Supportive Periodontal Treatment
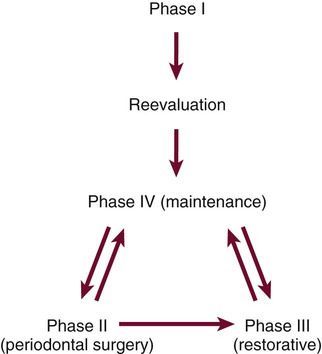
Preservation of the periodontal health of the treated patient requires as positive a program as that required for the elimination of periodontal disease. After Phase I therapy is completed, patients are placed on a schedule of periodic recall visits for maintenance care to prevent recurrence of the disease (Figures 69-1 and 69-2).
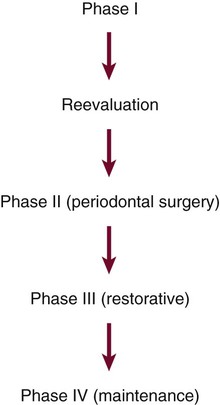
Maintenance phase should be started immediately after the reevaluation of Phase I therapy.
Transfer of the patient from active treatment status to a maintenance program is a definitive step in total patient care that requires time and effort on the part of the dentist and staff. Patients must understand the purpose of the maintenance program, and the dentist must emphasize that preservation of the teeth depends on maintenance therapy. Patients who are not maintained in a supervised recall program subsequent to active treatment show obvious signs of recurrent periodontitis (e.g., increased pocket depth, bone loss, or tooth loss).7,10,16,17,21,41 The more often patients present for recommended supportive periodontal treatment (SPT), the less likely they are to lose teeth.21,39,41,44,61,69 One study found that treated patients who do not return for regular recall are at 5.6 times greater risk for tooth loss than compliant patients.17 Another study showed that patients with inadequate SPT after successful regenerative therapy have a 50-fold increase in risk of probing attachment loss compared with those who have regular recall visits.20
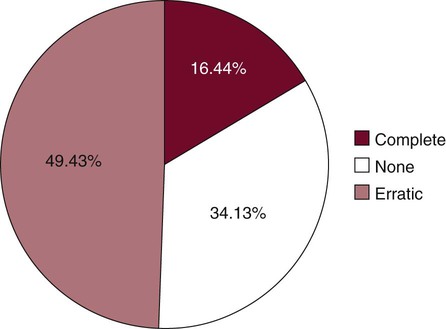
Motivational techniques and reinforcement of the importance of the maintenance phase of treatment should be considered before performing definitive periodontal surgery.10 Studies show that few patients display complete compliance with recommended maintenance schedules1,43,38,39,42,43,67,69 (Figure 69-3). It is meaningless simply to inform patients that they are to return for periodic recall visits without clearly explaining the significance of these visits and describing what is expected of patients between visits.
The maintenance phase of periodontal treatment starts immediately after the completion of Phase I therapy (see Figures 69-1 and 69-2). While the patient is in the maintenance phase, the necessary surgical and restorative procedures are performed. This ensures that all areas of the mouth retain the degree of health attained after Phase I therapy.
Rationale for Supportive Periodontal Treatment
Studies show that even with appropriate periodontal therapy, some progression of disease is possible.29,32,45,53,60,66 One likely explanation for the recurrence of periodontal disease is incomplete subgingival plaque removal.64,66 If subgingival plaque is left behind during scaling, it regrows within the pocket. The regrowth of subgingival plaque is a slow process compared with that of supragingival plaque. During this period (perhaps months), the subgingival plaque may not induce inflammatory reactions that can be discerned at the gingival margin. The clinical diagnosis may be further confused by the introduction of adequate supragingival plaque control because the inflammatory reactions caused by the plaque in the soft-tissue wall of the pocket are not likely to be manifested clinically as gingivitis. Thus inadequate subgingival plaque control can lead to continued loss of attachment, even without the presence of clinical gingival inflammation.
Bacteria are present in the gingival tissues in chronic and aggressive periodontitis cases.14,18,24,48 Eradication of intragingival microorganisms may be necessary for a stable periodontal result.24 Scaling, root planing, and even flap surgery may not eliminate intragingival bacteria in some areas.14 These bacteria may recolonize the pocket and cause recurrent disease.
Bacteria associated with periodontitis can be transmitted between spouses and other family members.2,62 Patients who appear to be successfully treated can become infected or reinfected with potential pathogens. This is especially likely in patients with remaining pockets.
Another possible explanation for the recurrence of periodontal disease is the microscopic nature of the dentogingival unit healing after periodontal treatment. Histologic studies have shown that after periodontal procedures, tissues usually do not heal by formation of new connective tissue attachment to root surfaces,15,56,57 but result in a long junctional epithelium. It has been speculated that this type of dentogingival unit may be weaker and that inflammation may rapidly separate the long junctional epithelium from the tooth. Thus treated periodontal patients may be predisposed to recurrent pocket formation if maintenance care is not optimal.
Subgingival scaling alters the microflora of periodontal pockets.40,47,54 In one study, a single session of scaling and root planing in patients with chronic periodontitis resulted in significant changes in subgingival microflora.40 Reported alterations included a decrease in the proportion of motile rods for 1 week, a marked elevation in the proportion of coccoid cells for 21 days, and a marked reduction in the proportion of spirochetes for 7 weeks.
Although pocket debridement suppresses components of the subgingival microflora associated with periodontitis, periodontal pathogens may return to baseline levels within days or months.4,53 The return of pathogens to pretreatment levels generally occurs in approximately 9 to 11 weeks but can vary dramatically among patients.4
Both the mechanical debridement performed by the therapist and the motivational environment provided by the appointment seem to be necessary for good maintenance results. Patients tend to reduce their oral hygiene efforts between appointments.5,69 Knowing that their hygiene will be evaluated motivates them to perform better oral hygiene in anticipation of the appointment.
In one study the proportion of spirochetes obtained in baseline samples of subgingival flora was highly correlated with clinical periodontal deterioration over 1 year.35 However, subsequent reports in the same longitudinal study concluded that the arbitrary assignment of treated periodontitis patients to 3-month maintenance intervals appears to be as effective in preventing recurrences of periodontitis as assignment of recall intervals based on microscopic monitoring of the subgingival flora.34,35 Microscopic monitoring was found not to be a reliable predictor of future periodontal destruction in patients on 3-month recall programs, presumably because of the alteration of subgingival flora produced by subgingival instrumentation.
Maintenance Program
Periodontal care at each recall visit comprises three parts (Box 69-1). The first part involves examination and evaluation of the patient’s current oral health. The second part includes the necessary maintenance treatment and oral hygiene reinforcement. The third part involves scheduling the patient for the next recall appointment, additional periodontal treatment, or restorative dental procedures. The time required for a recall visit for patients with multiple teeth in both arches is approximately 1 hour,49 which includes time for greeting the patient, setting up, and cleaning up.
Examination and Evaluation
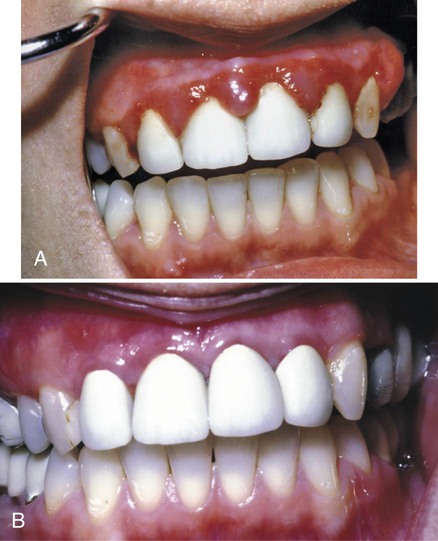
The recall examination is similar to the initial evaluation of the patient (see Chapter 29). However, because the patient is not new to the office, the dentist primarily looks for changes that have occurred since the last evaluation. Analysis of the current oral hygiene status of the patient is essential. Updating of changes in the medical history and evaluation of restorations, caries, prostheses, occlusion, tooth mobility, gingival status, and periodontal and periimplant probing depths are important parts of the recall appointment. The oral mucosa should be carefully inspected for pathologic conditions (Figures 69-4 to 69-9).

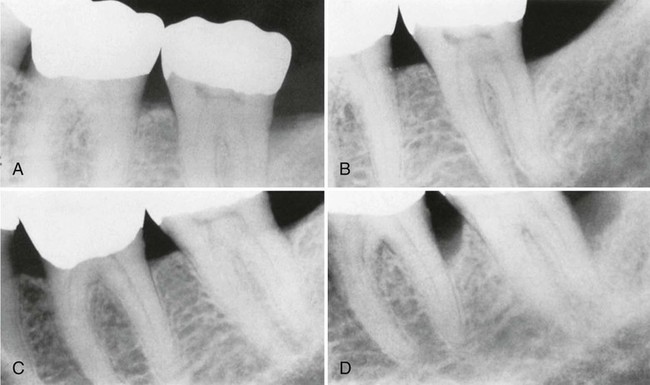
A, Original radiograph of a 58-year-old male. Note the deep distal bone loss on tooth #18 and the moderate distal lesion of tooth #19. Surgical treatment included osseous grafting. B, Radiograph 14 months after surgical therapy. The patient had recall maintenance performed every 3 to 4 months. C, Appearance 3 years after surgery, with regular recalls every 3 to 4 months. D, Appearance after 2 years without recalls (7 years after surgery). Note the progression of the disease on the distal surfaces of teeth #18 and #19.
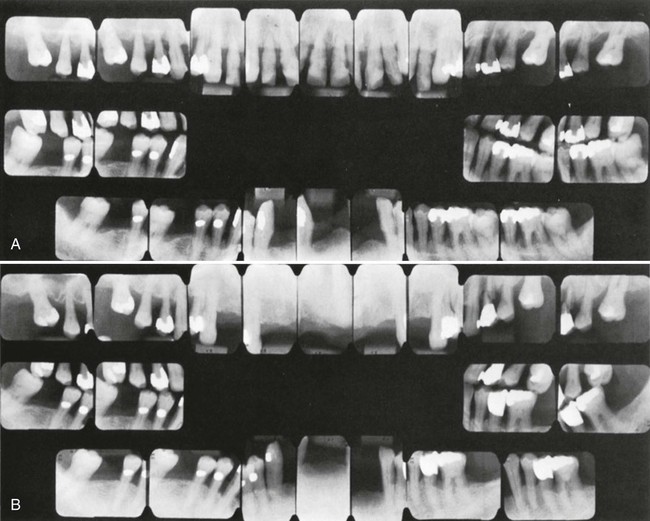
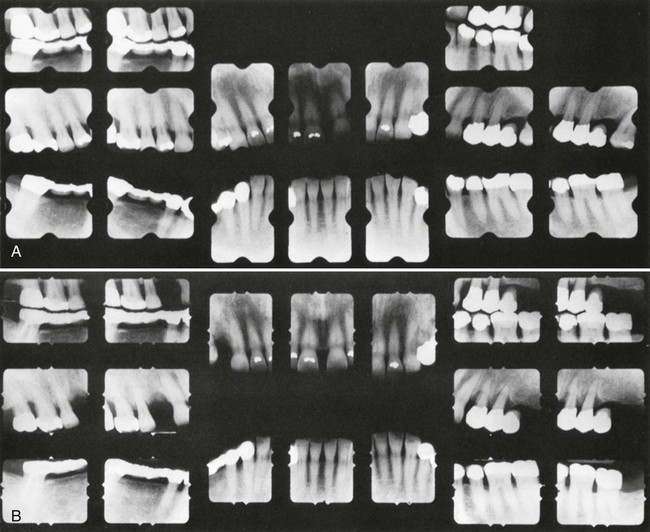
A, Initial radiographs showing a very advanced case. The maxillary arch had extractions and nonsurgical treatment. A plastic partial denture was placed and was expected to grow into a full denture within a few years. The mandibular arch was treated with periodontal surgery, and a permanent, metal and plastic, removable partial denture was placed. B, Radiographs taken 8 years later. The patient performed good oral hygiene and had 3-month recalls. Teeth #12 and #15 required extraction.
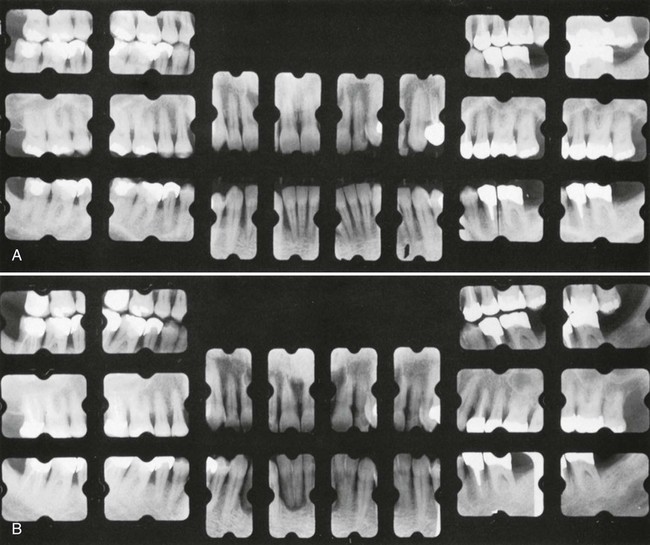
Radiographic examination must be individualized,27 depending on the initial severity of the case and the findings at the recall visit (Table 69-1). These are compared with findings on previous radiographs to check the bone height and look for repair of osseous defects, signs of trauma from occlusion, periapical pathologic changes, and caries.
TABLE 69-1
Radiographic Examination of Recall Patients for Supportive Periodontal Treatment*
| Patient Condition/Situation | Type of Examination |
| Clinical caries or high-risk factors for caries. | Posterior bite-wing examination at 6- to 18-month intervals. |
| No clinical caries and no high-risk factors for caries. | Posterior bite-wing examination at 24- to 36-month intervals. |
| Periodontal disease not under good control. | Periapical and/or vertical bite-wing radiographs of problem areas every 12 to 24 months. |
| History of periodontal treatment with disease under good control. | Bite-wing examination every 24 to 36 months. |
| Root form dental implants. | Periapical or vertical bite-wing radiographs after prosthetic placement and at 12 and 24 months, Then every 24 to 36 months unless clinical problems arise. |
| Transfer of periodontal or implant maintenance patients. | Full-mouth series if a current set is not available. If full-mouth series has been taken within 24 months, radiographs of implants and periodontal problem areas should be taken. |
*Adapted from Guide to Patient Selection and Limiting Radiation Exposure. American Dental Association website. http://ada.org/2760/aspx. Accessed May 24, 2013.
Checking of Plaque Control
To assess the effectiveness of their plaque control, patients should perform their hygiene regimen immediately before the recall appointment. Plaque control must be reviewed and corrected until the patient demonstrates the necessary proficiency, even if additional instruction sessions are required. Patients instructed in plaque control have less plaque and gingivitis than uninstructed patients,7,58,59 and the amount of supragingival plaque affects the number of subgingival anaerobic organisms.15,55
Treatment
The required scaling and root planing are performed, followed by an oral prophylaxis (see Chapter 46). Care must be taken not to instrument normal sites with shallow sulci (1 to 3 mm deep) because studies have shown that repeated subgingival scaling and root planing in initially normal periodontal sites result in significant loss of attachment.33 Irrigat/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses