Resective Osseous Surgery
Osseous surgery can be either additive or subtractive in nature. Additive osseous surgery includes procedures directed at restoring the alveolar bone to its original level, whereas subtractive osseous surgery is designed to restore the form of preexisting alveolar bone to the level present at the time of surgery or slightly more apical to this level (Figure 60-1).
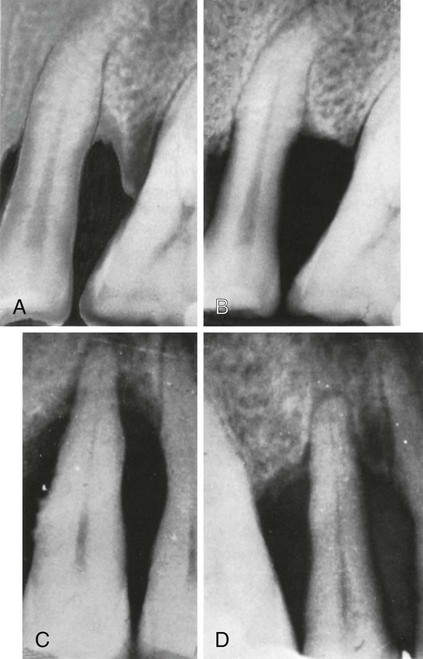
A, Before, and, B, immediately after subtractive osseous surgery; the osseous wall of the two adjoining infrabony pockets has been removed. C, Before, and, D, 1 year after additive osseous surgery; the area has been flapped and thoroughly instrumented, resulting in reconstruction of the interdental and periapical bone. (Courtesy Drs. E.A. Albano and B.O. Barletta, Buenos Aires, Argentina.)
Additive osseous surgery brings about the ideal result of periodontal therapy; it implies regeneration of lost bone and reestablishment of the periodontal ligament, gingival fibers, and junctional epithelium at a more coronal level. This type of osseous surgery is discussed in Chapter 61.
Rationale
Osseous resective surgery necessitates following a series of strict guidelines for proper contouring of alveolar bone and subsequent management of the overlying gingival soft tissues. The specifics of these techniques are discussed later in this chapter. The techniques discussed here for osseous resective surgery have limited applicability in deep intrabony or hemiseptal defects, which could be treated with a different surgical approach (see Chapter 61). Osseous surgery provides the purest and surest method for reducing pockets with bony discrepancies that are not overly vertical and also remains one of the principal periodontal modalities because of its long-term success and predictability.
Osseous resective surgery is the most predictable pocket reduction technique.10–12 However, more than any other surgical technique, osseous resective surgery is performed at the expense of bony tissue and attachment level.1,2,8 Thus its value as a surgical approach is limited by the presence, quantity, and shape of the bony tissues and by the amount of attachment loss that is acceptable.
The major rationale for osseous resective surgery is based on the tenet that discrepancies in level and shapes of the bone and gingiva predispose patients to the recurrence of pocket depth postsurgically.6 Although this concept is not universally accepted3,5 and the procedure induces loss of radicular bone in the healing phase, recontouring of bone is the only logical treatment choice in some cases. The goal of osseous resective therapy is to reshape the marginal bone to resemble that of the alveolar process undamaged by periodontal disease. The technique is performed in combination with apically positioned flaps, and the procedure eliminates periodontal pocket depth and improves tissue contour to provide a more easily maintainable environment. The relative merits of pocket reduction procedures are discussed in Chapters 59 and 61; this chapter discusses the osseous resective technique and how and where it may be accomplished.
It is proposed that the conversion of the periodontal pocket to a shallow gingival sulcus enhances the patient’s ability to remove plaque and oral debris from the dentition. Likewise, the ability of dental professionals to maintain the periodontium in a state free of gingivitis and periodontitis is more predictable in the presence of shallow sulci. The more effective the periodontal maintenance therapy, the greater is the longitudinal stability of the surgical result. The efficacy of osseous surgery therefore depends on its ability to affect pocket depth and to promote periodontal maintenance.11,22,23 The merits of resection versus other treatment procedures are discussed in Chapter 61.
Normal Alveolar Bone Morphology
Knowledge of the morphology of the bony periodontium in a state of health is required to perform resective osseous surgery correctly (Figure 60-2). The characteristics of a normal bony form are as follows:

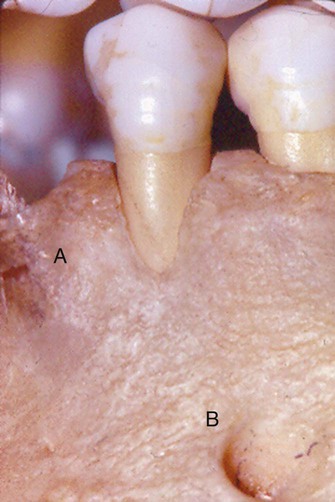
Although a slight amount of attachment may have been lost, this skull demonstrates the characteristics of normal form.
1. The interproximal bone is more coronal in position than the labial or lingual/palatal bone and pyramidal in form.
2. The form of the interdental bone is a function of the tooth form and the embrasure width. The more tapered the tooth, the more pyramidal is the bony form. The wider the embrasure, the more flattened is the interdental bone mesiodistally and buccolingually.
3. The position of the bony margin mimics the contours of the cementoenamel junction. The distance from the facial bony margin of the tooth to the interproximal bony crest is more flat in the posterior than the anterior areas. This “scalloping” of the bone on the facial surfaces and lingual/palatal surfaces is related to tooth and root form, as well as tooth position within the alveolus. Teeth with prominent roots or those displaced to the facial or lingual side may also have fenestrations or dehiscences (Figure 60-3). The molar teeth have less scalloping and a more flat profile than bicuspids and incisors.
Terminology
Procedures used to correct osseous defects have been classified in two groups: osteoplasty and ostectomy.7 Osteoplasty refers to reshaping the bone without removing tooth-supporting bone. Ostectomy, or osteoectomy, includes the removal of tooth-supporting bone. One or both of these procedures may be necessary to produce the desired result.
Positive architecture and negative architecture refer to the relative position of interdental bone to radicular bone (Figure 60-4). The architecture is “positive” if the radicular bone is apical to the interdental bone. The bone has “negative” architecture if the interdental bone is more apical than the radicular bone. Flat architecture is the reduction of the interdental bone to the same height as the radicular bone.
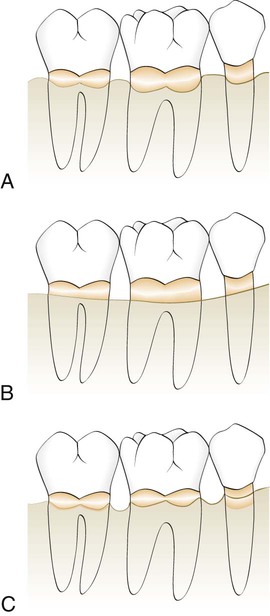
A, Positive bony architecture. B, Flat bony architecture. C, Reversed, or negative, bony form.
Osseous form is considered to be “ideal” when the bone is consistently more coronal on the interproximal surfaces than on the facial and lingual surfaces. The ideal form of the marginal bone has similar interdental height, with gradual, curved slopes between interdental peaks (Figure 60-5).
Factors in Selection of Resective Osseous Surgery
The relationship between the depth and configuration of the bony lesion(s) to root morphology and the adjacent teeth determines the extent that bone and attachment is removed during resection. Bony lesions have been classified according to their configuration and number of bony walls.9 The technique of ostectomy is best applied to patients with early to moderate bone loss (2 to 3 mm) with moderate-length root trunks18 that have bony defects with one or two walls. These shallow-to-moderate bony defects can be effectively managed by osteoplasty and osteoectomy. Patients with advanced attachment loss and deep intrabony defects are not candidates for resection to produce a positive contour. To simulate a normal architectural form, so much bone would have to be removed that the survival of the teeth could be compromised.
Two-walled defects, or craters, occur at the expense of the interseptal bone. As a result, they have buccal and lingual/palatal walls that extend from one tooth to the adjacent tooth. The interdental loss of bone exposes the proximal aspects of both adjacent teeth. The buccal–lingual interproximal contour that results is opposite to the contour of the cementoenamel junction of the teeth (Figure 60-6, A and B). Two-walled defects (craters) are the most common bony defects found in patients with periodontitis.14,20 If the facial and lingual plates of this bone are resected, the resultant interproximal contour would become more flattened or ovate (Figure 60-6, C and D). However, confining resection only to ledges and the interproximal lesion results in a facial and lingual bone form in which the interproximal bone is located more apically than the bone on the facial or lingual aspects of the tooth. This resulting anatomic form is reversed, or negative, architecture17,18,22 (Figure 60-6, C and D).
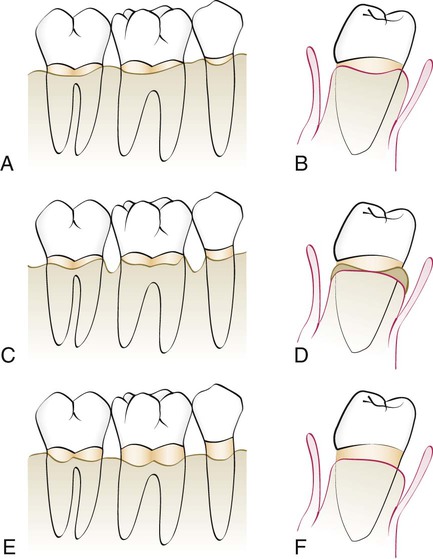
A and B, Diagram of facial and interproximal bony contours after flap reflection. Note the loss of some interproximal bone and cratering. C and D, Line angles; this is only osteoplasty and has resulted in a reversed architecture. E and F, Ostectomy on the facial and lingual bone and the removal of the residual widow’s peaks to produce a positive bony architecture.
Although the production of a reversed architecture minimizes the amount of ostectomy that is performed, it is not without consequences.5 Peaks of bone typically remain at the facial and lingual/palatal line angles of the teeth (widow’s peaks). During healing, the soft tissue tends to bridge the embrasure from the most coronal height of the bone on one tooth to the most coronal heights on the adjacent teeth. The result is therefore the tendency to replicate the attachment contour on the tooth. The interproximal soft tissues invest these peaks of bone, which may subsequently resorb with a tendency to rebound without gain in attachment over time. Interproximal pocket depth can recur.22,24
Ostectomy to a positive architecture requires the removal of the line-angle inconsistencies (widow’s peaks), as well as some of the facial, lingual, and palatal and interproximal bone. The result is a loss of some attachment on the facial and lingual root surfaces but a topography that more closely resembles normal bone form before disease (see Figure 60-6, E and F). Proponents of osseous resection to create a positive contour believe that this architecture, devoid of sharp angles and spines, is conducive to the formation of a more uniform and reduced soft-tissue dimension postoperatively.17,21 The therapeutic result is less pocket depth and increased ease of periodontal maintenance by the patient, dental hygienist, or dentist.
The amount of attachment lost from the use of ostectomy varies with the depth and configuration of the treated osseous defects. Osseous resection applied to two-wall intrabony defects (craters), the most common osseous defects, results in attachment loss at the proximal line angles and the facial and lingual aspects of the affected teeth without affecting the base of the pocket. The extent of attachment loss during resection to a positive architecture has been measured. When the technique is properly applied to appropriate patients, the mean reduction in attachment circumferentially around the tooth has been determined to be 0.6 mm at six probing sites.22 In practical terms, this means that the technique is best applied to interproximal lesions 1 to 3 mm deep in patients with moderate-to-long root trunks.17 Patients with deep, multiwalled defects are not candidates for resective osseous surgery. They are better treated with regenerative therapies or by combining osteoplasty to reduce bony ledges and to facilitate flap closure with new attachment/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses