Gingival Surgical Techniques
Gingival Curettage
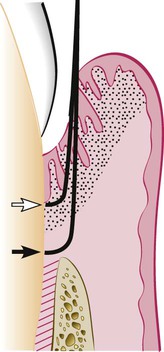
Curettage in periodontics has been defined as gingival and subgingival curettage (Figure 56-1). Gingival curettage consists of the removal of the inflamed soft tissue lateral to the pocket wall and the junctional epithelium. Subgingival curettage refers to the procedure that is performed apical to the junctional epithelium and that severs the connective tissue attachment down to the osseous crest.
Rationale
Curettage may also eliminate all or most of the epithelium that lines the pocket wall and the underlying junctional epithelium. Curettage for this purpose is still valid, particularly when an attempt is made for new attachment, as occurs in intrabony pockets. However, opinions differ with regard to whether scaling and curettage consistently remove the pocket lining and the junctional epithelium. Some investigators report that scaling and root planing tear the epithelial lining of the pocket without removing either it or the junctional epithelium.33 Others claim that both epithelial structures6,7,32 and sometimes the underlying inflamed connective tissue34 are removed by curettage. Some investigators have reported that the removal of the pocket lining and the junctional epithelium by curettage is not complete.51,54,57
Curettage and Aesthetics.
There are many instances in which a surgical flap is necessary for access to the root surface for scaling and root planing. A surgical technique that has been specially designed to minimize gingival recession and preserve the interdental papilla is the papilla preservation technique (see Chapter 59).
Indications
1. Curettage can be performed as part of new attachment attempts in moderately deep intrabony pockets located in accessible areas in which a nonflap type of “closed” surgery is indicated.
2. Curettage can be attempted as a nondefinitive procedure to reduce inflammation when aggressive surgical techniques (e.g., flaps) are contraindicated in patients as a result of their age, systemic problems, psychologic problems, or other factors. It should be understood that, in these patients, the goal of pocket elimination is compromised, and their prognosis is impaired. The clinician should attempt this approach only when the indicated surgical techniques cannot be performed and both the clinician and the patient have a clear understanding of its limitations.
3. Curettage is also frequently performed on recall visits45 as a method of maintenance treatment for areas of recurrent inflammation and pocket depth, especially where pocket reduction surgery has previously been performed. Careful probing should establish the extent of the required root planing and curettage.
Procedure
Basic Technique.
Curettage does not eliminate the causes of inflammation (i.e., bacterial plaque and deposits). Therefore, curettage should always be preceded by scaling and root planing, which is the basic periodontal therapy procedure (see Chapter 46). The use of local infiltrative anesthesia for scaling and root planing is optional. However, gingival curettage will always require some type of local anesthesia.
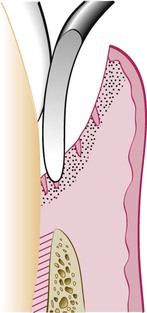
The curette is selected so that the cutting edge is against the tissue (e.g., Gracey no. 13 or 14 for mesial surfaces, Gracey no. 11 or 12 for distal surfaces). Curettage can also be performed with a 4R-4L Columbia Universal curette. The instrument is inserted to engage the inner lining of the pocket wall, and it is then carried along the soft tissue, usually in a horizontal stroke (Figure 56-2). The pocket wall may be supported by gentle finger pressure on the external surface. The curette is then placed under the cut edge of the junctional epithelium to undermine it.
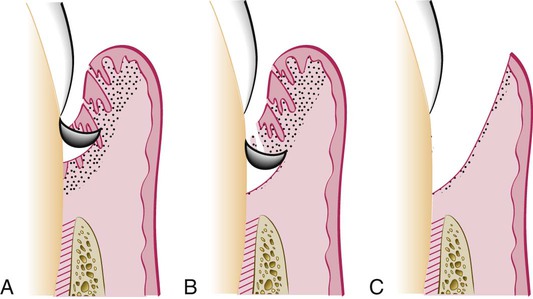
During subgingival curettage, the tissues attached between the bottom of the pocket and the alveolar crest are removed with a scooping motion of the curette to the tooth surface (Figure 56-3). The area is flushed to remove debris, and the tissue is partly adapted to the tooth by gentle finger pressure. In some cases, the suturing of separated papillae and the application of a periodontal pack may be indicated.
Other Techniques.
Excisional New Attachment Procedure.
The excisional new attachment procedure has been developed and used by the US Naval Dental Corps.40,62,63 It is a definitive subgingival curettage procedure that is performed with a knife. The excisional new attachment procedure technique is as follows:
1. After adequate anesthesia, make an internal bevel incision from the margin of the patient’s free gingiva apically to a point below the bottom of the pocket (Figure 56-4). Carry the incision interproximally on both the facial and the lingual side, and attempt to retain as much interproximal tissue as possible. The intention is to cut the inner portion of the soft-tissue wall of the pocket all around the tooth.
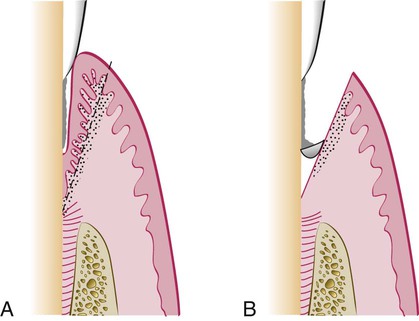
2. Remove the excised tissue with a curette, and carefully perform root planing on all exposed cementum to achieve a smooth, hard consistency. Preserve all connective tissue fibers that remain attached to the root surface.
3. Approximate the wound edges. If they do not meet passively, recontour the bone until good adaptation of the wound edges is achieved. Place sutures and a periodontal dressing.
Ultrasonic Curettage.
The use of ultrasonic devices has been recommended for gingival curettage.35 When applied to the gingiva of experimental animals, ultrasonic vibrations disrupt tissue continuity, lift off the epithelium, dismember collagen bundles, and alter the morphologic features of fibroblast nuclei.20 Ultrasound is effective for debriding the epithelial lining of periodontal pockets. This results in a narrow band of necrotic tissue (microcauterization), which strips off the inner lining of the pocket.
The Morse scaler-shaped and rod-shaped ultrasonic instruments are used for this purpose. Some investigators found ultrasonic instruments to be as effective as manual instruments for curettage35,50,64 and that such tools resulted in less inflammation and less removal of underlying connective tissue. The gingiva can be made more rigid for ultrasonic curettage by injecting anesthetic solution directly into it.10
Caustic Drugs.
Since early in the development of periodontal procedures,53,61 the use of caustic drugs has been recommended to induce a chemical curettage of the lateral wall of the pocket or even the selective elimination of the epithelium. Drugs such as sodium sulfide, alkaline sodium hypochlorite solution (Antiformin),8,24,26 and phenol4,9 have been proposed and then discarded after studies indicated their ineffectiveness.5,18,26 The extent of tissue destruction with these drugs cannot be controlled, and they may increase rather than reduce the amount of tissue to be removed by enzymes and phagocytes.
Healing After Scaling and Curettage
The restoration and epithelialization of the sulcus generally require 2 to 7 days,27,34,37,57 and restoration of the junctional epithelium occurs in animals as early as 5 days after treatment. Immature collagen fibers appear within 21 days. Healthy gingival fibers that are inadvertently severed from the tooth and tears in the epithelium are repaired during the healing process.33,46 Several investigators hav/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses