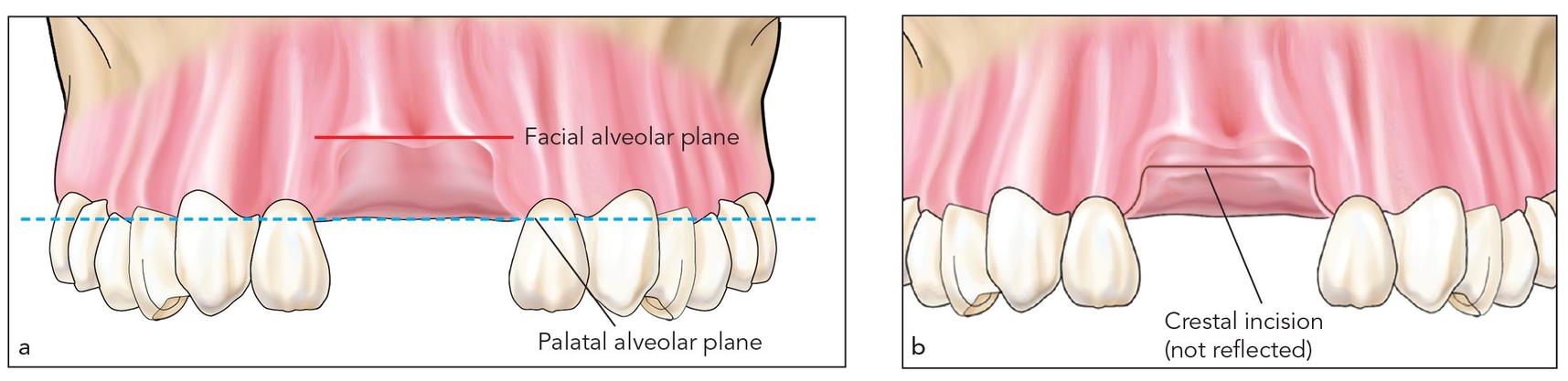
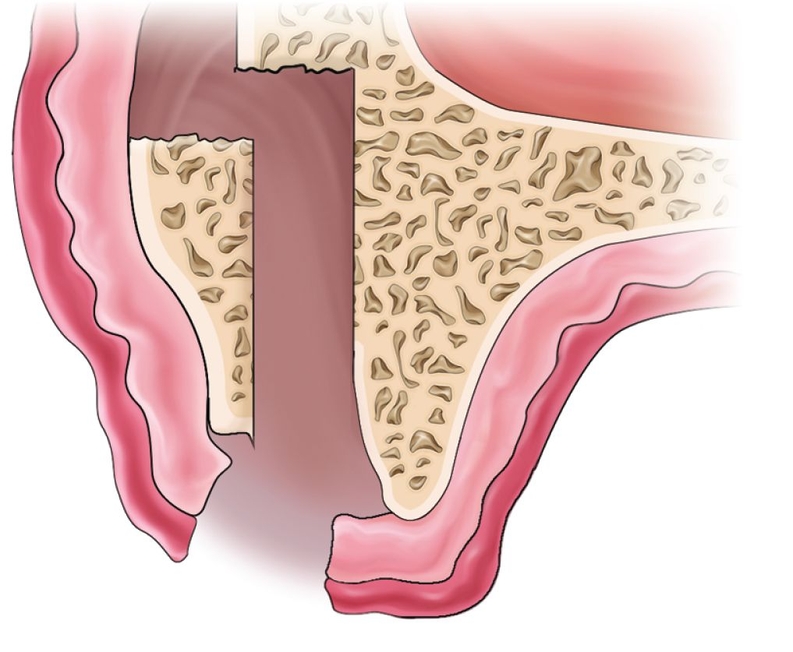
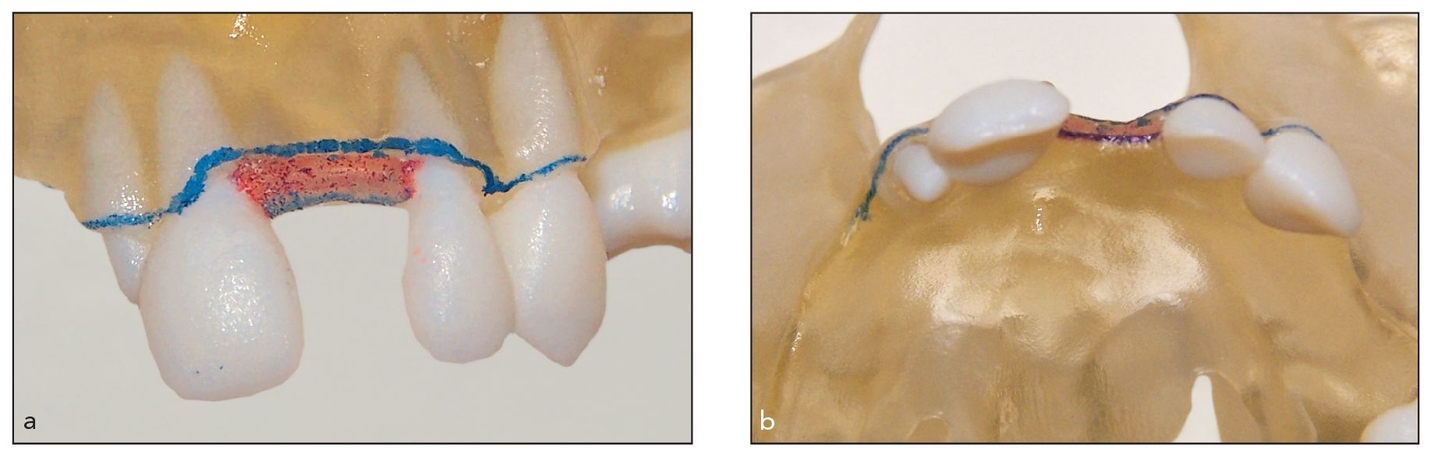
Figs 7-4a and 7-4b An edentulous site with facial plate dehiscence is approached through a minimally reflected crestal incision located in fixed connective tissue between the two planes at the crest.
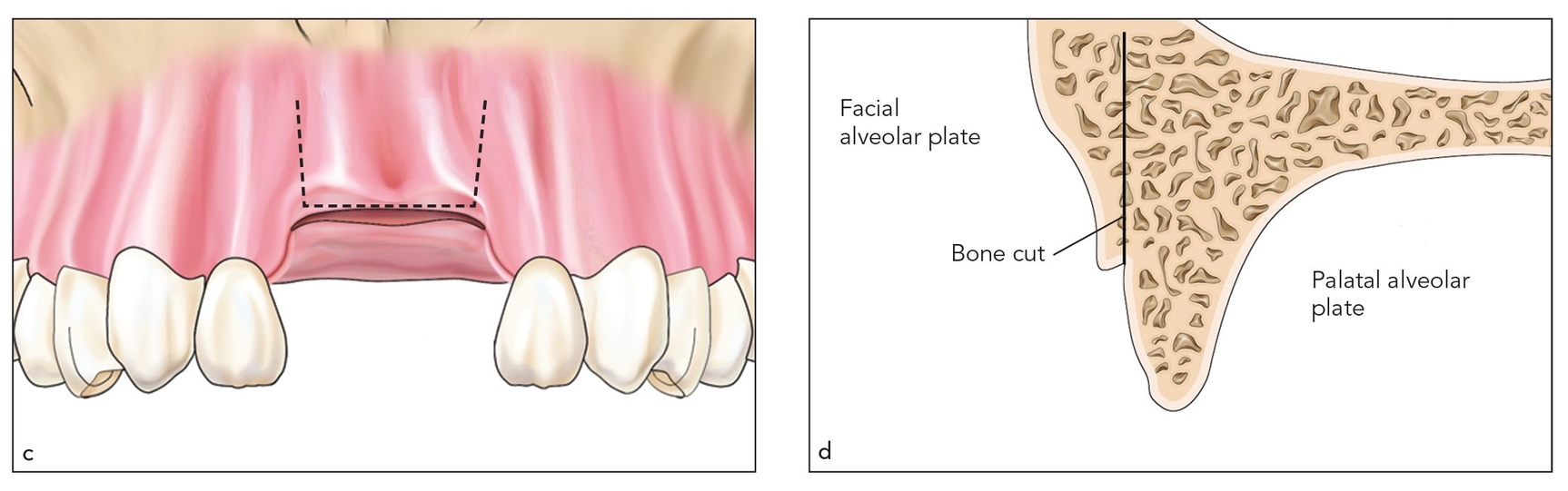
Figs 7-4c and 7-4d Piezoelectric surgery or osteotomes are used to split the ridge coronally after vertical cuts (dashed lines) are made about 2 mm from adjacent teeth. The alveolar split extends approximately 10 mm toward the vestibule, where the outfracture occurs.
 Surgical Technique
Surgical Technique
A palatal crestal incision is made in the edentulous space with minimal extension around the teeth adjacent to the defect. A minimal full-thickness flap is reflected to expose the alveolar crest only (Figs 7-4a and 7-4b). A piezoelectric knife or osteotomes are used to split the ridge coronally after vertical cuts are made about 2 mm from the adjacent root surfaces and extended in the vestibular direction about 10 mm (Figs 7-4c and 7-4d). A minimum of 2 mm of facial bone plate width should remain after the split is completed.
The osteotome is inserted and malleted to basal bone (about 10 mm). The osteotome is left in place and then torqued facially to open about a 4-mm gap (Figs 7-4e and 7-4f). The straight osteotome is then removed and replaced with a curved osteotome with the curve facing facially. The curved osteotome is then gently malleted or deflected by hand pressure palatally, that is, in the opposite direction; during this process, a finger is placed over the facial plate to prevent dislodging. This palatal movement usually completes the fracture separation of the facial plate from the basal bone without detachment from periosteum.
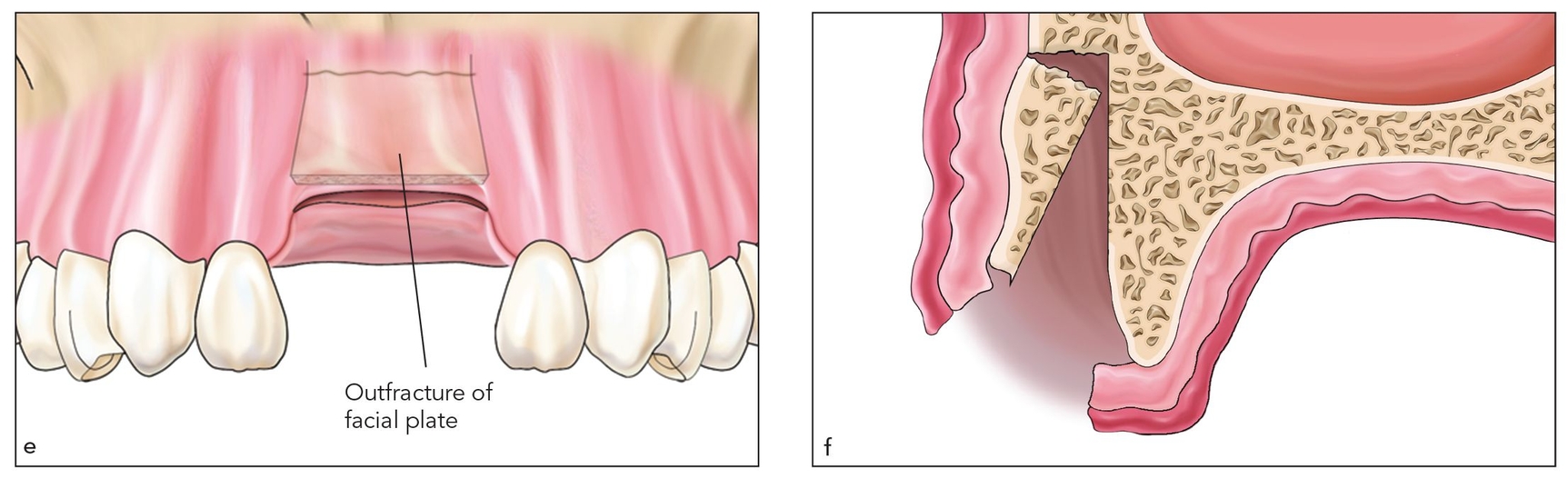
Figs 7-4e and 7-4f The alveolar split is spread open with an osteotome torqued facially. At least a 2-mm-thick facial bone plate should be obtained.
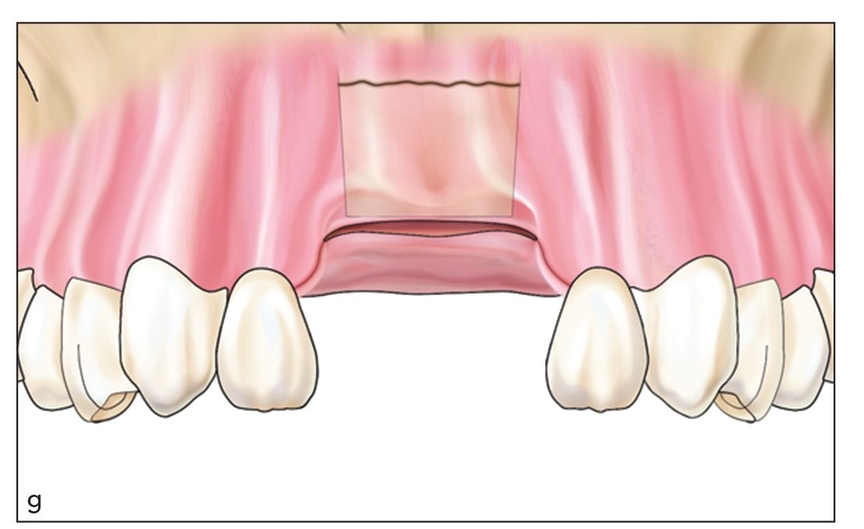
Fig 7-4g The i-flap is created by using a curved osteotome to free the facial plate at the site of greenstick fracture. Then, the osteotome is deflected palatally, that is, in the opposite direction, to move the i-flap crestally.
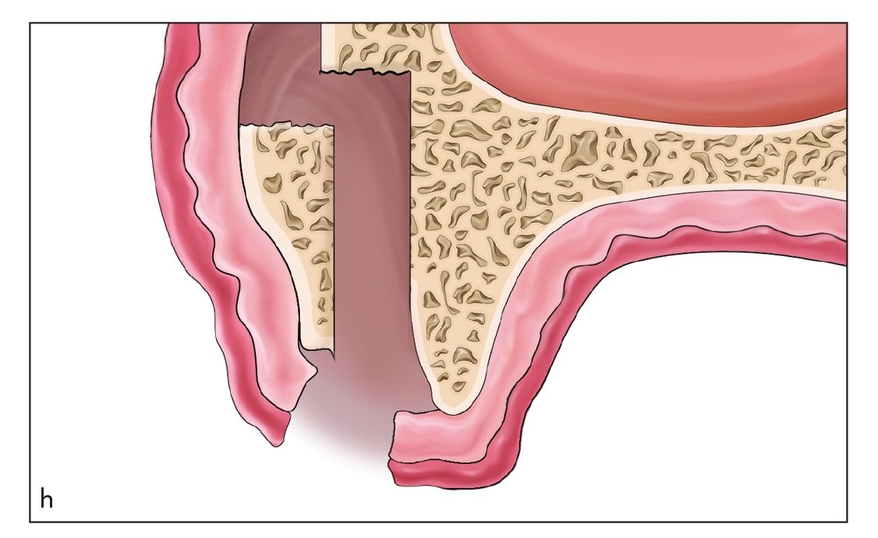
Fig 7-4h Palatal deflection with the osteotome frees the facial plate, creating an i-flap.
The free-floating osteoperiosteal i-flap is easily advanced crestally using blunt instrumentation (Figs 7-4g and 7-4h). The segment of bone is then manipulated and advanced into position away from the fracture site by relieving wound tension (Fig 7-4i). An interpositional bone graft is placed (Fig 7-4j). Transgingival fixation with a bone screw is seldom necessary because suturing usually stabilizes the bone within the flap as the wound is closed (Fig 7-4k).
Implants are placed 4 months after the flap procedure (Fig 7-4l), and then the final restoration is completed (Figs 7-4m and 7-4n).
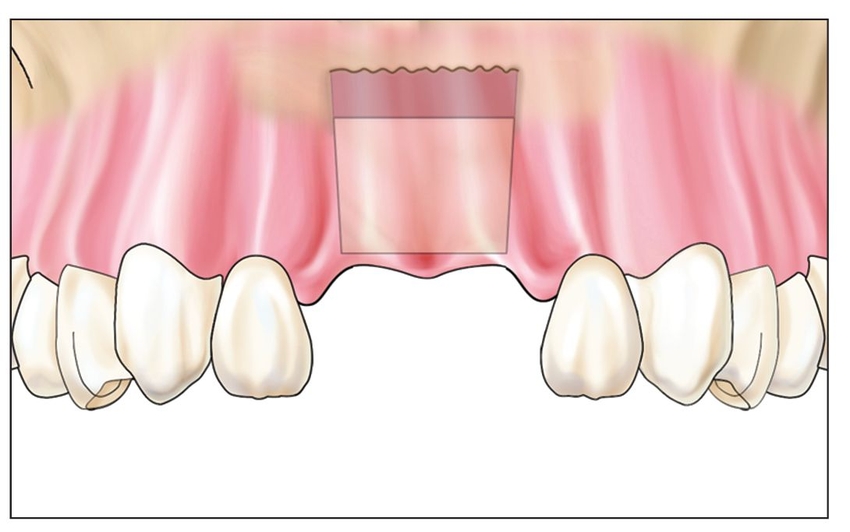
Fig 7-4i The free-floating bone flap is mobilized and placed in the desired position to make the facial plane even with the palatal plane.
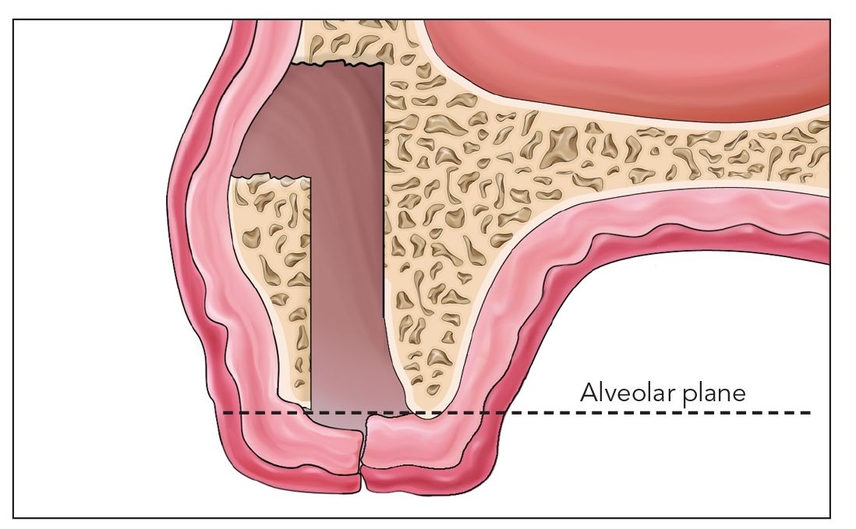
Fig 7-4j Following interpositional bone grafting, the i-flap will be sutured in position to heal at the alveolar plane (dashed line).
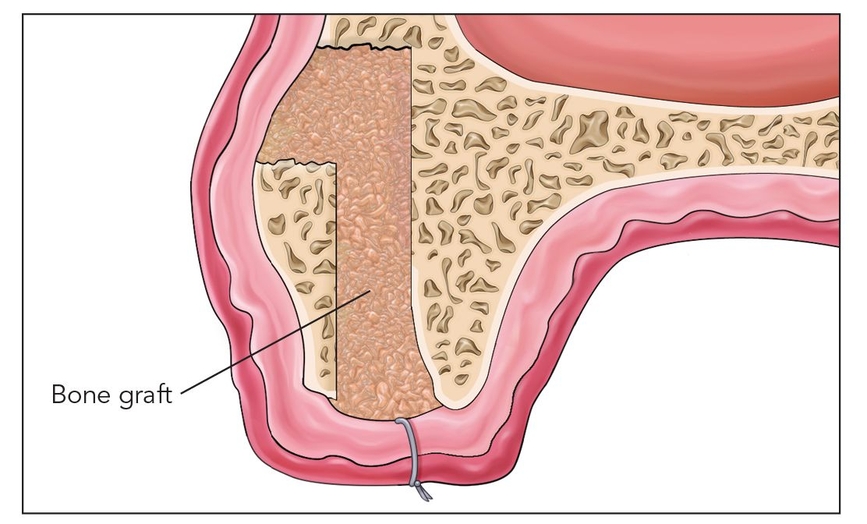
Fig 7-4k The interpositional graft is done in such a way that alveolar widening and crestal movement of the facial plate are obtained without rigid fixation.
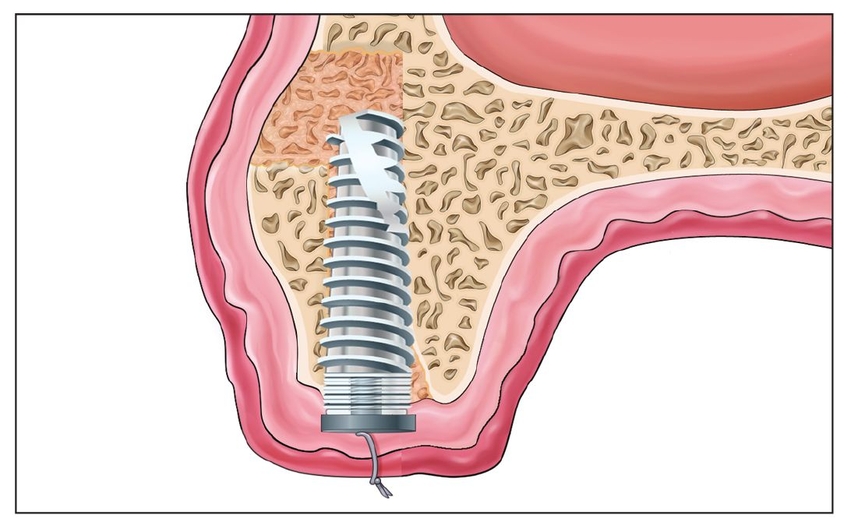
Fig 7-4l The implant is placed 4 months after surgery, after the bone graft has consolidated.
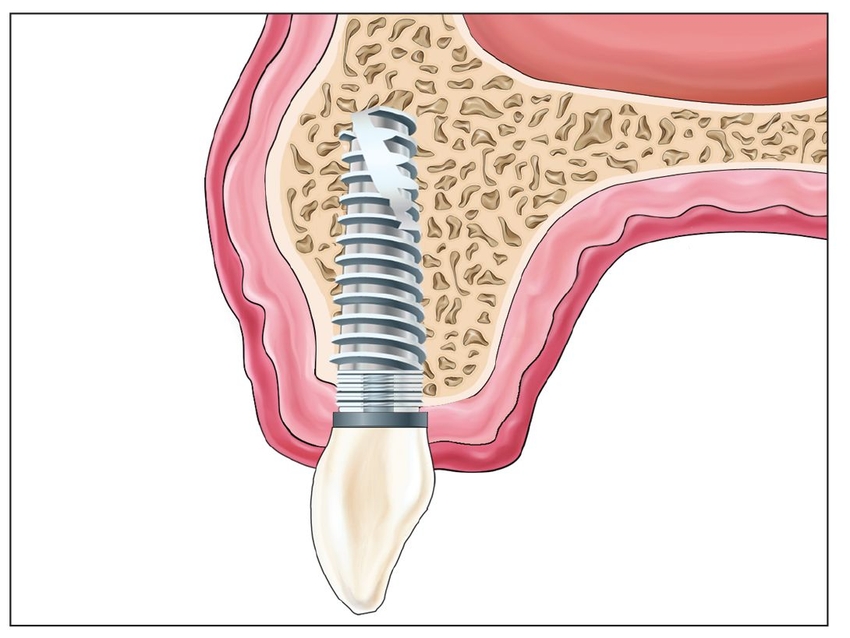
Fig 7-4m The final restoration, in lateral view, shows that the alveolar width is adequate and the implant body is located well within the buccal plane.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses