CHAPTER 51 Drugs of Abuse
Drug abuse can be defined as an inappropriate use of a drug for a nonmedical purpose. Drug abuse is considered to cause harm to the individual abuser and to society as a whole. Many variables not directly related to a drug can influence whether a given individual becomes a drug abuser. Many experts argue that cocaine possesses the greatest potential for abuse based on its pharmacologic characteristics alone. For individuals who try nicotine, the risk of developing an addiction is approximately twice that for individuals who try cocaine, however.7 This statement is not meant to infer that the pharmacologic abuse potential of nicotine is twice that of cocaine; rather, some psychosocial factors are equally important in affecting onset and continuation of drug abuse and addiction. It is beyond the scope of this chapter to discuss these factors related to drug users and their environment; this chapter concentrates solely on the pharmacologic aspects of drugs of abuse.
HISTORIC PERSPECTIVE
Natural products such as hemp flowers, opium, and coca leaves have been used for thousands of years for their ability to cause pleasurable sensations or other alterations in consciousness. Other than alcohol, the first major drugs of abuse in the United States were cocaine and opioids. Throughout the nineteenth century, unregulated opium use led to a plethora of patent medicines containing opium derivatives. As a result, many middle-class Americans became dependent on opium because of promiscuous use of such preparations. Nevertheless, social attitudes toward drug abuse remained relaxed until after the Civil War. The widespread use of morphine by injection for dysentery, malaria, and pain resulted in such large numbers of morphine-addicted veterans that morphine dependence became known as “soldier’s disease.”10
In the early 1900s, the mass media developed the myth of cocaine-crazed renegades committing heinous crimes against society. Opioid dependence was still prevalent, and morphine was the major opioid of abuse. During this period, federal laws were enacted to control the widespread drug abuse problem. The introduction of the Pure Food and Drug Act in 1906, the Harrison Narcotic Act in 1914, and the Narcotic Drugs Import and Export Act in 1922 and the enforcement of these acts by law enforcement officials led to the virtual disappearance of cocaine abuse by the 1930s. The increased cost and reduced street availability of cocaine helped lead to the increase of amphetamine as a stimulant drug of abuse. Intravenous (IV) heroin use was also becoming popular, and by 1935 it was as widely abused as morphine. Between World Wars I and II, addiction began to be widely equated with criminality.10 In the case of marijuana, sensationalized accounts of murders perpetrated by individuals under the influence of the “killer weed” led to the passage of the Marihuana Tax Act of 1937, which effectively banned its production, distribution, and sale.
In the 1960s, drug abuse began to make major inroads into middle-class society. The baby-boom generation began experimenting with lysergic acid diethylamide (LSD) and marijuana. Epidemic amphetamine abuse developed during the 1960s, peaking in 1967 with 32 million legal prescriptions written for amphetamines that suppress appetite and lead to weight loss. To combat the rising tide of drug abuse, the Comprehensive Drug Abuse Prevention and Control Act was enacted in 1970 and replaced previous laws in this area. This act classified drugs into five schedules according to their abuse liability and provided a graded set of penalties for violation of regulations relating to the manufacture, sale, prescription, and record keeping of drugs of abuse. A summary of the abuse potential and examples of drugs falling under this act are provided in Table 55-5. This act is the major regulatory legislation controlling drugs of abuse (see Chapter 55).
In the early 1970s, cocaine was rediscovered as a recreational drug by the young, upwardly mobile, affluent generation. This second cocaine epidemic necessitated a redefinition of the picture of the typical drug abuser as an unemployed, minority male criminal. The 1993 National Household Survey on Drug Abuse reported that 70% of illicit drug abusers are employed, 80% are white, and 75% live in areas outside of the city.43 As of 2006, the characteristics of the typical drug abuser remain similar to those of 1993.44
The economic effect of these new patterns of abuse can be felt in hospital emergency departments and in board rooms across the United States. Although cocaine and methamphetamine abuse has generally declined since the 1980s, the incidence of cocaine-related and methamphetamine-related medical emergencies has increased threefold since 1981.6 This increase may reflect the increased toxicity of smokable drug preparations because smoking leads to a greater concentration of drug in the body than other routes of administration. Potential costs of illicit drug use in the workplace include payment for substance abuse treatment programs, loss of productivity from absenteeism, accidents, disability claims, theft, and employee screening for drug use. Among full-time workers, 43% reported that tests for illicit drug or alcohol use occurred at their place of employment during the hiring process; in the employed 18- to 64-year-old age group, 8% reported positive for an illicit drug in the previous month.37
In general the incidence of illicit drug use has declined modestly since 1975.31,32 In 1979, 51% of American high school seniors reported using marijuana annually; that figure decreased to 32% in 2007. Similar trends were reported for cocaine (6% in 1975 and 5% in 2007), hallucinogens (8% in 1975 and 5% in 2007), barbiturates and other sedative-hypnotics (10% in 1975 and 6% in 2007), heroin (1% in 1975 and 1% in 2007), inhalants (3% in 1976 and 4% in 2007), and amphetamines (16% in 1975 and 9% in 2001). There are some important exceptions to the decline in illicit drug use since the 1970s. Although overall amphetamine use has decreased, annual use of the smokable preparation of methamphetamine has increased from 1.5% in 1990 to a peak in 2004 (3.5%), followed by a decline to 1.7% in 2007. A noteworthy increase in MDMA use from trace levels in 1985 to 3.5% in 1995 to 4.5% in 2007 reflects the current upward trend in overall use of so-called “club drugs.” In addition, an emerging trend indicates that nonmedical use of prescription drugs such as clonazepam (Klonopin), methylphenidate (Ritalin), and oxycodone (OxyContin) is extremely prevalent with 15% of high school seniors reporting recreational use of at least one prescription medication within the past year.
DRUG ABUSE CHARACTERISTICS AND TERMINOLOGY
The term addiction refers to a compulsion to take a drug on a continuous or periodic basis to experience its psychoactive effects.4 For addiction to exist, the abuser must have a mental obsession to continue drug administration to produce pleasure. Additional characteristics of addiction, which may or may not be present, are dependence and tolerance. When the administration of a drug is discontinued or, in the case of certain drugs, significantly reduced, dependence leads to the appearance of a characteristic and specific group of symptoms, termed a withdrawal or abstinence syndrome.28 Tolerance exists when administration of the same dose of a drug has progressively less effect. This decreased response to the effects of a drug requires that increasingly larger doses of a drug be given to produce the same pharmacologic actions. The development of tolerance depends on the dose of the drug and the frequency of its administration. Tolerance is caused by compensatory responses that act to decrease the body’s response to a drug. The cellular basis for drug tolerance may be related to a decrease in receptors for the drug, a reduction in enzyme activity associated with signal transduction pathways, or other effects. Cross-tolerance is the phenomenon whereby chronic use of a drug produces tolerance to that drug’s effects and to other drugs that produce the same effect. Cross-tolerance may be observed among drugs of similar or different chemical types. A related but different phenomenon is cross-dependence, which refers to an ability of one drug to substitute for another drug, usually in the same class, in a dependent individual without precipitating a withdrawal syndrome.
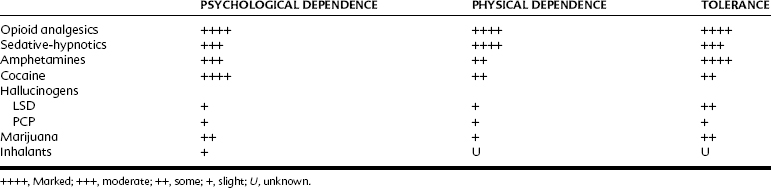
On the basis of common pharmacologic actions and of cross-tolerance and cross-dependence, the major drugs of abuse can be divided into distinct categories: opioid analgesics; general depressants of the CNS, including sedative-hypnotics and antianxiety drugs; cocaine, amphetamines, and related psychomotor stimulants; hallucinogens; marijuana; and inhalants. Table 51-1 lists the major abuse characteristics of these six drug groups—the degree of addiction and dependence and tolerance development commonly associated with the abuse of each drug group. In the following discussion, each drug group is described in terms of three major factors: (1) the pharmacologic effects produced by the drug group; (2) the abuse characteristics of the drug group, including addiction, tolerance, dependence, withdrawal, and other characteristics; and (3) the toxicity caused by the drug group and how it is treated.
ABUSE OF OPIOID ANALGESICS
Pharmacologic Effects
In the following discussion, the subjective effects of opioids are the effects observed in individuals who are opioid abusers. Although opioids produce similar pharmacologic effects in most individuals (see Chapter 20), not everyone reports the subjective effects of warmth, contentment, orgasm, and euphoria. In nonabusing individuals, the nausea and vomiting caused by opioids are construed as unpleasant and may obfuscate many of the reinforcing characteristics of these drugs. Many individuals view the mental clouding produced by opioids as an undesirable inability to concentrate, whereas addicts find this quality appealing. Most important, because opioids are the mainstay in the treatment of moderate-severe pain, it is relevant to know that in the therapeutic setting little substantive evidence suggests that effective pain management with opioids in individuals leads them to develop into opioid abusers.
Abuse Characteristics
Patients in need of pain control should not be denied adequate opioid medication because they show evidence of tolerance or exhibit withdrawal symptoms if the medication is stopped, as these signs do not indicate addiction. In addition, a patient who is in pain and receiving opioids does not respond the same way a psychologically dependent addict responds to opioids. Patients who are able to self-administer their opioid analgesic take the drug solely to reduce the pain, do not increase the dose greatly over time, and stop administration when the pain goes away.24
Toxicity
When the supply of an addict’s preferred drug is compromised, the addict may substitute substances of unknown content and potency or drugs thought to have a similar effect. Many addicts like the effects caused by IV injection of the agonist-antagonist pentazocine with the antihistamine tripelennamine. The talc contained in the crushed tripelennamine tablet has caused deaths as a result of lung emboli. Overdose leading to death may occur when an addict injects a purer sample than that to which he or she is accustomed or a sample containing a much more potent opioid, such as those seen with China white in the 1980s and fentanyl in the 1990s. Unexpected toxic effects also occurred in the late 1970s and early 1980s, when “bathtub chemists” trying to synthesize potent opioids produced a compound contaminated with 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP), which caused Parkinson-like symptoms in many young abusers (see Chapter 15). Abuse of prescription opioid analgesics has also resulted in unexpected deaths. In the late 1990s and early 2000s, deaths from overdosage resulted when individuals crushed tablets of the controlled-release formulation of oxycodone to make the entire dose available for intranasal or IV administration.
Opioid withdrawal or detoxification of heroin addicts or other opioid-dependent individuals can be managed with methadone because cross-dependence exists between it and other opioids.36,45 Because methadone and all other opioid analgesics act at opioid receptors, methadone can be substituted for the opioid being abused without precipitating a withdrawal syndrome. By substituting longer acting methadone for a short-acting opioid such as heroin, the addict is spared the undesirable effects of withdrawal because the opioid receptor remains occupied. Methadone can be withdrawn from the addict over weeks. Methadone, with its long duration of action, produces a protracted but tolerable withdrawal syndrome.
In 2000, Congress passed the Drug Addiction Treatment Act (DATA), allowing certified physicians to prescribe narcotic medications for the treatment of opioid addiction. DATA produced an important paradigm shift that allowed for the treatment of addiction to opioids such as heroin to occur in physicians’ offices, rather than limiting it to highly stigmatized government-regulated methadone clinics. Buprenorphine, an agent now being used under this new legislation, is a long-acting partial agonist that acts on the same receptors as heroin and morphine; it relieves opioid cravings in mildly to moderately addicted individuals and produces less respiratory depression and withdrawal symptoms than the full agonist methadone.21
ABUSE OF SEDATIVE-HYPNOTICS
Drugs in the sedative-hypnotic group are general CNS depressants and include sedative-hypnotic and antianxiety drugs (discussed in Chapter 13). Older sedative-hypnotic drugs, including barbiturates, glutethimide, and the widely abused but no longer approved drug methaqualone, have substantial abuse potential. Benzodiazepines and related drugs are now the most commonly used sedative-hypnotic and antianxiety drugs. Although these newer drugs have significant abuse potential, they are less frequently abused than the older sedative-hypnotic agents. Sedative-hypnotic drugs are readily available from illicit sources and by prescription abuse when large amounts of the drugs are accumulated by drug abusers visiting different prescribers.
Abuse Characteristics
The degree of addiction with sedative-hypnotic drugs depends on the dose of the drug, the frequency of administration, and the duration of drug use. Sedative-hypnotic drugs differ in onset and duration of action (short-acting and long-acting barbiturates and benzodiazepines are available). Addiction is most commonly associated with abuse of short-acting drugs, such as secobarbital, pentobarbital, oxazepam, and lorazepam. Dependence on longer acting agents, such as phenobarbital and chlordiazepoxide, is less common.3,22 Dependence occurs only rarely with intravenously administered ultrashort-acting sedative-hypnotics because they cannot be taken frequently enough to maintain adequate plasma concentrations.
For benzodiazepines, drugs with a higher affinity for the BZ2 benzodiazepine receptor subtype (e.g., alprazolam) seem to have a greater potential for abuse than drugs with a higher affinity for the BZ1 benzodiazepine receptor.30 Initial exposure to sedative-hypnotics may occur when the drug is prescribed to relieve anxiety or insomnia. The dose is slowly increased, and the abuser may become preoccupied with obtaining and using the drug. So-called date rape drugs, such as γ-hydroxybutyrate, a metabolite of γ-aminobutyric acid, and the prescription benzodiazepine flunitrazepam (“roofies”) are also subject to misuse. Both drugs have similar effects as sedative-hypnotics; however, their rapid oral absorption, onset of action, and ability to cause anterograde amnesia have resulted in their surreptitious use as sedatives to facilitate rape of unwitting individuals.
In contrast to opioids, sedative-hypnotics do not induce dependence unless increased doses of drugs are taken over a long period (≥1 month). The onset and severity of the abstinence syndrome also depend, in part, on the dose and the duration of drug use. Minimal withdrawal symptoms are elicited by abrupt withdrawal from chronic daily use of 400 to 500 mg of pentobarbital or secobarbital.20 With chronic use of larger doses, progressively more severe symptoms of withdrawal can be precipitated, even by abruptly reducing the accustomed dose by half. Although withdrawal from daily doses of 600 to 800 mg of secobarbital after 1 month produces a minor withdrawal syndrome, withdrawal from daily doses of 800 to 900 mg after 2 months or more produces major withdrawal symptoms. Another important determinant of the onset, severity, and duration of the withdrawal syndrome is the half-life of the specific drug. Drugs with relatively short half-lives (8 to 30 hours) tend to produce a severe withdrawal syndrome that develops quite rapidly. Drugs with longer half-lives (40 to 100 hours) produce a slower onset but less severe withdrawal syndrome of long duration.
The withdrawal syndrome after cessation of sedative-hypnotics resembles that seen after alcohol withdrawal. After a usually symptomless period (8 to 18 hours after the last dose), the individual exhibits increasing symptoms of anxiety, insomnia, agitation, and confusion. Anorexia, nausea and vomiting, sweating, and muscle weakness are also seen. Coarse tremors in the face and hands; dilation of the pupils; and increases in respiratory rate, heart rate, and blood pressure may occur. Orthostatic hypotension and syncope may also occur. These symptoms become more severe during the first 24 to 30 hours of drug withdrawal. By the third or fourth day, major manifestations of abstinence may develop, which include delirium, hallucinations, agitation, hyperthermia, convulsions, and nonspecific symptoms of anxiety. Symptoms associated with benzodiazepine withdrawal also occur; these are persistent tinnitus (≤8 months), muscle twitching, paresthesias, visual disturbances, and confusion and depersonalization.38 Reports of xerostomia and pain in the jaws and teeth have particular dental significance.8
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses