CHAPTER 53 Geriatric Pharmacology
In 2008, the elderly—individuals 65 years old or older—numbered 38.9 million and represented 12.8% of the U.S. population60; by 2030, they are expected to represent 20% of the population and number approximately 72 million. Not only is the total ≥65 years group growing faster than the population as a whole, but between the years 2003 and 2030 the group 85 years old and older is expected to increase from 4.7 million to 9.6 million.61
Of special interest to dentists is the fact that the newer cohorts of older adults are and will be in better oral health than before.21,43 The rate of edentulousness has declined,39,62,63,70 and the number of retained teeth among dentate adults has increased.29,37,39,62,63 With this trend among dentate older adults has emerged an understanding that this population has similar needs for routine restorative and periodontal treatments as younger adults.20,29,63 An increasing number of elderly individuals will need the kind of dental treatment that was formerly rare in elderly patients. This treatment requires, among other things, antianxiety drugs, analgesics, local anesthetics, and anti-inflammatory drugs. The dentist will be confronted by an increasing number of ambulatory, community-dwelling elderly patients with a significant burden of systemic disease and medication use.
As people age, they are more likely to be seen at the dental office with various diseases, especially chronic diseases, for which they take numerous drugs that are strong in effect and potentially toxic. Americans 65 years old and older take a disproportionately high percentage of all drugs prescribed.13,44 Studies of ambulatory populations indicate that although 80% to 90% of older adults take at least one medication, most take two or more. The most commonly used drugs are agents affecting the cardiovascular system, analgesic and anti-inflammatory drugs, psychotherapeutic medications, and gastrointestinal preparations such as laxatives and antacids. Approximately 40% of the medications are prescribed to patients to be taken “as necessary,” with an average of three drugs per patient.47,50
The number of medications prescribed to individuals of any age increases the risk of adverse drug reactions, drug interactions, and other health-related problems associated with the use and misuse of medications.27,47,50 Potential problems in older adults are compounded by age-related physiologic changes that may place these individuals at greater risk. The misuse of medications among elderly patients is considered a major health care problem.19,41,50 Finally, many segments of society, not the least important of which are health care providers, have become sensitized to the nonmedical problems common among elderly individuals (loneliness, depression, poverty, poor nutritional status) and have come to understand how these can complicate therapeutic management.
PHYSIOLOGIC CHANGES ASSOCIATED WITH AGING
Studies of the aging process in community-dwelling, healthy (presumed disease-free) individuals have provided insights into the process of biologic aging. These studies have been either cross-sectional studies, in which different-aged individuals are assessed at the same point in time, or longitudinal studies, in which the same individuals are assessed at different times as they “age in place.” Although the former studies are easier and quicker to complete, they limit inferences to age differences rather than age-related changes because of the limitations in controlling for and measuring individual differences in biology and behavior. Results of cross-sectional and longitudinal studies have reported a gradual decline in performance from the third decade through the seventh and eighth decades in a broad range of physiologic functions, including renal function, pulmonary function, cardiac function, and nerve conduction velocity (Figure 53-1).54
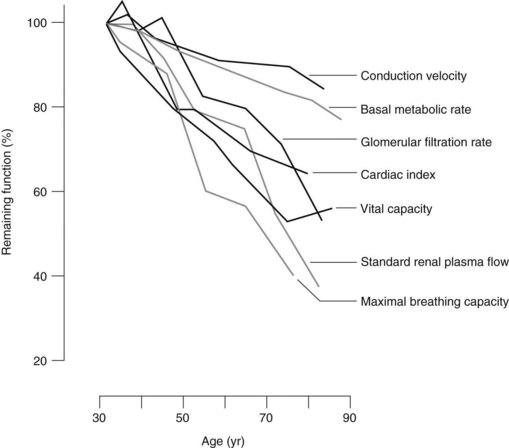
FIGURE 53-1 Influence of age on measures of physiologic function beginning at age 30 (100% of remaining function).
(From Miller RD: Anesthesia for the elderly. In Miller RD, editor: Anesthesia, ed 2, New York, 1986, Churchill Livingstone.)
Table 53-1 summarizes age-related changes in drug disposition that have potential importance to drug use. These alterations affect the absorption, distribution, biotransformation, and excretion of drugs; the specific features of these changes are considered later. A well-documented decline in homeostatic competence occurs in elderly individuals, which accounts for the increased incidence of postural hypotension with age,10 the increasing sluggishness of thermoregulation, and the fact that elderly individuals are less able to compensate rapidly for the hypotensive effects of an antihypertensive drug.24 Elderly individuals undergo physiologic changes that can be characterized as normal concomitants of the aging process, but they also experience changes related to disease and medication. Aging represents an interplay among the physiology of aging, disease, and the cumulative effects of behavioral and lifestyle choices (e.g., sedentary living and tobacco use versus regular exercise and abstention from tobacco); as a result, the elderly population is a more heterogeneous population than that of children between birth and puberty.65
TABLE 53-1 Summary of Age-Related Changes That Affect Drug Disposition in Older Adults
| PHARMACOKINETIC PROPERTY | PHYSIOLOGIC CHANGE | POSSIBLE INFLUENCE ON DRUG EFFECT |
|---|---|---|
| Absorption | ↑Gastric pH | Increased absorption of drugs inactivated by stomach acid |
| ↓Absorptive surface | Minor effect | |
| ↓Splanchnic blood flow | Minor effect | |
| ↓Gastrointestinal motility | Minor effect | |
| Distribution | ↓Cardiac output | Impaired delivery of drugs to organs of greater acute elimination; effects on CNS |
| ↓Total body water | Increased concentration and effect of drugs distributed in body water | |
| ↓Lean body mass | Increased concentration and effect of drugs distributed in lean body mass | |
| ↓Plasma albumin | Increased effect of, and interaction between, drugs extensively bound to albumin | |
| ↑α1-Acid glycoprotein | Minor effect | |
| ↑Body fat | Increased sequestration of lipophilic drugs in fat | |
| Metabolism | ↓Hepatic mass and enzyme activity | Decreased phase I metabolism of some drugs |
| ↓Hepatic blood flow | Decreased metabolism of drugs normally rapidly cleared by the liver | |
| Excretion | ↓Renal blood flow | Decreased renal elimination of water-soluble drugs and metabolites |
| ↓Glomerular filtration rate | Decreased renal excretion of water-soluble drugs and metabolites | |
| ↓Tubular secretion | Decreased renal elimination of drugs and metabolites actively secreted into urine |
CNS, Central nervous system.
NONPHYSIOLOGIC ASPECTS OF AGING
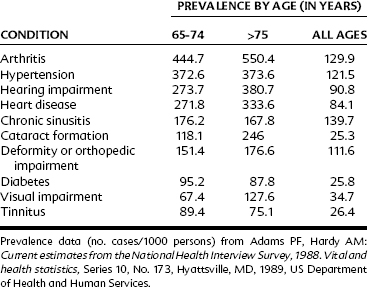
Multiple Disease States
Elderly individuals have more health problems, especially chronic diseases and conditions, than younger individuals. Table 53-2 lists the most prevalent chronic conditions among older adults. Some of these diseases are degenerative (e.g., cataracts, detached retina), others are caused by cumulative exposure to environmental contaminants (e.g., cases of chronic obstructive pulmonary disease and cancer), and still others are the consequence of changing metabolic processes commonly seen in aging (e.g., decreased bone density with increasing age). Older adults have an increased incidence of all varieties of heart disease (e.g., arrhythmias, myocardial infarction, valvular disease), renal disease, atherosclerosis, arthritis, diabetes, osteoporosis, and various gastrointestinal problems. They also experience declines in humoral-mediated and cell-mediated immune responses (leading to a decreased resistance to infectious diseases) and various sensory and musculoskeletal impairments. More than four out of five individuals 65 years old and older have at least one chronic illness, and multiple coexisting conditions are common. The leading chronic health conditions for this age group are arthritis, hypertensive disease, and heart disease.2,12
Although elderly individuals represent less than 13% of the population, they account for 30% of hospitalizations23 and 32% of drug use.17 The symptoms of disease in older adults may often manifest differently in elderly individuals compared with younger individuals. Infections are sometimes manifested by tachycardia instead of fever in older individuals. Transient or episodic symptoms may be forgotten, misreported, or misinterpreted.
Numerous studies have shown that older adults, because of the higher prevalence of chronic disease, are the principal consumers of drugs.44,48 Their use of over-the-counter and prescription medications for the treatment of chronic diseases has dual implications. These agents can provide a cure or palliative treatment of a disease in a nontoxic and economical manner. Because of the age-related changes in physiologic status and age-dependent and age-related diseases,9 however, medications can induce adverse reactions that can be a major source of morbidity or mortality.27,49
Adverse Drug Reactions
The incidence of adverse drug reactions among older adults is much greater than among younger individuals; this increase is related mostly to polypharmacy (multiple drug use). Other important factors in the occurrence of adverse drug reactions include multiple diseases (especially chronic diseases), hepatic or renal insufficiency, small body size, malnutrition, and previous drug reactions. Important adverse reactions include side effects (e.g., dry mouth with tricyclic antidepressant medication), drug allergy (e.g., pruritus or hives), and toxic reactions (e.g., digitalis toxicity).35 Toxic reactions are especially important in older adults and may be caused by a broad range of potential pharmacodynamic changes (age-related changes in drug sensitivity) or pharmacokinetic changes (including decreased renal function and changes in lean body mass and water content).
Because most adverse drug reactions are preventable, the clinician should be aware of the patient’s medical history, drug history, current list of medications (over-the-counter and prescribed), the pharmacologic characteristics of each agent used, and any abnormal physiologic factors that can affect drug action. Although the incidence of adverse reactions increases among older patients in part because of polypharmacy, actions of a single powerful agent can produce severe adverse reactions for elderly patients. Many drugs commonly prescribed by dentists can produce various harmful reactions in patients. As illustrated in Table 53-3, various drug classes can be of potential risk to older patients. Cephalosporins commonly prescribed to treat infections can produce deleterious effects. Cefoperazone, cefamandole, and cefotetan can prolong prothrombin time and partial thromboplastin time, which can impair hemostasis.16,46 Other antibiotics, such as clindamycin, can markedly increase the incidence of gastrointestinal problems such as diarrhea and colitis in patients older than 60 years.26,45
TABLE 53-3 Age-Related Increased Risk of Toxicity with Commonly Prescribed Dental Agents
| DRUG | INCREASED RISK FOR ELDERLY PATIENTS |
|---|---|
| Clindamycin | Diarrhea and colitis |
| Metronidazole | Toxic plasma concentrations (patients >70 yr old) |
| Cephalosporins | Impaired clotting mechanisms and bleeding problems |
| NSAIDs | Compromised renal and gastrointestinal function |
| Opioid analgesics | Increased plasma half-life, respiratory depression |
| Glucocorticoids | Muscle wasting and osteoporosis with long-term therapy |
| Benzodiazepines | Impaired memory and decrements in psychomotor performance |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses