Recent Advances in Surgical Therapy
Lasers in Periodontal Therapy
In deciding if a new technology, such as laser, should be incorporated into clinical practice, studies are required to demonstrate equivalence or superiority in clinical trials. The usual goals of clinical studies are to determine if a new product, therapy, or technique is superior or equivalent to an established therapy or a placebo. Superiority is usually defined as greater than 20% of the effect of the established treatment. If the new treatment is no greater than or less than 20% of the effect of the established treatment, then the two groups are considered equivalent. Despite the fact that two treatment modalities are equivalent, there may be other advantages such as safety, cost, or ease of use that may warrant the utilization of the new technology.29 The sample size required to statistically test superiority versus equivalence is generally much larger than what has been used in clinical trials for implementation of lasers. Additionally, the limited number of longitudinal clinical trials and cohort studies for each type of laser (i.e., carbon dioxide [CO2], neodymium : yttrium-aluminum-garnet [Nd : YAG], erbium : yttrium-aluminum-garnet [Er : YAG], GaAS [diode]) makes implementation of this new technology for periodontal application difficult. Recently, meta-analysis of the available reports has been used in an attempt to define if laser could provide additional benefits.83–86 Despite the large number of reports, the lack of well-designed parallel randomized clinical trials on which meta-analyses are based are minimal. As such, the conclusions should be interpreted with caution. Nevertheless, this chapter discusses the current literature and some of the clinical applications of laser for periodontal therapy.
Physics of Lasers and Their Biological Interactions
Laser is an acronym for light amplification by stimulated emission of radiation and functions by transmitting light energy to tissues. It is a collimated, focused monochromatic ray of light. The energy beam reacts with a target material by being absorbed, reflected, or scattered. A target tissue absorbs the light. If it is well absorbed, the energy virtually explodes the cell (and extracellular matrix) in a process called ablation.66 The efficiency of ablation is related to the wavelength and the affinity of the target tissue. If the wavelength is not well absorbed, there is scattering and a thermal reaction occurs with carbonization, charring, and melting. The clinician must understand how this energy is affecting the target tissue and the adjacent tissues as well.
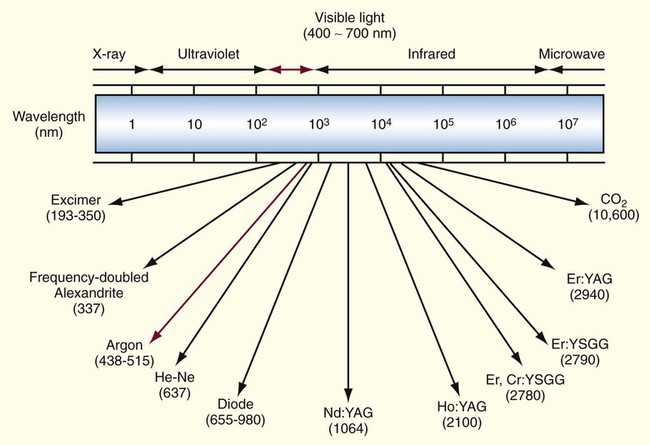
Lasers are named in relationship to the active element(s) that when stimulated, generate the energy beam. The range of lasers used in dentistry consist of CO2, Nd : YAG, HO : YAG, Er : YAG, Er, CT : YSGG, Nd : YAP, GaAs (diode) and argon lasers with the wavelengths delivered as either a continuous, pulsed (gated), or running pulse waveform.15 Reported periodontal applications for these lasers include soft tissue incision and ablation; subgingival curettage, scaling of root surfaces, bacterial elimination, osteoplasty, and ostectomy. Because of the varying absorption spectrum for each tissue type, each laser has its unique wavelength spectrum. In understanding the use of lasers, considerations that each type of wavelength, which the laser functions with, will have its own set of characteristics (Figure 65-1).
Lasers were first used in the 1960s for dental applications.28,46,52,67,86 They were initially used for removing hard tissue and caries but offered little benefit over standard rotary instruments. Recent advances in new wavelengths, delivery units, and power maximums have refocused the use of lasers on both the soft and/or hard tissues (Table 65-1).24,44 When applied to the various periodontal tissues such as the gingiva, periodontal ligament, cementum, dentin, and bone, the biological interactions will be unique for that wavelength. Gingiva, dentin, enamel, and bone are all composite structures of inorganic and organic elements. Gingiva is comprised of fibrous connective tissue, extracellular matrix components (including melanin pigmentation), and 70% water. Bone is comprised of 67% inorganic minerals (calcium hydroxyapatite) and 33% organic elements (collagen, noncollagenous proteins, and water). Other factors to consider are the textures and the densities of these structures. An example is the varying percentages of mineralized structures, blood vessels, and fluid found with cortical and cancellous bone. With the differences in tissue makeup, the laser energy beam will encounter many fluctuations in absorption and scattering, regardless of the wavelength. So when considering clinical application, it is important to appreciate not only what can be accomplished clinically but also the type of laser being used.
TABLE 65-1
Types of Lasers Currently Used in Dentistry
| Laser Medium | Wavelength (nm) | Dental Uses |
| Argon | 488-514 | Tooth bleaching and advanced curing lights |
| Carbon dioxide (CO2) | 10,600 | Gingivectomy/gingivoplasty, second-stage implant exposure, periodontal curettage (advocated but not evidence based) |
| Diode | 655-980 | Gingivectomy/gingivoplasty, oral medicine uses (aphthous ulcer therapy, biopsies, dentinal desensitizing), second-stage implant exposure, periodontal curettage (advocated but not evidence based) |
| Neodymium : yttrium-aluminum-garnet (Nd : YAG) | 1064 | Gingivectomy/gingivoplasty, oral medicine uses (aphthous ulcer therapy, biopsies, dentinal desensitizing), second-stage implant exposure, periodontal curettage (advocated but not evidence based) |
| Erbium : YAG (Er : YAG) | 2940 | Gingivectomy/gingivoplasty, oral medicine uses (aphthous ulcer therapy, biopsies, dentinal desensitizing), second-stage implant exposure, periodontal curettage (advocated but not evidence based), hard tissue cutting (dentin and osseous) |
| Erbium, chromium : yttrium (Er,Cr : YSGG) | 2780 | Gingivectomy/gingivoplasty, oral medicine uses (aphthous ulcer therapy, biopsies, dentinal desensitizing), second-stage implant exposure, periodontal curettage (advocated but not evidence based), hard tissue cutting (dentin and osseous) |
The wavelengths of erbium : YAG (Er : YAG) (2790 nm) and erbium, chromium : yttrium (Er,Cr : YSGG) (2780 nm) lasers have a positive affinity for both water and hydroxyapatite. The specificity for hydroxyapatite also allows cutting hard tissues such as bone, dentin, or enamel.6–10 The selection of the type of laser is ultimately based on the amount of energy transmitted to that tissue during a procedure.
Photothermal energy is measured in watts (W = joules/second). There are other factors to consider besides the amount of watts being delivered. The amount of energy delivered to the target can be altered if it is continuous, gated, and/or pulsed. A continuous laser transmits more energy than a pulsed laser to the target tissues. Hertz (Hz) is the cycle/second of a pulsed laser. It is imperative when comparing techniques and the type of laser that watts, hertz, and total time in contact with surgical sites be evaluated. The benefits of using a laser can be compromised if the energy is excessive. Care must be taken to avoid the transmission of excessive thermal energy to the tissues adjacent to the target because it can result in cellular damage. In a study with the Nd : YAG laser, wound healing was compared to that of a scalpel used for soft tissue incisions. Two different energy levels were used. Healing with the laser was excellent with a setting of 1.75 W, 20 Hz. When the energy was increased to 3 W, 20 Hz, the healing was delayed. The scalpel was better compared to the laser at this higher energy setting.69 This study demonstrated that it is not only the type of laser that is used but also the energy level and total quantity that is delivered to the tissue that make a difference. Different energy levels and quantity may have different effects. The secondary message from this study that it is inappropriate to have the result of one study compared to another unless the same type of laser and energy setting and quantity is being used. The literature shows a wide range of approaches for laser application.
Advantages and Disadvantages of Laser Therapy
There are many advantages to using laser therapy, including better visualization of cutting, patient acceptance, and the detoxification of a wound. Other advantages are less invasive surgery to gain access and minimal wound contraction and scarring.4,34,48 Many of these concepts of laser therapy are positive, although others still require research.35 There are clearly many favorable applications for lasers in periodontal therapy but further studies are necessary as to which procedures laser therapy can be best applied.
While there are advantages, conversely, lasers can also generate excessive temperature changes in hard tissues as reported from the studies by Eriksson and Albrektsson.24 The exposure of bone to temperatures ≥47° C (116.6° F) can induce cellular damage and osseous resorption. Extreme temperature levels of ≥60° C (140° F) result in tissue necrosis.44
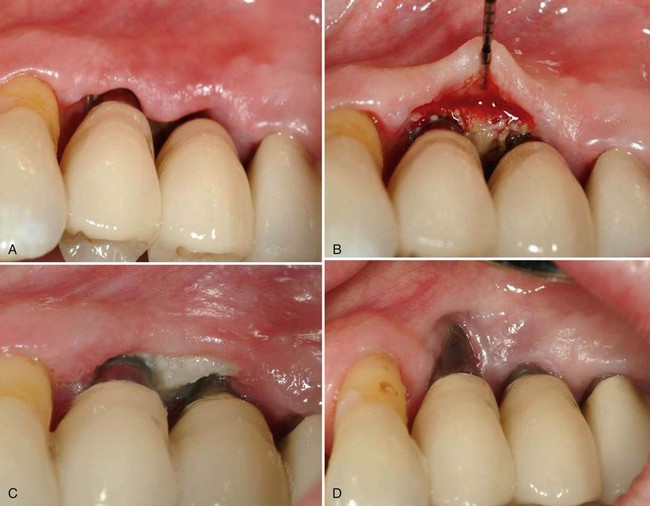
Overexposure of laser energy has been the basis for reports of tissue damage and destruction of the periodontium. As such, it has been the basis for malpractice suits. Misuse of new technologies can result in “cutting-edge” clinicians finding their early experiences resulting in disastrous results (Figure 65-2). To avoid these negative results, knowledge of the laser mechanics and technique are essential to avoid causing damage to the adjacent tissues. Once mastery of the information has been achieved, it is critical to identify the desired laser application(s) and the fashion in which it will be used. In reviewing this chapter, you will find that most laser applications are at best equivalent. With the significant investment for lasers, it behooves the clinician to be clear as to the additional benefits that justifies this type of expense.
Laser Use in Periodontal Procedures
Periodontal Esthetic Applications and Functional Crown Lengthening
Several types of laser wavelengths have been reported to be effective for soft tissue procedures.4,48,49 Appropriate use of laser for procedures such as frenectomy, gingivectomy/gingivoplasty, recontouring of drug-induced gingival overgrowth, short crowns associated with altered/delayed passive eruption, and management of mucosal tissue/pericoronitis situations distal of mandibular second molars have been well documented. Some of the positive aspects of laser therapy are good visibility during the surgical procedure as a result of coagulation, hemostasis, and minimal tissue damage adjacent to the laser wound are also advantages. Additionally, laser therapy can potentially offer extreme precision and may be easier than using a scalpel.
Esthetic applications for gingivectomy and gingivoplasty procedures allow delicate tissue shaping. The laser is effective for the removal of pigmentation from the gingival tissues, which can significantly improve the esthetics of highly pigmented areas. The CO2, diode, and Nd : YAG lasers have been used for depigmentation.3,53
Some clinicians advocate the use of lasers for crown-lengthening procedures. Whereas crown lengthening involving only soft tissue can be effectively be performed with a wide variety of lasers, lasers may be somewhat advantageous for hemostatic control during tissue removal. For functional crown lengthening involving osseous contouring, the use of laser is controversial. (See Chapter 60 for a discussion of crown-lengthening surgery.) The Er : YAG and Er,Cr : YSGG lasers have been advocated as one approach for clinical crown lengthening without gingival flap reflection.25,26,38,88,94–97 The Er,Cr : YSGG laser can safely cut bone without burning or altering the calcium-to-phosphate ratio of the irradiated bone.38,95 This approach has been described in case technique reports and case series, but there are no controlled longitudinal or cohort studies supporting the use of lasers for clinical crown lengthening using the closed-flap technique.
Decision making for the use of lasers in crown lengthening in an open or closed approach is based on osseous biotypes.39 In the closed approach, the Er,Cr : YSGG or Er : YAG laser can be used only in the medium gingival biotype cases in which the width of the osseous crest is approximately 1 mm in thickness and may be limited to situations where only 1 to 2 mm of osseous removal is required. In this technique, sounding is indicated after the external gingivectomy to determine the thickness of the osseous biotype and to determine the amount of bone removal that is required. The laser tip is placed in contact with the bone, and the laser is fired for 1 to 2 seconds. The tip is moved slowly around the tooth until the biologic width is achieved. The osseous removal is verified by sounding, and detailing is performed with a small chisel (Figure 65-3). This technique can be surgically conservative and result in symmetric gingival levels in the esthetic zone.4,43,48




Further issues of concern include: (1) Is there sufficient tactile sense to permit adequate osseous contouring with properly defined osseous anatomical dimension required for crown lengthening? (2) Is there any root surface damage?15 Given these concerns and the possible retreatment because of tissue rebound or poor tissue healing suggest that this is not a superior or equivalent technique as compared to traditional functional crown lengthening that requires osseous contouring.
Nonsurgical Laser Periodontal Therapy
Two of the purported benefits of using laser-mediated periodontal therapy are for subgingival curettage and significantly decreasing subgingival pathogenic bacteria.80 In the clinical situation, periodontal pathogenic bacteria exist in a protective biofilm in a periodontal pocket. In vitro laboratory analysis of laser bactericidal properties is not clinically relevant in that these bacteria do not exist as a suspension or monolayer. The protective nature of the biofilm and the disruption of this biofilm result in renewal microbial colonization of this micro niche. In addressing these issues for each laser type, one needs to ask the following questions:
1. Do the in vivo studies indicate reduction in pathogenic bacteria as compared to conventional scaling and root planing?
2. Are the microbial changes sustained or does microbial colonization reinitiate?
3. Are there any differences in clinical parameters following laser-mediated versus conventional scaling and root planing? When evaluating nonsurgical periodontal therapy, gain in clinical attachment level (CAL) represents the gold standard. Pocket depth (PD) and levels of subgingival microbes are important because they correlate with changes in CAL.14,71
4. Are there changes in root surface in vitro conditions?
In evaluating laser (i.e., Nd : YAG, Er : YAG, and diode lasers) used for nonsurgical periodontal therapy, these questions need to be addressed. Three recent reviews on the effect of laser therapy as an adjunct of nonsurgical periodontal treatment in patients with chronic periodontitis have been published.36,
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses